INTRODUCTION
Skeletal muscle strength is a predictor of all causes of mortality; higher levels of upper- and lower-body muscular strength are associated with a lower risk of mortality (1) related to several medical conditions such as cardiovascular disease (CVD) and cancer, amongst others (2). Particularly, handgrip strength (HGS) is a health status marker (3). This represents a simple parameter, convenient, and fast for the assessment of total muscle strength that, nevertheless, may vary depending on age and health status (4). The cutoff points of HGS for low muscle strength in men and women vary between populations. HGS has shown a correlation with anthropometric parameters such as weight and height, and has been used to form indexes with the maximal HGS (5). In recent studies, relative HGS, defined as absolute HGS divided by body mass index (BMI) (HGS/BMI), showed a stronger correlation with cardiovascular biomarkers, thus muscle strength adjusted for BMI has been recommended to minimize the confounding effect of body size (6,7). By itself, in older adults, low HGS is a biomarker for sarcopenia and functional limitations (8,9). In addition, HGS levels can be an effective screening tool for CVD and different comorbidities such as type-2 diabetes (T2D) in the younger (3) and older population (10). On the other hand, high levels of relative HGS in the adult population have been associated with a low risk for CVD, including hypertension (HT), T2D and dyslipidemia (11); meanwhile, low levels of HGS are associated with alcohol consumption, poor exercise, dietary pattern, education level, age, BMI and T2D (12). A study by Kim et al. (13) has shown that the lowest relative HGS tertile in both sexes can have an influence on chronic disease development or aggravation. Stenholm et al. (14) proved that the occurrence of obesity determines the presence of low levels of HGS. In the Mexican population, the prevalence of obesity is high and represents a main factor related to HT, T2D and dyslipide- mia (15). Although low HGS has been related to mortality of all causes (16,17), the relation between levels of relative HGS and specific comorbidities have not been explored.
Accordingly, the objective of the present study was to determine the association between HGS (absolute and relative) and abdominal obesity (AO), T2D, and HT, as well as to determine the association between low relative HGS with co-occurrence of comorbidities or multicomorbidity (i.e., presence of two or three comorbidities together) in the Mexican population.
METHODS
A cross-sectional study was carried out in 860 participants from the south of Mexico. The studied group consisted of 661 female and 199 male participants, while the evaluated age range went from 18 to 65 years. The participants were invited to partake in this study and those interested were evaluated in health care centers and educational centers. Pregnant women or volunteers who were unable to stand upright with or without assistance, along with those with a physical disability that prevented independent walking (such as lower limb amputations, hemiplegia and monoplegia, musculoskeletal sequel) were not considered in the study. The study was approved by the local Research Ethics Committee of the University of Guerrero. Informed written consent was obtained from all participants before enrollment in the study and all procedures were carried out according to the Declaration of Helsinki.
MEASUREMENTS
Assessments were made regarding sociodemographic variables, clinical, and anthropometric parameters, as well as the measurement of maximal HGS.
Sociodemographic data
Sociodemographic data such as age, gender, educational level, socioeconomic level, job occupation, and marital status were obtained using a questionnaire. In addition, lifestyle habits including smoking, alcohol consumption, and physical activity (150 min/week) were also recorded. Presence of diagnosed diseases such as T2D and HT, or uses of medication for their treatment were self-reported.
