BACKGROUND
The World Health Organization (WHO) defines obesity as a body mass index (BMI) greater than 30 kg/m2 in adults (1). Overweight and obesity in children are present when BMI is above the age- and sex-specific cut-off point established by the International Obesity Task Force (IOTF). In recent years the prevalence of obesity in infants, children and adolescents has increased alarmingly (2). Obesity can affect health, educational outcomes and quality of life (3). If current trends continue, 70 million obese children are expected by 2025 in the developed world (4).
Studies have described the consequences of obesity on children's health. With respect to cardiovascular outcomes there is a higher risk of hypertension, dyslipidemia, metabolic syndrome (5,6), glucose intolerance, and insulin resistance among children with obesity than among those with an appropriate body weight (7,8). From a psychological perspective children with obesity have lower levels of self-esteem (9,10), often as a consequence of school bullying, which can increase the risk of anxiety, depression, attention deficit, hyperactivity, and sleep disorders (11-13).
These factors can contribute negatively to a child's perceived quality of life, which may explain the lower scores obtained in specific questionnaires (14-16). The WHO defines quality of life as "the individual's perception of their situation in life, within the cultural context and values in which they live, and in relation to their objectives, expectations, values and interests" (17). The concept of health-related quality of life (HRQoL) has been specified relatively recently.
Diverse instruments can be used to address HRQoL by assessing all the dimensionsthat may play a role. One such instrument is the SF-36 questionnaire, which was developed in the United States in 1992 for the Medical Results Study (MOS) (18). This questionnaire, for use with persons aged over 18 years, is composed of 36 items that assess positive and negative health states, grouped within eight dimensions: physical function, physical role, body pain, general health, vitality, social function, emotional role, and mental health (18,19). Subsequently, the best question from each of the facets was selected, obtaining the WHOQOL-BREF, which produces a quality of life profile covering four areas: physical, psychological, social relations, and environment (19). This test has a short version for application to children aged between 5 and 14 years, known as the SF-10 (20). The latter test was applied in our study.
One of the fundamental approaches employed in the prevention and reduction of childhood obesity is through sports programs. Studies have confirmed that intervention with physical activity can improve the quality of life of children with overweight or obesity (21). Regular sports activities significantly reduce body fat, especially in the legs and trunk, and increase bone mineral density (22,23). If this physical activity is accompanied by compliance with nutritional recommendations, the results may be further improved (24). The aim of the present study was to determine whether a program incorporating physical activity and nutritional recommendations may improve HRQoL in children with overweight or obesity.
MATERIAL AND METHODS
The design employed in this study was that of an open-label randomized clinical trial. It was carried out in Granada (Spain). Sample recruitment took place at the pediatric consultations of 12 health centers and at the endocrinology consultations of the Hospital Complex of Granada. In all cases the informed consent of the child's parents or tutor was obtained for participation in the trial. This study is registered at www.clinicaltrials.gov (identifier NCT02779647). The research respects the risk of bias criteria (according to GRADE): it presents information on the tests performed, the key statistical results, and the rating of the quality of the tests for each result.
Based on results from previous studies in overweight children, Carrel A et al. (25) found a decrease in body fat of 4.1 ± 3.4 % in the group of children who performed the intervention with physical exercise, compared to 1.9 ± 2.3 % in the control group. Considering that in our study similar results will be obtained, to achieve a power of 80 % to detect differences in the contrast of the null hypothesis H0: -1-2 by means of a bilateral Student's T-test for two independent samples, taking into account that the significance level is 5 %, it will be necessary to include 27 children in each group. The randomization technique used the Microsoft Excel™ random number generator.
Overweight and obesity are defined as being present when the body mass index (BMI, calculated as weight/height2 [kg/m2]) exceeds the corresponding cut-off point (according to age and sex) stipulated by the IOTF. Thus, for boys with an average age of 10.65 years, as was the case in our study sample, overweight is present when BMI is between 20.20 and 24.57, and obesity when BMI exceeds 24.57. For girls of the same age, overweight is present when BMI is between 22.30 and 24.77, and obesity when BMI exceeds 24.77 (2).
The intervention program consisted of physical activity based on games, with four 90-minute sessions per week, for nine months (corresponding to the school year). Attendance at all sessions was recommended and was mandatory for at least two sessions per week. This measure was adopted to provide flexibility to families who had difficulty in attending all the sessions provided. In addition, theoretical-practical sessions of nutritional advice were given twice monthly to the children and their families. The SG performed the physical activity and received nutritional advice, while the CG only had the theoretical-practical sessions on nutrition. This study carried out a health campaign using focus groups to increase parents' awareness of childhood obesity and dispel myths around children's weight.
