INTRODUCTION
In emergencies or in situations involving critically ill patients, the accurate calculation of body weight is essential to ensure adequate medical care (1). Indeed, weight is not only associated with the patient's nutritional status, but also forms a basis on which to calculate intravenous fluid volumes and drug doses, as well as on which to determine the dimensions of the equipment used in resuscitation (1,2). In no other patient population is there a greater need to calculate and manipulate these doses than in the paediatric population. Therefore, recording the patient's correct weight plays a crucial role in minimizing drug dosage errors (3).
Simple techniques are generally used to determine weight (3). In some circumstances, however, an anthropometric evaluation is impossible and other people able to supply the necessary information are not always present. In critical and/or bedridden patients, these measurements are rarely taken in view of the difficulty involved in applying the conventional methods of determining the correct weight. Attempting to estimate weight solely by visual observation is a practice that is not recommended and that may result in serious errors in drug administration (4).
Various tools aimed at enabling weight to be estimated quickly have been proposed in the literature. The most commonly used methods are based on the age or the length of the patient. Based on the patient's age are methods such as APLS (Advanced Paediatric Life Support), Best Guess, and those adapted by Luscombe and Owens. The Broselow tape proposed in the Pediatric Advanced Life Support (PALS) manual (5 6 7-8) is an example of a method based on length. In a review of the literature on this subject, Young and Korotzer argued that the ideal method of estimating weight should be precise, reliable, quickly obtainable, simple to use, and readily available to healthcare professionals (9).
Several studies comparing weight estimation methods have been published, with results varying as a function of the different populations and ethnic groups evaluated (2,4,10,11). A study conducted in hospitalized paediatric patients in Australia compared measured weight with the weight estimated using different equations. The methods that proved most accurate in that study population were the APLS Update for patients under 12 months of age, and the Best Guess for those over a year old (10).
A review of the literature showed that few studies have been conducted to evaluate the precision of these weight estimation methods in the Brazilian paediatric population. The objective of the present study was to evaluate these weight estimation methods, comparing estimated weight with measured weight in children and adolescents receiving care at a Brazilian reference hospital.
MATERIALS AND METHODS
STUDY DESIGN AND SITE
This observational study was performed in a paediatric clinic at the Instituto de Medicina Integral Professor Fernando Figueira (IMIP) between August 2016 and January 2017. IMIP, situated in the Brazilian state of Pernambuco, is a philanthropic quaternary hospital dedicated exclusively to the care of patients within the public healthcare system. With 1,066 beds, the hospital includes 214 paediatric beds and 6 intensive care units (ICUs), 2 of which are paediatric. During the data collection period of this study, 900 paediatric patients on average were admitted to this hospital each month.
POPULATION & STUDY SAMPLE
Data were collected from hospitalized patients of both sexes under 14 years of age, who were able to walk and/or on whom it was possible to take their anthropometric measurements. Patients with encephalopathy, amputees or patients whose limbs were disproportional, those with genetic syndromes, oedematous patients, and any who had been included in the study previously (readmissions to hospital) were excluded from the study.
DATA COLLECTION
Following an interview and after the informed consent had been obtained from the parents/guardians or from the child itself, anthropometric measurements were performed in accordance with the techniques recommended by the World Health Organization (WHO) (12,13). Measurements were taken in duplicate, sequentially, by the same investigator, using standardized procedures. In the analysis, in order to maximize quality control, thus improving reliability and accuracy, the mean value of the two measurements was used as the measured weight.
Weight was measured using a digital electronic scale (Welmy, Brazil) and length/height was measured using an infantometer (Welmy, Brazil) for children two years of age or under, and a stadiometer (Tonelli, Brazil) for those over two years of age.
Ethnicity was self-reported by each individual and the overall sample was then dichotomized into white or non-white.
Weight was estimated using the following formulae:
A version of the Broselow tape produced by PediaTape was used. This version is based on the combined data obtained from the databases of the 2007 National Health and Nutrition Examination Survey (NHANES) in the United States. The tape is divided into colour zones that estimate the patient's weight in accordance with his/her length. To perform the estimation, the patient lies down, barefoot, with his/her arms extended along their body and with their legs stretched out. According to the manufacturer's recommendations, the tape was applied to paediatric patients of up to 144 cm in length and/or 37 kg. In the case of obese individuals, it is recommended that the estimated weight should correspond to the next higher colour zone. Estimated weight for the later analysis of agreement was defined as the mean point on each color-coded range of weight.