Measurement of blood pressure and anthropometrics
The evaluation of the participants was performed in the morning hours between 7:00 and 10:00 AM. A physical examination of neck, folds and underarm allowed the identification of acanthosis nigricans (AN). Resting heart rate (RHR) and blood pressure were measured using an automated baumanometer (HEM-712C, OMRON, IL, USA); two measurements were made on the left arm, with the participant resting in a sitting position for at least 5 minutes before and between measurements. Body composition was evaluated according to the bioelectrical impedance technique with HBF-514C (OMRON, IL, USA) to assess weight, body mass index (BMI) (kg/m2), free fat mass % (FFM), visceral fat % (VF), and body fat (BF) percent. Height was determined using a portable stadiometer (Seca 240, Hamburg, Germany). Waist circumference (WC) was measured at the level of the umbilicus, with the subject standing. Hip girth was measured at the maximal circumference of the buttocks; both were measured in duplicate, using a measuring tape with an accuracy of ± 0.1 cm (Seca 201, Hamburg, Germany). Anthropometric indices were defined according to the following formulas: body mass index (BMI) = weight (kg) / height (m)2; waist to hip ratio (WHR) = WC (cm) / hip (cm); waist to height ratio (WHtR) = WC (cm) / height (m).
Handgrip strength
HGS was assessed using an electronic dynamometer (EH101; CAMRY, Guangdong, China). Participants were tested under the same conditions and the dynamometer was adjusted to the optimal fit for each participant according to the manufacturer's instructions. HGS was measured twice in each hand, in the standing position and with the arm extended to the front (horizontal angle 90°). The maximal handgrip strength values (kg) were considered the maximal force from each hand and were used for the data analysis. Relative HGS (RHGS) was calculated as the absolute maximal handgrip strength (kg) (AHGS) divided by BMI (reported as kg/BMI) (5). In this study most of the subjects were right-handed. Only twelve participants were left-handed.
RELATIVE HANDGRIP STRENGTH CLASSIFICATION
The values of RHGS showed a better parametric distribution in comparison to AHGS, therefore RHGS was used in the principal analyses. Values below the median were considered to evaluate the presence of decreased strength and its association with the presence of comorbidities. The values that defined decreased strength in men were: RHGS < 1.26 kg/BMI for the left hand and < 1.38 kg/BMI for the right hand; for women, decreased strength was considered as RHGS < 0.75 kg/BMI for the left hand, and RHGS < 0.81 kg/BMI for the right hand. Concurrently, the AHGS values that defined decreased strength in men were: AHGS < 34.2 kg for the left hand and < 38.1 kg for the right hand. In women, decreased strength was considered as AHGS < 21.2 kg for the left hand, and AHGS < 22.9 kg for the right hand.
COMORBIDITIES
Comorbidities were defined according to the following criteria: abdominal obesity (AO) was defined by a waist circumference for women ≥ 88 cm, and ≥ 102 cm for men according to the WHO criteria (18). Pre-hypertension (Pre-HT) was defined by the presence of diastolic and systolic blood pressure ≥ 80-189/120- 139 mmHg, and hypertension (HT) was defined according to American Heart Association criteria, by self-reporting, use of antihypertensive treatment, and presence of diastolic and systolic blood pressure ≥ 90/140 mmHg (19). Acanthosis nigricans (AN) was defined by the presence of dark, velvety hyperpigmentation and thickened skin, symmetrically distributed over the neck, armpits, and other flexural regions of the body, and type-2 diabetes (T2D) was defined by self-reports of previous physicians' diagnosis and use of antidiabetic medication.
In this study, joint presence refers to the co-occurrence of two or more conditions or metabolic characteristics, which may or may not directly interact with each other within the same individual. On the other hand, the number of comorbidities refers to the presence of one, two, and three conditions, regardless of which one.
STATISTICAL ANALYSIS
Participants' baseline demographics, anthropometrics, and lifestyle characteristics were reported as median and percentile ranges (5 and 95) for continuous variables, and were reported as proportions for categorical variables. These were analyzed using the Mann-Whitney U-test and Chi-square test, respectively. The correlation between RHGS and anthropometric parameters was determined by Spearman's rank correlation. We calculated the β coefficient to determine the effect of the presence of comorbidities and their joint presence in regards to RHGS and AHGS in a model adjusted by age. Therefore, relative risk (RR) and 95 % confidence intervals (CI) were estimated using logistic regression models to determine the association between RHGS and number of comorbidities — model 1, adjusted by age, and model 2, adjusted by age and physical activity. A value of p < 0.05 was considered statistically significant using the STATA. V.13.0 software.