The physical activity consisted of playful, non-competitive sessions, since the main objective was that the children should enjoy themselves. All the sessions were structured in three parts: warm-up, main part, and cooling off. Taking into account the needs of the study population, 5 minutes' rest was allowed for every 30 of activity, to enable hydration. The main part of the exercise was based on the practice of popular games and sports, as well as alternative sports, all of which had an aerobic component and did not involve strenuous jumping. In the initial weeks of the program all the sessions were controlled by the sports technical staff, although the children could then choose the games they wanted to play. Thus, a learning period of different games and sports was established, and the children decided which activities were most enjoyable, which encouraged their participation in, and their adherence to the program.
The clinical history obtained was composed of each child's personal data, family history, sociodemographic data, and nutritional assessment.
All the analyses were carried out by the researchers, and calibrated by an anthropometric technician (kappa coefficient > 0-80). Height was measured with a Seca 222 stadiometer (Seca Deutschland®, Germany) with a sensitivity of 0.1 cm; body weight was evaluated with an electronic scale, previously calibrated, with a sensitivity of up to 0.1 kg (KERN MBP 12K5BM Version 1.1®, Germany). The anthropometric examination was performed with the following measurements and indices: weight, height, upper arm circumference (on the left or non-dominant arm), skin folds (left triceps and subscapular on the non-dominant side), and waist-hip circumferences following the indications provided by the Spanish Pediatrics Association (26). A Harpenden caliper (British Indicators, Ltd.®, London) with a sensitivity of 0.1 mm and a constant pressure of 10 mm2 was used.
The body composition of the children was determined by measuring bioelectrical impedance using an inBody 720 apparatus. This method enables the researcher to determine body composition by measuring and quantifying the content of water, proteins, body fat, and minerals in the body (7). The measurement method was standardized according to the Lukaski protocol (27); likewise to transform the electrical data into body composition variables, the Deurenberg formula was used: 0.406 (height2 (cm) / R) + (0.360 x weight) + (5.580 x height) + (0.56 x sex) - 6.48 (female : value 0; male: value 1) (28).
The SF-10 is a 10-item questionnaire designed to measure health-related quality of life (HRQOL) in children between 5 and 14 years of age. It is the short version of the SF-36 HRQoL questionnaire and, unlike the latter, must be applied by researchers. The scoring method produces two general measures of HRQoL: an overall score for the physical component and a global score for the mental component (29).
Before starting this investigation, the project was presented to and approved by the Research Ethics Committee of the province of Granada (CEI Granada, Spain).
The well-being of those participating in this study, and respect for their privacy, was at all times upheld by the researchers. In all respects, this study complied with the ethical standards currently required by the Research and Clinical Trials Committee, according to the Declaration of Helsinki of 1964 (revised in Fortaleza, Brazil, in 2013).
STATISTICAL ANALYSIS
A descriptive analysis was performed of the main variables. For the quantitative variables, the mean, standard deviation, median, and percentiles were calculated. The qualitative variables are expressed as percentages. To study the effectiveness of the intervention, the change in variables such as weight, height, or BMI was determined, while variations in the quality of life were analyzed using Student's t-test or Wilcoxon's signed-rank test for related samples, according to whether the variables were normally distributed. The association of qualitative variables was analyzed using Pearson's chi-square test or Fisher's exact test. The level of significance assumed was p < 0.05. All data were analyzed using the SPSS v.19 statistical software.
RESULTS
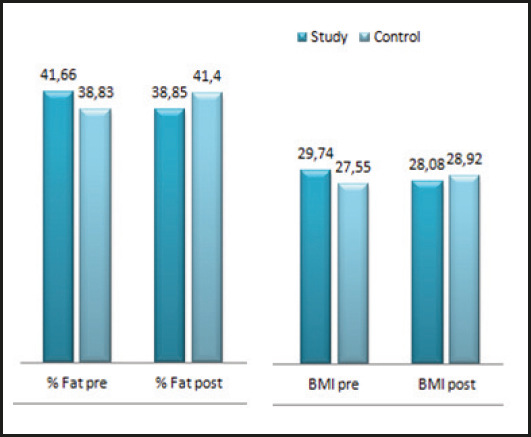
Table I describes the characteristics of the sample at the beginning of the study. In total, 27 boys and 27 girls were included. Average age was 10.62 ± 1.33 years for the Intervention group, with an average weight of 68.33 ± 17.05 kg and BMI of 29.73 ± 4.12. On the other side, average age was 10.68 ± 1.44 years for the control group, with an average weight of 65.69 ± 16.76 kg and BMI of 27.54 ± 3.75.
Table I. Characteristics of the sample in terms of body weight, height, BMI, and percentage of fat at the time of assessment

Figure 1 shows that a large proportion of the parents had no educational qualifications beyond primary school.