DATA ANALYSIS
The STATA software program, version SE12.0, and Excel 2010 were used to store, process and analyse the data. The Anthro and the Anthro Plus software program was used to calculate the z-scores in accordance with the criteria proposed by the WHO (12,13). Patients whose BMI-for-age z-score was between -2 and +2 were considered to be well nourished.
Student's t-test for paired samples was used to compare the mean measured weight with the mean weight estimated by each method. A significance level of 5 % was established for the tests applied.
The Bland-Altman method (14) and Lin's concordance correlation coefficient (15) were used to analyse concordance. The Bland-Altman method generates graphs that show the average value of measured and estimated weight on the horizontal axis, and the differences between them on the vertical axis. This technique provides the bias, precision (standard deviation [SD] of the bias) and the limits of concordance according to the 95 % confidence interval (95 % CI) (bias ± 1.96 SD). A positive bias indicates underestimation by the method, while a negative bias indicates overestimation.
As proposed by McBride, Lin's concordance correlation coefficient should be interpreted according to the position of the lower limit of the 95 % CI for this coefficient as follows: < 0.90 = poor; 0.90-0.95 = moderate; 0.95-0.99 = good; and > 0.99 = excellent (15).
The concordance tests were initially applied to the entire sample and subsequently to groups classified according to nutritional status, bearing in mind that one of the methods, the Broselow tape, requires a different estimation to be used for obese patients. However, considering the small percentage of dystrophic patients in the sample, and in order to preserve the pre-established criteria equally for each method, it was decided to present the results obtained only from the group of well-nourished patients.
ETHICAL ISSUES
The internal review board of IMIP approved the study protocol under reference CAAE 51877115.0.0000.5201. Patients were admitted to the study following authorization from their parents or guardians, who were required to sign an informed consent form. In addition, participants of 8 years of age or more were asked to sign an assent form.
RESULTS
PARTICIPANTS
During the data collection period, 465 hospitalized patients fulfilled the eligibility criteria. Of these, 19 (4.1 %) refused to participate or did not agree to have their anthropometric measurements taken for the study. Therefore, the final sample consisted of the 446 individuals whose clinical and sociodemographic data are described in table I. Most of the included children and adolescents (58.1 %) were male, of 1-5 years of age (43 %), and well nourished (85 %).
MEASURED AND ESTIMATED WEIGHT
The mean measured weight of all the patients evaluated was 21.8 kg (± 13.8 kg). The means and standard deviations for each weight estimation method according to age group, sex, and ethnicity are described in table II. For children under 12 months of age, there were no statistically significant differences between the means of measured weight and estimated weight according to the APLS Update and Best Guess (p = 0.183 and p = 0.140, respectively). For patients of 1-5 years of age, there were no statistically significant differences between the means of measured and estimated weight with APLS Update (p = 0.200); however, the differences found with the Luscombe and Owens and Best Guess methods were statistically significant (p < 0.001). In the case of the children over five years of age, statistically significant differences were found between measured and estimated weight (p < 0.001) for all of the methods evaluated. The Broselow tape was not included in this analysis because it does not take age into account when estimating weight. The Broselow tape was applied to 383 patients whose length was within the limit of its extension (144 cm), and in 61 % of cases the measured weight was in agreement with the weight range estimated by the tape.
Table II. Mean measured versus mean estimated weight as calculated by the different methods evaluated in paediatric patients admitted to a clinical ward, according to age group, sex, and ethnicity. IMIP, August 2016 - January 2017

Weight is expressed in kg, as mean ± SD.
*p-value obtained using the t-test for paired samples.
†A p-value greater than the significance level indicates that measurements tend to be the same with both methods.
Figures 1, 2 and 3 are graphic representations of the Bland-Altman plot analysis. In the group of patients under 12 months of age, the bias was minimal both with the APLS Update and with the Best Guess, although the concordance limits indicated a considerable difference between measured weight and the weight estimated by each method for this age group (95 % CI: -1.9 to 2.1; 95 % CI: -2.3 to 1.5, respectively), as shown in table III.
