INTRODUCTION
During adolescence, a healthy diet is important because it affects wellbeing and health, and can reduce the risk of developing diseases or illnesses in adulthood; components such as these influence health related quality of life 1. Conversely, a poor diet quality or eating disturbances can contribute to an increased risk of obesity 2) and, consequently, can lead to risk factors such as heart disease and type 2 diabetes 3. An adolescent's eating behavior is the result of a myriad of influences 4. Multiple factors contribute to eating behaviors; these include family meals and dieting habits, weight status, and societal norms for thinness, which is related to body weight perceptions.
Adolescents are more likely to skip breakfast 5 and less likely to participate in family dinners 6,7, which may explain why adolescents are failing to meet dietary recommendations 8. The frequency of family meals has been associated with adolescents' health, including good nutritional intake 9 and promoting better outlook towards food and diet quality 10,11. On the other hand, the absence of family meals is related to a decreased diet quality, and unhealthy eating patterns 12.
Considering the existence of an eating transition from childhood to adolescence, which is characterized by changes in eating frequency, size portions, increased consumption of sugar sweetened beverages, calorie-dense, nutrient poor snacks and food away from home, it is expected that these eating behaviors have a relationship with weight status. A positive connection has been observed between eating and body mass index (BMI), as BMI predicted more restrained eating 13. Moreover, less frequent eating predicts gain in adiposity 14 and larger portion sizes of high-energy-dense foods are positively associated with BMI 15.
The body weight perception is a multidimensional concept that involves the self-perception of body size, feelings, beliefs and behaviors toward physical appearance 16. Because of the mass media influence and social and cultural norms, adolescents are constantly concerned about their body weight 17. The growing concern with body image has led many adolescents to change their eating habits, which can potentially be a serious threat on psychosocial development 18,19, nutritional status 17 and to the development of eating disturbances 20.
Therefore, this study aimed to analyze the connection between eating behaviors and family meals, body mass index and body weight perception on adolescents. Understanding the factors related to adolescents' eating behaviors is a valuable asset in matters of research, clinical practice and health promotion.
METHODS
PARTICIPANTS AND PROCEDURES
This is a cross-sectional study based on data from the Health Behavior in School-Aged Children (HBSC) Portuguese survey conducted in 2014 21. HBSC is a World Health Organization collaborative study that is conducted every four years in nationally representative, school-based samples 22. Over 40 countries participate in the study. HBSC examines a number of health behaviors and lifestyles and their context in young people.
The Portuguese HBSC 2014 survey included a representative sample of 6,026 adolescents (2,872 boys) from 125 public schools, with weighted distributions reflecting the distribution of Portuguese students in grades 6, 8, and 10. For the present study, only students from grades 8 and 10 were selected, because they had better awareness of eating behaviors and body weight; therefore, students from grade 6 were excluded (n = 2,157). In addition, 71 adolescents did not report weight and/or height, 87 did not report their body weight perception, 19 did not report their eating habits, and were removed from the sample. The result was a final sample size of 3,693 adolescents (1,723 boys), aged 14-17 years (mean = 12.6 ± 1.1).
The survey consists of a self-administered questionnaire that is completed in public schools. The schools were randomly selected from a national list, which had been stratified by administrative regions. A detailed description of the methods and instrument can be found elsewhere 23,24. The administration of the surveys was conducted according to standard guidelines from the HBSC survey protocol 23,24 and was carried out by trained teachers during class time. All school administrators, legal guardians, and students gave their written consent. Adolescents' participation in the study was voluntary, anonymous, and there were no incentives for participation. Research was conducted in accordance with both the Ethical Committee of the Oporto Medical School and the National Data Protection System.
MEASURES
Adolescents' socio-demographic characteristics included sex, school grade, age, and parents' education (a proxy for socioeconomic status). Adolescents' eating habits were assessed by asking "describe your eating habits, do you eat well?". Response options were "never or almost never", "sometimes" and "always or almost always". The first two response options were combined as "sometimes or rarely" and the third option was named "almost always". For the second section, adolescents were asked to report their eating practices, measuring unhealthy food consumption by stating if they overate, ate very little, ate only what was available, and if it was difficult to stop eating. The response options were similar to the previous questions. A general eating practice score was created based on six possible eating habit responses. It was considered that adolescents who answered at least once "sometimes or rarely" did not have good eating practices and that the others did. Combining the adolescents' eating habits and their general eating practice score generated a new variable that was computed. This lead to the creation of four eating behavior profiles: a) realistic negative were those who did not have good eating practice and reported not having good eating habits; b) underestimators were those who had good eating practice, but reported not having good eating habits; c) overestimators were those who did not have good eating practice, but reported having good eating habits; and d) realistic positive were those with good eating practice and reported having good eating habits.