RESULTS
In this study, 860 participants were enrolled. The baseline demographics and lifestyle characteristics are shown in table I. The median age was 42 years. In terms of lifestyle, a low proportion of participants smoked and occasionally drank alcohol, while 57 % said they were physically active.
Table I. General characteristics of the population

aQuantitative data shown as a 5th and 95th percentiles. bQualitative data shown as n and proportions.
The men reported higher AHGS (p < 0.001) and RHGS (p < 0.001) in both hands, when compared to women; however, the frequency of lowest RHGS was similar in both sexes: around 25 % of the population showed RHGS below the first quartile. On the other hand, women had higher WC (p < 0.001), WtHR (p < 0.001) and resting HR than men (p = 0.007). Instead, men reported higher SBP (p < 0.001) and WHR (p < 0.001) (Table II).
Table II. Comparison of variables according to sex
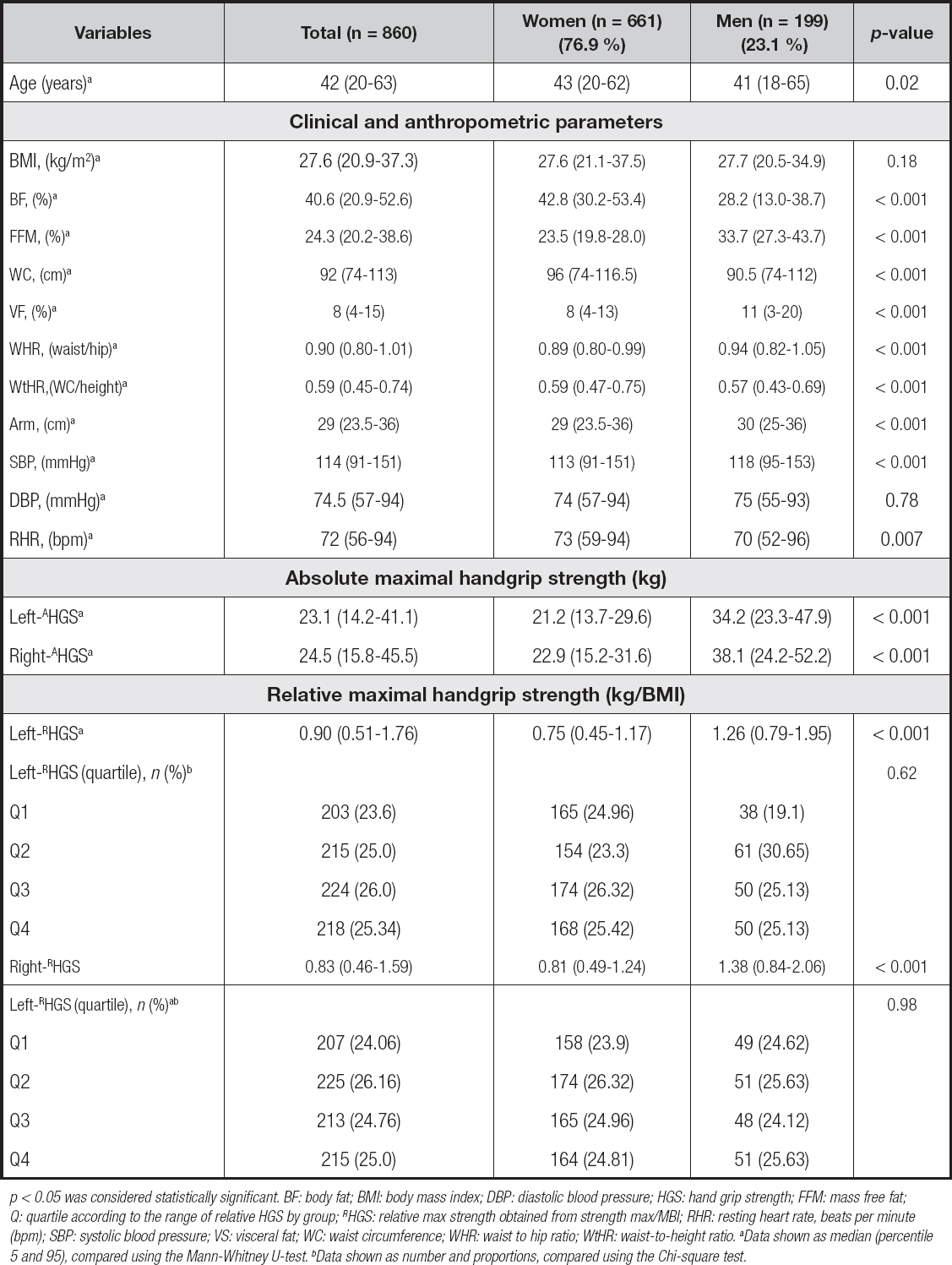
p < 0.05 was considered statistically significant. BF: body fat; BMI: body mass index; DBP: diastolic blood pressure; HGS: hand grip strength; FFM: mass free fat; Q: quartile according to the range of relative HGS by group; RHGS: relative max strength obtained from strength max/MBI; RHR: resting heart rate, beats per minute (bpm); SBP: systolic blood pressure; VS: visceral fat; WC: waist circumference; WHR: waist to hip ratio; WtHR: waist-to-height ratio. aData shown as median (percentile 5 and 95), compared using the Mann-Whitney U-test. bData shown as number and proportions, compared using the Chi-square test.
The RHGS in both hands showed a better relationship with the co-occurrence of comorbidities as well as with the number of comorbidities in women (Figs. 1C and D) and men (Figs. 2C and D), in comparison to AHGS (Figs. 1 and 2, panels A and B).

Figure 1. Absolute and relative handgrip strength (HGS) according to the co-occurrence and number of comorbidities in women. A. Absolute HGS according to co-occurrence of comorbidities in women. B. Absolute HGS according to number of comorbidities in women. C. Relative HGS according to co-occurrence of comorbidities in women. D. Relative HGS according to number of comorbidities in women.