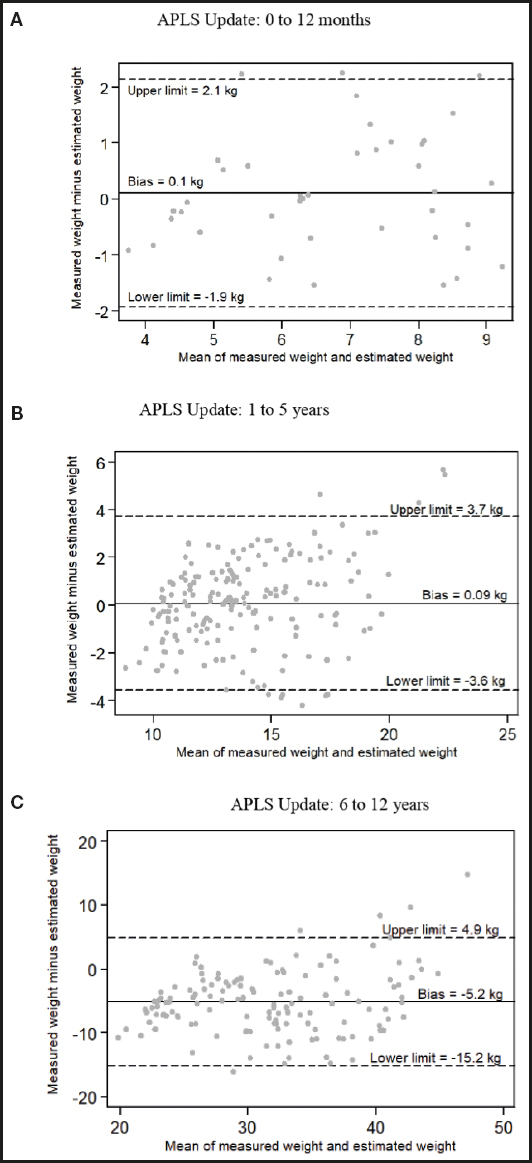
Figure 1. Bland-Altman plot showing the difference between measured and estimated weight as calculated by the APLS Update method in well-nourished patients. A. Weight = (0.5 x age in months) + 4; B. Weight = (2 x age in years) + 8; C. Weight = (3 x age in years) + 7. The continuous line indicates the bias and the dotted lines indicate the limits of concordance. IMIP, August 2016 to January 2017.
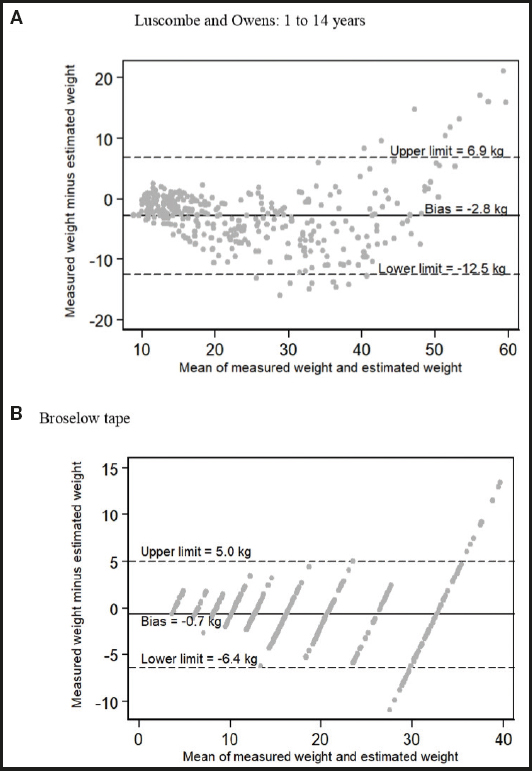
Figure 2. Bland-Altman plot showing the difference between measured and estimated weight as calculated by the Luscombe and Owens method [A) weight = (3 x age in years) + 7] and by the Broselow tape in well-nourished patients (B).The continuous line indicates the bias and the dotted lines indicate the limits of concordance. IMIP, August 2016 to January 2017.

Figure 3. Bland-Altman plot showing the difference between measured and estimated weight as calculated by the Best Guess method in well-nourished patients. A. Weight = (age in months + 9)/2; B. Weight = 2 (age in years + 5); C. Weight = 4 x age in years. The continuous line indicates the bias and the dotted lines indicate the limits of concordance. IMIP, August 2016 to January 2017.
