INTRODUCTION
Sarcopenia is a complex and serious geriatric syndrome in the life of the elderly triggering functional impairment and increasing the risk of falls, fractures and dependence. It has the potential to reduce quality of life leading to higher spending on health and increased mortality 1,2. Its prevalence can reach 5-13% in the elderly between 60-70 years and 11-50% in those over 80 years old depending on the criteria used for diagnosis 1. In Brazil in 2006, a prevalence of 15.4% was found among the elderly population living in São Paulo 3.
Currently sarcopenia can be diagnosed taking into account the reduction of muscle mass and function including the evaluation of strength and physical fitness 1,4. However, some studies have shown that the isolated use of the skeletal muscle mass (SMM) is an appropriate parameter in the identification of sarcopenia 5,6,7,8.
The evaluation of SMM can be carried out using methods such as computerized tomography, magnetic resonance imaging and dual-energy X-ray absorptiometry 2. However, the high cost and the use of radiation in such methods have limited their applicability in clinical practice 9. Therefore, bioelectrical impedance is increasingly used to evaluate sarcopenia due to its low cost, ease of use and absence of radiation as well as being a method that has been validated for the diagnosis of this syndrome 10. Given the consequences of sarcopenia and lack of research in the Brazilian population, especially those who are institutionalized, this study assesses the prevalence and factors associated with sarcopenia in long-term care facilities (LTCF) in the city of Salvador Bahia, Brazil.
METHODS
STUDY DESIGN
This cross-sectional study is part of a larger project entitled "Multidimensional evaluation of the elderly living in long-term care facilities in Salvador, Bahia", developed by the Aging-Related Research and Intervention Center (CEIAE) at the Nutrition School the Federal University of Bahia (ENUFBA).
Sample
The sample of the larger study was performed in three stages. In the first stage, was identified a total of 29 LTCFs which were located in 10 Health Districts of the 12 existing in the urban area. In the second stage, the number of elderly subjects by Health District that would participate in the study was determined. This number was proportional to the total elderly population living in each Health District, thus ensuring 80% power in representing the institutionalized elderly of the city. At a significance level of 5%, this number totaled 412 elderly subjects of both genders. In the third stage, LTCFs and elderly subjects were selected by simple random sampling. The final sample information available bioelectrical impedance and anthropometric measures was 216 elderly evaluated.
ELIGIBILITY CRITERIA
Those eligible to participate in the study were individuals of both sexes, aged over 60 years living in LTCF (public, philanthropic and private) located in the urban area of Salvador and who agreed to participate in the research.
Non-eligibility criteria for the examination of bioelectrical impedance were: limb amputation, presence of edema and/or ascites, cardiac defibrillator or pacemaker use and inability of weight measurement 11. Those who were unable to move and/or position themselves for gauging the anthropometric measures did not participate.
DATA COLLECTION
Data collection took place from November 2012 to October 2013 by a multidisciplinary team who had been previously trained to use standardized techniques.
Variables
OUTCOME
Sarcopenia was identified according to the SMI (SMM (kg) / height (m2) (6). The whole body SMM was estimated using the equation proposed by Janssen et al. 10 where SMM (kg) = ENT#091;(height in centimeters²/resistance of the bioelectrical impedance in ohms × 0.401) + (sex × 3.825) + (-0.071 × age in years)ENT#093; + 5,102. For this calculation, the values considered were 1 and 0 for male and female, respectively.
The resistance measurement was carried out by a tetrapolar body composition analyzer Biodynamics (BF-450 model). The pretest care protocol used was that proposed by Kyle et al. 11: fasting for at least four hours prior to emptying of the bladder, alcohol abstention for 48 hours before the test and no intensive physical activity in the last eight hours.
SMI was classified by the following cut-off points proposed by Janssen et al. 6: severe sarcopenia ≤ 8.5 kg/m², moderate sarcopenia 8.51-10.75 kg/m², normal muscle ≥ 10.76 kg/m² for men and severe sarcopenia ≤ 5.75 kg/m², moderate sarcopenia 5.76- 6.75 kg/m², normal muscle ≥ 6.76 kg/m² for women.
COVARIATES
Covariates measured were sex, age, time at the institutionalization, type of institution, body mass index (BMI) and functional capacity.
The BMI was classified according to the Nutrition Screening Initiative 12. Weight and height were obtained according to standards established by Jellife 13.
For the assessment of functional capacity the 'Activities of Daily Living' scale proposed by Mahoney and Barthel 14 was used and the cutoff points proposed by Azeredo and Matos 15 were adopted.