Figure 2. Absolute and relative handgrip strength (HGS) according to the co-occurrence and number of comorbidities in men. A. Absolute HGS according to co-occurrence of comorbidities in men. B. Absolute HGS according to number of comorbidities in men. C. Relative HGS according to co-occurrence of comorbidities in men. D. Relative HGS according to number of comorbidities in men.
In this study, the prevalence of cardiometabolic-based disease was elevated. AO was the most frequent condition (55.9 %), followed by Pre-HT (26.28 %), HT (21.05 %), AN (17.17 %) and T2D (13.6 %). However, 26.63 % of participants did not present any comorbidity. The co-occurrence of comorbidities is present in around 45 % of the total sample, being more frequent the combination of AO + Pre-HT. In relation to the number of comorbidities, one third of the population had two comorbidities, principally women, although the comorbidities related to elevated blood pressure were more frequent in men (Table III).
Table III. Co-occurrence of comorbidities according to frequency and sex

p < 0.05 was considered statistically significant. AO: abdominal obesity; Pre HT: prehypertension; HT: hypertension; T2D: type-2 diabetes; AN: acanthosis nigricans. Data shown as number and proportions were compared using the Chi-square test.
The regression models adjusted by age show that the presence of comorbidities was linked to RHGS (Table IV). T2D presented the highest decrease of AHGS in both hands (left, β: -5.47, 95 % CI: -8.89 to -2.05, p = 0.002, and right, β: -6.24, -10.0 to -2.46, p = 0.001). AO presented an inverse association with HGS in both the left (relative, β: -0.24, 95 % CI: -0.31 to -0.18, p < 0.001, and absolute, β: -1.76, -3.44 to -0.081, p = 0.040) and right hands (relative, β: -0.28, 95 % CI: -0.35 to -0.21, p < 0.001, and absolute, β: -2.22, 95 % CI: -4.08 to -0.37, p = 0.019) (Table IV).