Table III. Agreement between measured and estimated weight according to method and respective criteria in paediatric well-nourished patients admitted to a clinical ward. IMIP, August 2106 - January 2017
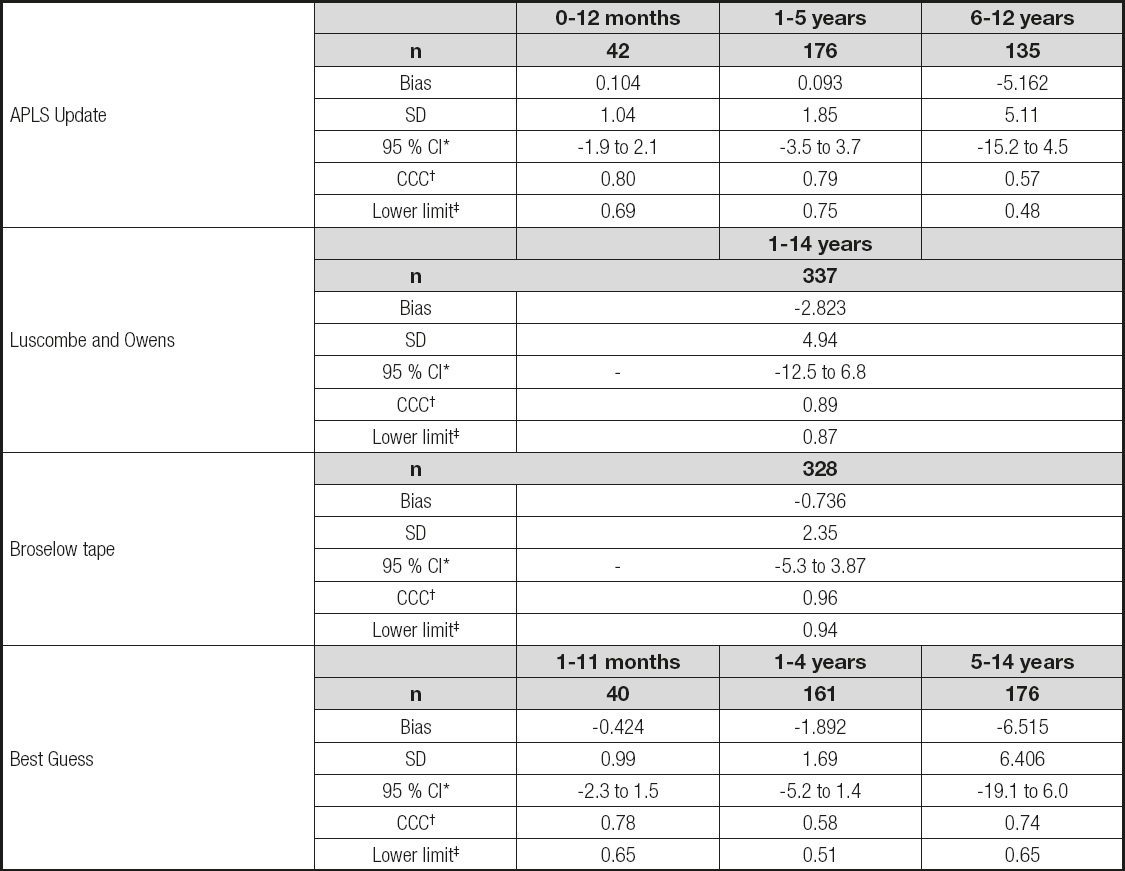
*95 % confidence interval. †CCC: Lin's concordance correlation coefficient (14).
‡Lower limit of the 95 % confidence interval of the reliability of Lin's concordance correlation coefficient: < 0.90 = poor; 0.90-0.95 = moderate; 0.95-0.99 = good; > 0.99 = excellent (15).
Lin's concordance correlation coefficient was also applied to the sample and the values found are shown in table III. Concordance was best with the Broselow tape, with a coefficient of 0.96 and a lower limit of 0.94, considered a moderate correlation.
DISCUSSION
Although weight estimation methods are widely used worldwide in paediatric emergency departments, to the best of our knowledge no studies have been published to validate their use in the Brazilian population. The agreement between the age-based weight estimation method and the measured weight of the children and adolescents in the present study was not good. In general, agreement was poorest when the method proposed by Luscombe and Owens was used. On the other hand, the Broselow tape, which is based on patient length, was the method in which the estimated weight was closest to the patient's measured weight. The performance of the methods deteriorated as the age of the participants in the study increased.