The actual weight (to the nearest 0.5 kg) and height (to the nearest 0.5 cm) were also self-reported. Body mass index (BMI) was then calculated based on mass (kilograms) divided by height (m2). Adolescents were placed into normal weight, overweight, and obese categories according to age- and sex-specific cut-off points proposed by the World Health Organization 25. The group of adolescents categorized as underweight was small, and that is the reason why this category was removed from the analysis and these adolescents were added into the normal weight category.
Body size perception was assessed by asking adolescents, "do you think your body is...?", with the response options "too thin", "a bit too thin", "about the right size", "a bit too fat", and "too fat", which were combined to be perceived as underweight ("too thin" and "a bit too thin"), normal weight and overweight ("a bit too fat", and "too fat"), respectively.
DATA ANALYSIS
Descriptive statistics are presented as means and standard deviation or percentages. Bivariate analysis between eating habits and eating practices were tested by Chi-squared or Fisher's exact test. The relationship between family meals, BMI categories and body weight perception with adolescents' profiles according to their eating habits and eating practices were tested by Chi-squared. Then, multiple binary logistic regressions were used to assess the extent to which factors were associated with each of the four adolescents' eating behaviors profile. Analyses were adjusted based on sex, age, and parents' education. Data analysis was performed using SPSS version 22, and the level of significance was set at 0.05.
RESULTS
Adolescents' characteristics are presented in Table I. Most adolescents had a normal weight (78%), but it is important to note that 22% were overweight or obese. However, only 49.9% classified themselves as normal weight. The majority of adolescents reported good eating habits as "almost always" (71.5%). Almost one quarter (24.4%) of adolescents misperceived their weight status (data not shown).
The relationship between eating habits and eating practices is represented in Table II. Picking the response "almost always" concerning good eating habits was related to eating unhealthy food (χ2[1] = 5.252, p = 0.022) and eating very little (χ2[1] = 47.347, p < 0.001) less often.
Table II. Relationship between self-report eating habits and eating practices
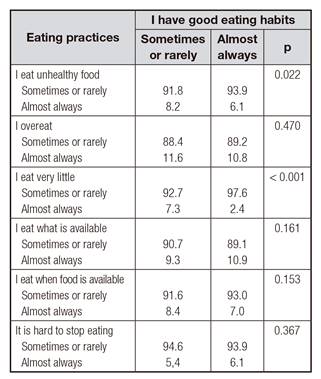
Tested by Chi-squared or Fisher's exact test.
The cross-tabulation between eating habits and eating practices was shown in Table III. Those who "almost always" had good eating habits and good eating practices were classified as realistic positive (51.6%). In opposition, those who had good eating habits "sometimes or rarely" and did not have good eating practices were classified as realistic negative (9.6%). These two groups of adolescents were aware of their eating behaviors. On the other hand, 19.9% of the adolescents reported having good eating habits "almost always" but did not have good eating practices, and as such, they were classified as overestimators. Finally, there were 18.9% of adolescents classified as underestimators, who had good eating practices but stated that they had good eating habits only "sometimes or rarely".
Table III. Adolescents eating behaviors profile

*General eating practice was calculated based on six items of self-report eating practices. Those who reported "sometimes or rarely" in all self-report eating practices were considered to have good eating practices.
The adolescents' eating behaviors profiles were related to family meals, BMI category and body weight perception. The results can be seen in Table IV. Realistic positives and overestimators accounted for the higher proportion that had breakfast (χ2[6] = 133.711, p < 0.001) and dinner with their families (χ2[6] = 53.230, p < 0.001). The percentage of normal weight (χ2[3] = 18.603, p < 0.001) and perception of being normal weight (χ2[6] = 152.624, p < 0.001) were significantly higher among realistic positives and overestimators.
Table IV. Relationship between adolescents eating behaviors profile with family meals, body mass index and body weight perception

BMI: body mass index. Tested by Chi-squared.
Results of the binary logistic regression analysis for the associations between adolescents' eating behaviors profile with family meals, BMI and body weight perception are shown in Table V. Having breakfast with family several times a week (OR = 1.42, 95% CI: 1.20-1.68, p < 0.001) or every day (OR = 1.64, 95% CI: 1.37-1.97, p < 0.001), and having a normal weight (OR = 1.74, 95% CI: 1.41-2.14, p < 0.001) were positively associated with being classified as realistic positive. On the contrary, realistic negatives were less likely to have breakfast with family several times a week (OR = 0.57, 95% CI: 0.43-0.75, p < 0.001) or every day (OR = 0.48, 95% CI: 0.34-0.67, p < 0.001), and have normal weight (OR = 0.40, 95% CI: 0.29-0.56, p < 0.001).
Table V. Binary logistic regression model of meals with family, body mass index, body weight perception and adolescents' eating behavior

OR: odds ratio; CI: confidence interval; BMI: body mass index. Analysis were adjusted for sex, age, and father and mother education. *p < 0.05, †p < 0.01, ‡p < 0.001.