STATISTICAL ANALYSIS
The Kolmogorov-Smirnov test was used to analyze the data normality. Descriptive statistics were used (mean, standard deviation, median, interquartile range and percentile values), the Mann-Whitney tests, t student and Chi square Pearson test.
To investigate the relationship between sarcopenia and covariates, we used the Poisson regression model with robust variance, estimating the prevalence ratios and their respective confidence intervals at 95%. We opted for the multilevel modeling because of a possible clustering effect relating to the aggregation of individuals in institutions. Regression models were constructed by stepwise backward.
A 5% significance level was adopted for all analyses, which were carried out with the aid of the software STATA version 10.0 (STATA Corp, College Station, TX).
Ethical aspects
This project was approved by the Ethics Committee at ENUFBA (protocol number 11/2012). Prior authorization was sought from the LTCF and the elderly participants gave their informed consent using a signature or fingerprint. At the end of the study, the results from the evaluations were presented to the LTCFs in a report.
RESULTS
The population characteristics are shown in table I. It can be observed in table II that the average values of SMM and SMI were higher for males in all age groups. Comparing gender and age group, the average values of the SMI and SMM were lower in women who were 80 and older and men aged between 70 and 79 years. It is noteworthy that 75% of elderly men of all the age groups analyzed had some degree of sarcopenia (SMI < 10.76 kg/m²) (Table II).
Table I Characteristics of institutionalized elderly according to sex. Salvador Bahia

SMI: Skeletal muscle index; SMM: Skeletal muscle mass; BMI: Body mass index. Weight (kg), height (m), SMI (kg/m²) and the Barthel Scale Score are expressed as median (interquartile range). The other variables are expressed as mean (standard deviation). *Mann-Whitney test and t student test.
Table II Mean values, standard deviations, percentiles of the SMM and SMI of institutionalized elderly according to sex and age group. Salvador Bahia

SD: standard deviation; SMM: skeletal muscle mass; SMI: skeletal muscle index.
Most of the elderly people presented sarcopenia (72.2%) with the highest percentages observed among men (87.7%), in elderly people 60-69 years (77.3%), those who had been institutionalized for one to five years (75.8%). Those who resided in philanthropic LTCF (76.4%) showed thinness (92.4%) and moderate dependence (89%). Sarcopenia was associated only with sex (p = 0.006) and BMI (p < 0.001) (Table III).
Table III Prevalence, gross prevalence ratio and confidence intervals at 95% for association between sarcopenia and covariates in institutionalized elderly in Salvador Bahia
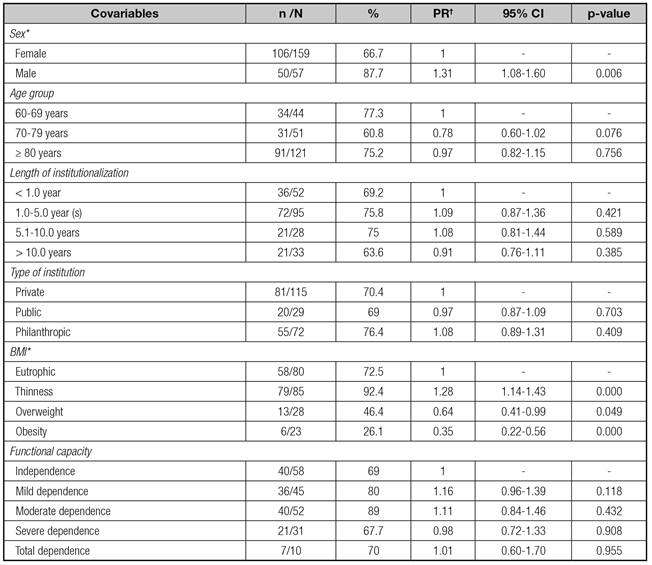
PR: prevalence ratio; CI: confidence interval; BMI: body mass index. *Statistically significant association by the Chi-square test (gender: p-value = 0.002; BMI: p-value = 0.001). †Poisson regression model with gross prevalence ratio for association between sarcopenia and other variables.
The gross prevalence ratio also showed a statistically significant association between sarcopenia and BMI with a prevalence of sarcopenia which was 28% higher among elderly people with thinness (PR = 1.28, 95% CI: 1.14 to 1.43) compared to normal and 31% higher in men (PR = 1.31, 95% CI: 1.08 to 1.60) when compared to women. For these elderly people overweight and obesity were demonstrated to be sarcopenia protection factors (Table III).