Table IV. Effect of comorbidities on relative and absolute HGS in the total sample

p < 0.05 was considered statistically significant. AHGS: absolute handgrip strength; Ref: reference category; RHGS: relative handgrip strength. β coefficient (95 % confidence interval). Model adjusted by age.
Similarly, considering the median values for defining the cutoff points of HGS for low muscle strength, in an adjusted model the presence of low RHGS in men (right, RR: 17.2, 95 % CI: 1.91-154.2, p < 0.001, and left, RR: 11.92, 95 % CI: 1.33-106.4, p = 0.020) and women (right, RR: 10.42, 95 % CI: 5.31-20.47, p < 0.001, and left, RR: 9.90, 95 % CI: 5.11-19.19, p < 0.001) presented an association with the joint presence of disease, associated with components of metabolic syndrome (MetS) (i.e., AO, HT and T2D). In general, the risk associated with low HGS is in accordance with an increase in the number of comorbidities (Figs. 3A and B).
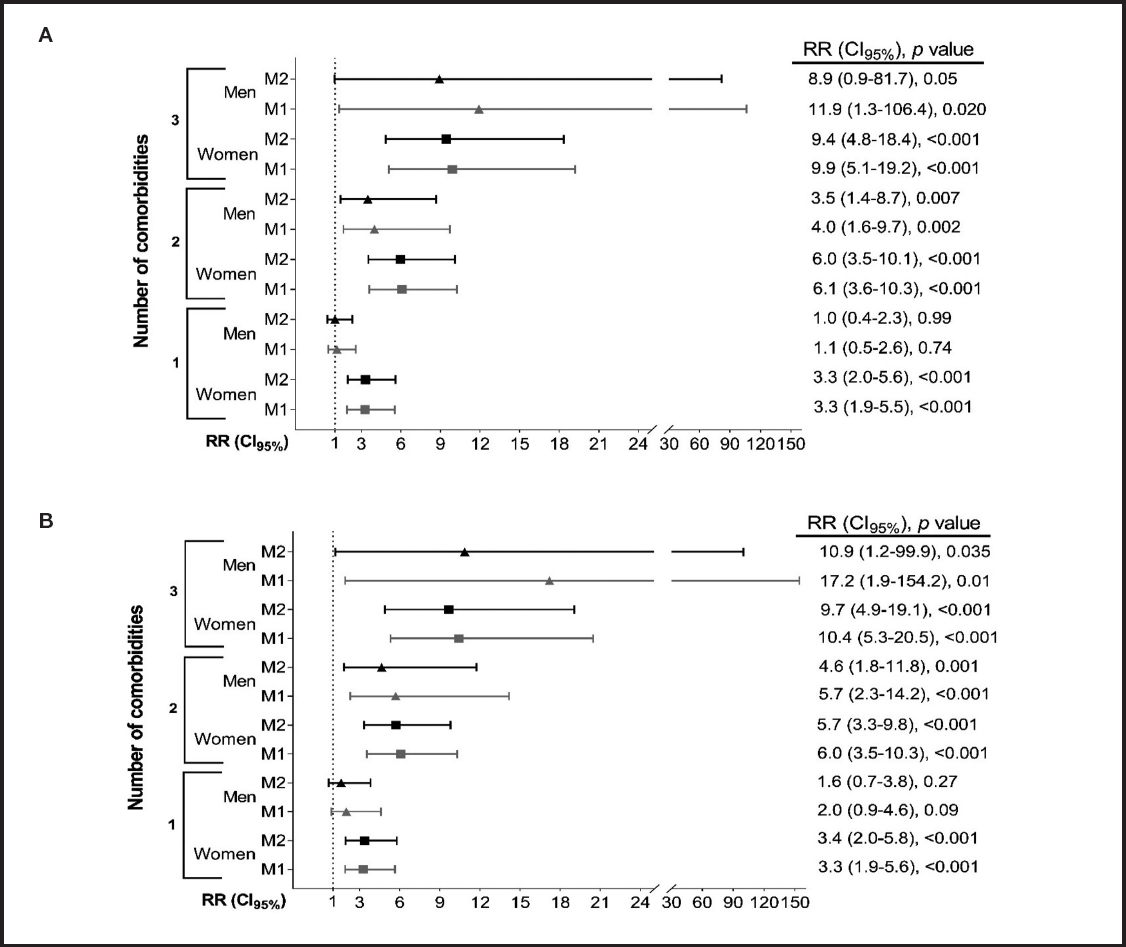
Figure 3. Low relative handgrip strength (RHGS) is associated with comorbidities and the co-occurrence of cardiometabolic-based disease in the Mexican population. A) Relative handgrip strength - left-hand. B) Relative handgrip strength - right-hand. Low RHGS according to median values was considered < 1.26 kg/BMI for the left hand and < 1.38 kg/BMI for the right hand; and RHGS < 0.75 kg/BMI for the left hand and RHGS < 0.81 kg/BMI for the right hand for women. RR: relative risk (95 % confidence interval), p value. M1: model 1 adjusted by age; M2: model 2 adjusted by age and physical activity.
DISCUSSION
The main findings of our study prove that low HGS (absolute and relative) were linked to the presence of cardiometabolic-based comorbidities, as well as to multicomorbidity (i.e., the joint presence of AO, T2D and HT). The evidence has shown that improved muscle function can affect whole-body glucose-lipid metabolism and peripheral insulin sensitivity, due to the direct or indirect regulation of whole-body energy homeostasis through myokines that are secreted from the muscle and their subsequent effects on the endocrine system (20).