DISCUSSION
The purpose of this study was to analyze the relationship between perception of quality of eating behaviors, and family meals, body mass index and body weight perception on adolescents. There are several aspects of this study to highlight. First, having breakfast with family more often and being of normal weight were positively related with being classified as realistic positive (having good eating practices and being aware of them). On the other hand, having breakfast with family often and being of normal weight were negatively associated with being realistic negative (not having good eating practices and being aware of it). Second, adolescents classified as having good eating habits also reported eating unhealthy food and eating very little less often. Third, most adolescents were aware of their eating behaviors, but 38.8% misjudged their diet either positively or negatively.
The findings of this study confirm that family meals, essentially breakfast, are associated with adolescents' better eating behaviors, as previously observed in other studies 9,10. Findings are also consistent with research regarding the inverse relationship between family meal frequency and unhealthy eating patterns 12,26. This relationship might be due to the fact that family, mainly parents, influence their children's eating behavior by actively making food choices for the family (such as higher intake of fruit, whole grains, and fiber), serving as models for dietary choices and patterns, and using feeding practices to reinforce the development of healthy eating patterns and behaviors that they believe to be appropriate 9,27. Other than the benefits related with adolescents' dietary intake, breakfast consumption with family is also essential in obesity prevention, because those who have it are less likely to be overweight/obese 9,28,29. Therefore, breakfast consumption with family should be encouraged as a mean to promote adolescents' better eating behaviors, and prevent obesity. This is particularly important nowadays because adolescents are more likely to skip breakfast 5.
Dinner with family was not associated with adolescents' eating behaviors, as observed previously 9,30. However, these results were different from others in which eating dinner with the family was associated with healthy dietary intake patterns 6,31. More studies on how family dinner impact adolescents' eating behaviors should be done to better understand the discrepancy of these studies. Nonetheless, family dinners seem to be more than just a meal time: they promote better family connections and are a protective factor that may help reduce high-risk behaviors among youth (i.e., substance use, sexual activity, depression/suicide, antisocial behaviors, violence, school problems, and excessive weight loss), especially if the family maintains good communication 32,33.
Although it was expected that eating behaviors would have a relationship with weight status 13,14,15, it was only verified in bivariate analysis. The proportion of normal weight among those who had healthy eating behaviors (realistic positive) was significantly higher than among those with unhealthy eating behaviors (realistic negative). In binary logistic regressions the analysis did not show any link between the two variables. Once body weight perception was related to adolescents' eating behavior in bivariate analysis and in binary logistic regressions analysis, even when adjusted for potential confounders (sex, age, and father and mother education), it appears that perceptions are very important to predict behavior. Studies indicated that body weight perception influences eating behaviors, such as food restriction, and the use of pharmaceutical drugs that promote weight loss 20,34. This indicated that adolescents are very concerned about body image 17 and that they establish a link between body weight perception and eating behaviors 19,20,34. Thus, this explained why adolescents that had a better eating behavior were more likely to perceive themselves as having a normal weight and, on the contrary, those who had worse eating behaviors or even those who perceive having good eating habits only sometimes or rarely (underestimators) were less likely of being normal weight. These findings made it possible to conclude that awareness and perception of not having good eating behavior is related to body weight perception 35.
Although it was not directly related with this study's aims, it is noteworthy that 38.8% of the teenagers were not aware of their eating behaviors. This leads to the topic of food literacy. This is a relatively new concept that is described as the capacity of an individual to understand basic information about nutrition and food as well as the competence to use that information in order to make appropriate health decisions 36. Food literacy seems to influence adolescents' eating behaviors, as adolescents with greater food knowledge are shown to have healthier practices 37,38,39. As a result, it is essential that public health promotion and interventions should focus on health and food literacy during adolescence.
Some limitations and strengths should be noted. First, the cross-sectional design of the study precludes any inference about causality. Second, self-report eating habits and practices might introduce recall bias. However, self-report is appropriate for population-based studies or those with epidemiological characteristics, since they are easy to use and inexpensive. Third, height and weight were self-reported and are subject to bias. Nevertheless, self-reporting weight and height is considered as a valid tool for BMI estimates in epidemiological studies 40. Furthermore, the eating information did not contain nutrition information. The strengths of the study include the representative sample of adolescents, which allows generalization of the Portuguese adolescent population, and the fact that the study follows a rigorous methodological procedure in line with the demands of a large scale cross-European recognized study.
Adolescents' eating behaviors are related to family meals, and body weight perception. Having breakfast with family more often and being normal weight were positively related to adolescents' awareness of good eating behaviors. An understanding of the factors that influence eating behaviors during adolescence is needed to improve the dietary patterns and health status of this age group, mainly due to the higher prevalence of overweight and obesity among adolescents 41,42.