In table IV multivariate Poisson model can be seen. This considers the possible cluster effect due to the aggregation of the elderly in LTCF. In model 1, adjusted for all variables, only males (PR = 1.34, 95% CI: 1.10 to 1.65), thinness (PR = 1.38, 95% CI: 1.19 to 1 60) and obesity (PR = 0.38, 95% CI: 0.20 to 0.73) were significantly associated with sarcopenia.
Table IV Poisson regression model with adjusted prevalence ratio for association between sarcopenia and covariates in institutionalized elderly. Salvador Bahia
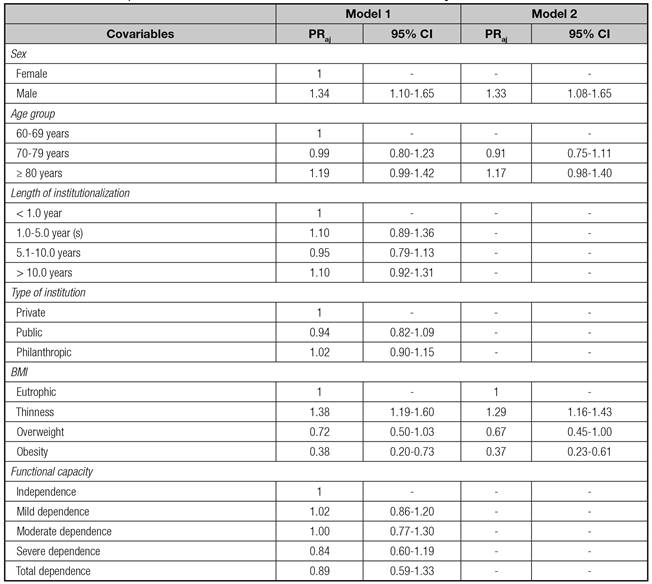
PRaj: adjusted prevalence ratio; CI: confidence interval; BMI: body mass index. Model 1: adjusted by gender, age, length of institutionalization, type of institution, BMI and functional capacity. Model 2: adjusted by gender, age and BMI.
In model 2, the same variables remained significantly associated with sarcopenia, adjusted for other variables in the model, with prevalences of 33% and 29% higher from sarcopenia, respectively, in the men (OR = 1.33, 95% CI: 1 , 08 to 1.65) compared to females, and thinness (PR = 1.29, 95% CI: 1.16 to 1.43) compared to normal weight. On the other hand, obese elderly people had a 63 % lower prevalence of sarcopenia (PR = 0.37, 95% CI: 0.23 to 0.61) compared to those with adequate nutritional status, revealing obesity to be a protective factor for sarcopenia.
DISCUSSION
The prevalence of sarcopenia in this population was high (72.2%) and higher than that found in studies of institutionalized elderly in other countries 16,17. This is probably a result of the different methods used in the studies and the different living conditions of such populations.
This result highlights the vulnerability of the elderly because sarcopenia can affect the quality of life, functional capacity, health and morbidity of this population 2.
More than half of the elderly men of all age groups showed SMI values below the recommended, or had some degree of sarcopenia. The findings of a higher prevalence of sarcopenia in men (87.7%), corroborate those of other studies with institutionalized elderly 18,19. Bahat et al. 18 who investigated elderly men in LTCF in Turkey reported a prevalence similar to that found in our study (85%).
Although the present study did not find an association between sarcopenia and type of institution, the high prevalence of sarcopenia found in philanthropic institutions justifies more research on the impact of the characteristics of these LTCF on the nutritional status of the elderly. The work of Camarano et al. 20 shows that most of the expenses of running Brazilian LTCF are on staff costs (52.5%) and only 14.1% is spent on food. Perhaps this is one reason for the impairment of the nutritional status these elderly people.
Malnutrition implies loss of muscle and fat and this is a major problem in the institutionalized elderly population 21 and this may explain the higher prevalence of sarcopenia found in the elderly with thinness in this study. Similar results have been found by other authors 16,17,22. On the other hand, the protective effect of obesity for sarcopenia, despite being considered a risk factor for comorbidities in the case of the elderly, has been linked to a lower risk of death, complications during hospitalization and the development of sarcopenia 8,23.
Physical inactivity, insulin resistance, chronic diseases, hormonal changes, inflammation and nutritional deficiencies (protein, calories, vitamin D and antioxidants) stand out as major causes of sarcopenia in the elderly 24. Therefore, better research on these factors may help to understand this reality.
The severity of the clinical and nutritional status, and functional impairment made it impossible to gauge the weight of many elderly people living in the LTCF investigated and that may have caused an underestimation of the prevalence of sarcopenia found. Although SMI has been used for the diagnosis of sarcopenia in this study, further research is required into the sensitivity of the isolated use of this index for this purpose.