In this study the prevalence of cardiometabolic disorders was elevated. AO was the most frequent condition (55.9 %), followed by Pre-HT (26.28 %), HT (21.05 %), AN (17.17 %) and T2D (13.6 %). In this context, our study evaluated the clinical components of the MetS. It has been reported that MetS consists of a cluster of metabolic abnormalities that increase the risk of developing CVD and Mexico has one of the highest prevalences of metabolic disease worldwide (21). In line with this finding, a study reported that the prevalence of MetS in Mexican adults was 36.8 % — AO was 42.7 %, HT was 42.6 %, and elevated fasting glucose was 21.0 % (22). Another recent study showed that the most frequent MetS component was low HDL-c levels (75.8 %), while central obesity was the second most frequent component in females (61 %), and elevated blood pressure was 42.7 % in Mexican adults from different ethnic groups (21). In the Korean population relative HGS has been inversely associated with the risk of MetS (5,23).
In the present study, participants with T2D presented a negative relationship with absolute and relative HGS in both hands. In agreement with these findings, a longitudinal study reported a negative association between HGS and T2D risk in adults (24). Similarly, the evidence suggests that HGS was inversely associated with fasting glucose, fasting insulin levels and insulin resistance (HOMA-IR) score; in addition, this study indicated that HGS was significantly inversely associated with T2D and insulin resistance (25). In addition, RHGS was significantly associated with better cardiometabolic health in adult subjects, therefore muscle strength may play an important role in cardiovascular health (7). Likewise, a recent study concluded that HGS may be a risk indicator for T2D in the general population (26). Karvonen-Gutierrez et al. (27) reported that a rise in the normal grip strength value by 0.1 was associated with a 19 % lower incidence of T2D; therefore, the authors concluded that improving muscle strength may contribute to preventing diabetes among women. In agreement with these findings, a study conducted in older males and females indicated that muscle weakness was associated with an increased rate of T2D (28).