In the case of patients under 12 months of age, the results obtained with the method proposed by the APLS Update and by Best Guess were satisfactory in that the mean measured weight was similar to the mean estimated weight. Similar findings were reported from a study involving around 30,000 patients at the Children's Hospital at Westmead, a tertiary hospital in Australia (10), with the APLS Update proving even more specific than the Best Guess (a difference between means of 0.5 kg and 0.9 kg) (10). Flannigan et al. retrospectively evaluated around 10,000 patients in the United Kingdom and also found that the APLS Update gave a more accurate estimation of weight for patients under 12 months of age (p = 0.189) (16).
For the group of patients of 1-5 years of age in the present study, agreement was best with the APLS Update, with only 0.2 kg of difference between measured and estimated mean weight. The APLS Update introduced three new methods for three different age groups instead of using one single method for all ages, as previously recommended (5). Results have shown that agreement is more satisfactory with the new version compared to the previous one, particularly in patients under five years of age (9,10).
As age increased, statistically significant differences began to appear between measured and estimated weight when using these mathematical methods (17). In a study conducted by Chavez et al. to evaluate the effectiveness of four weight estimation methods in 324 patients at a paediatric emergency department in Florida, USA, the difference between mean weights was also found to be directly proportional to the age of the individual (18). This finding agrees with the results from other studies showing that the methods that are based exclusively on patient age do not appear to be sufficiently accurate to enable their widespread use in paediatric emergency departments (1,4,9,16,19).
The percentage of participants in the present study whose weight was correctly estimated using the Broselow tape is close to that reported by Mishra et al., who evaluated around 500 children of up to ten years of age receiving outpatient care at a hospital in India (20). Agreement was found between measured and estimated weight according to the colour zone proposed by the tape in 63.2 % of the sample (20). These results are more satisfactory than those obtained by other studies, in which the mean percentage of accuracy was below 50 % (10,16,18,21).
The analyses of concordance evaluated using the Bland-Altman plot technique in well-nourished patients showed that, although in some groups there was a minimum bias that was directly proportional to an increase in age, there is an important dispersion in the values, and the limit of the differences was unacceptable. In the patients under 12 months of age, for example, although the bias was small, the limit of the difference between means is of approximately two kilograms, both in the group whose weight was estimated using the APLS Update and in that in which Best Guess was used. In our opinion, an error of two kilograms in patients who are only months old would correspond to a significant percentage of their body weight and could cause serious errors in their clinical management.
Lin's concordance correlation coefficient was also used, and its results reinforce those found with the Bland-Altman plots, in which agreement with measured weight, considered the gold standard, is poor with all the age-based methods. The imprecision of these methods was recently described by Wells et al. (19), who evaluated 28 estimation methods in a sample of around 1,000 children aged from one month to sixteen years admitted to four different paediatric emergency departments in Johannesburg, South Africa. None of the mathematical methods analysed presented satisfactory statistical results that would justify their use in that study population. To draw their conclusion, those authors also took studies conducted to validate these methods into consideration, reporting on the performance of each one in the published paper (20).
The results obtained with the Broselow tape, nevertheless, were best when compared to the mathematical methods, confirming that the effectiveness of the length-based method is better than the effectiveness of those approaches that take only age into consideration (4,9,16,21 22-23). This finding agrees with the results reported by Geduld et al., who compared weight estimation methods in approximately 2,000 children. In that sample, agreement with measured weight was better when the Broselow tape was used (0.9 % of difference between mean measurements) when compared to Best Guess and the methods proposed by Luscombe and Owens, which tended to overestimate weight by 15.4 % and 12.4 %, respectively (24).
Illnesses and hospitalization can result in weight loss, and this could be considered a limitation of the present study. Nevertheless, it was decided that the weight estimation methods should be applied under the actual circumstances in which they would need to be used, i.e., that the study should be performed in a sample of hospitalized patients. Another limitation of the study refers to the fact that the methods analysed here were instituted based on data from populations with different ethnic and anthropometric characteristics when compared to those of this sample. On the other hand, with the objective of identifying possible variations in the performance of the methods assessed, the sample was stratified according to patient nutritional status, evaluated in accordance with the WHO parameters.
Age-based weight estimation methods are imprecise, since the weight of children and adolescents is affected by various other factors in addition to age (1,9,25). In the present sample only the Broselow tape yielded satisfactory results when compared to the other methods evaluated. The age-based methods used were not accurate enough, and their use in this population cannot be endorsed. In this respect, whenever it is impossible to assess weight by the conventional method, and parents are absent or unable to supply this information, the use of weight estimation methods based on patient length is recommended.