Figure 1. Educational background of parents (primary school, obligatory secondary education, professional training, university).
Table II shows the percentage of body fat, measured before and after the intervention, in the SG and the CG, reflecting a significant difference in this respect between the two groups. In the former, the percentage of fat decreased significantly, while it increased in the control group.
Table II. Percentage of fat in the control group and the study group before and after the intervention

Figure 2 shows the changes in body composition for the study group and the controls. The largest difference between the groups was recorded for body fat. Among the children who took part in the physical activity program and also received nutritional advice, body fat levels decreased from 28.90 to 26.56 kg, while those in the control group, with no added physical activity, experienced an increase in body fat from 26.83 to 29.84 kg. This finding highlights the importance of physical activity and play in reducing excess body fat.
The SF-10 questionnaire considers both a physical and a mental component. In the physical domain, statistically significant differences were observed in the SG between the pre- and post-intervention periods (p = 0.011) and also between the two groups (p < 0.001). In the SG, quality of life in the physical domain improved, but in the CG it worsened, as shown in figure 3.

Figure 3. Results for the physical domain of the SF-10 questionnaire, pre- and post-intervention, for the intervention group and the control group.
Figure 4 reveals statistically significant differences between the pre- and post-intervention periods in the mental component (p = 0.021). At the outset, perceptions of HRQoL were similar in the two groups, but by the end of the study there was a significant difference between them (p < 0.001). Specifically, HRQoL had improved in the SG in this domain, but it had worsened in the CG.
DISCUSSION
The results obtained by this study show that an intervention based on a program including physical activity and nutritional advice can reduce overweight and obesity in children, thus improving their quality of life, in comparison with the results presented by a control group, which received only nutritional advice.
Our findings corroborate those of Jafarzadeh et al. (30), who studied a sample of 80 children and reported that a comprehensive nursing health program improved the quality of life and reduced the body weight of children aged 11 years. The latter study used the Quality of Life Questionnaire to measure quality of life, instead of the SF-10 questionnaire applied in the present case. Another interesting study related to the quality of life of children was conducted by Robertson et al. (34), who analyzed an intervention program carried out with 115 families to improve life habits and reduce overweight and obesity among their children. According to the results obtained, this intervention with the family was effective in reducing the children's body weight and improving their quality of life. In accordance with our own findings, these authors concluded that the role played by the family is of great importance in this respect. This study performed a health campaign using focus groups to Increase parent awareness of local resources for obesity prevention and treatment. It was necessary because parents must stimulate physical activity, a healthy diet, and less screen time in their children.
Similar results in this field have also been obtained by Damuid et al. (31), who carried out a cross-sectional study of 5,759 children, and concluded that a healthy lifestyle is directly related to the presence of a better HRQoL. These authors recommended that families should reduce the time their children spent watching television, and instead increase their physical activity and promote health-giving habits.
Another cross-sectional study by Bagordo et al. (32), examined a cohort of 1,164 children, and found that children from families with a low socioeconomic level tend to have a poorer quality of life than those from families with a higher level. These results are related to our own in that children with overweight or obesity and low HRQoL often come from families with a low sociocultural level.
Overall, then, the results we present show that by reducing body weight, the physical and mental components of a child's HRQoL are improved. In the intervention group, body fat levels decreased from 28.90 to 26.56 kg, while those in the control group, with no added physical activity, experienced an increase in body fat from 26.83 to 29.84 kg. These findings, however, are in contrast with those of Lim et al. (33), who associated the child's weight with psychosocial factors, but did not obtain a significant correlation for the physical component.
CONCLUSIONS
Our intervention resulted in significant positive effects on body weight, BMI, body fat, habitual activity, physical health, and quality of life.
The participation of the family is vital in helping children improve their life habits and thus reduce their overweight or obesity.
Another important finding of this study is that families with a low socioeconomic status tend to have a lower quality of life and to present higher levels of overweight or obesity.
In this research, the SF-10 questionnaire was used to measure HRQoL in children with overweight or obesity. Both aspects had improved in the study group by the end of the intervention program.
The intervention including physical activity based on games was very effective. However, the nutritional recommendations alone, as given to the control group, did not produce any improvement in the quality of life of these children.
Our review of the literature in this field revealed that many descriptive studies do not propose any interventions. Therefore, we believe intervention studies with larger groups and a longer duration as compared to the present case should be considered, but patients may cease participating in a long-term study and become lost to follow-up. Inadequate patient retention during the conduct of a trial affects conclusive results. It is one of the difficulties of carrying out a clinical trial.
The fundamental aim of this type of research should be to identify means by which families could be helped to acquire healthier life habits and thus improve their quality of life.