Particularly in this study the prevalence of obesity was high. We found that AO presented an inverse association with HGS (i.e., relative and absolute). Another study reported that subjects with low RHGS showed high levels of AO and fat mass (29). In addition, another study found a significant association between higher RHGS and more favorable features of WC and body weight in women (30). Also, evidence has shown that HGS is inversely associated with MetS and its components, such as AO in adult men and women (23). Similarly, it has been reported that the direct effect of AO on RHGS was statistically significant. In addition, this study suggests that high glucose levels could worsen the association between AO status and lower HGS (31).
In our study, RHGS presented consistent and better relations with the number of comorbidities (i.e., 1, 2 or 3 comorbidities) than AHGS in both hands in both sexes. The differences in results across absolute and relative HGS measures support the utility of RHGS to simultaneously assess health risks of increased BMI (kg/m2) and furthermore, low muscle strength may be a feasible measure to use in future muscle strength and body composition research, given that it is relatively simple, quick, reliable and inexpensive to use (6). In an adult population, values of RHGS < 2.52 in men and < 1.55 in women were associated with CVD in men and women (32). These cut-off values are significantly higher than those found in our study, and this can be determined by the high frequency of multicomorbidity in our population; therefore, the clinical value of this parameter must be determined between populations.
The RHGS in the Taiwanese population was linked to different cardiometabolic risk factors (7). Our results are in line with previous studies, showing that in Korean men between 20-64 years old RHGS presents a positive association with BMI and in women, moreover, RHGS is positively correlated with systolic blood pressure and LDL-c (3), and RHGS decreases are significantly associated with increasing weight status (6). On the other hand, RHGS is useful to identify subjects at high risk of pre-diabetes (33), in addition to presenting an association with T2D (34) and fasting blood glucose levels (6). In this context, women with lower BMI-related HGS have a higher prevalence of T2D and HT than those with higher levels of HGS (35). A recent study identifies a strong relationship between RHGS and the prevalence of MetS in adults, regardless of sex (36). On the other hand, in older adults, fasting glucose is inversely related to RHGS (31). Also, subjects with higher RHGS had a lower risk of HT, T2D and dyslipidemia than those with lower HGS (11). In addition, RHGS is inversely associated with dyslipidemia in both men and women (37). In a Korean population aged 40 to 79 years old, RHGS showed an inverse relationship with cardiovascular risk factors such as blood pressure, waist circumference, Framingham risk score, and high-sensitivity C-reactive protein levels (25). Similarly, it has been demonstrated that RHGS is inversely associated with CVD risk factors and all-cause mortality events, therefore HGS may be a useful prognostic tool for fatal CVD events (38). As well, it could be a screening tool for a number of comorbidities and for intervention strategies design. It has been determined that an increase of 1 kg in HGS reduced the 10-year CVD risk by 1.76 times (39), with a 3 % decreased risk of mortality 5 years later (16). A meta-analysis showed that isolated progressive resistance training resulted in an increase in lower and upper body strength, and improved aerobic fitness to a similar degree as aerobic training in coronary heart disease cohorts (40). Therefore, improving muscle strength should be a prioritized public health strategy.
LIMITATIONS
Limitations include the lack of measurements of biochemical-metabolic parameters as well as the lack of detailed information on cardiorespiratory fitness and the lower sample size of men compared to women. Also, the cut-off for RHGS that defines risk associated with comorbidity presence in this study can vary between populations, i.e., according to lifestyle or presence of disease. Therefore, HGS averages must be estimated in multiple populations in order to determine general cutoff values.
CONCLUSION
Lower levels of HGS (i.e., absolute and relative) presented an association with the presence of T2D and AO in the Mexican population; moreover, lower levels of relative HGS were linked to the co-occurrence of comorbidities (i.e., joint AO, HT and T2D). Therefore, public health policies should incorporate strategies to improve HGS, due to its association with the presence of joint comorbidities.














