BACKGROUND
Delayed gastric emptying (DGE) is one of the most common complications after pancreatoduodenectomy (1). Many technical details, both in resection and reconstruction phases (2), have been associated with this complication. Likewise, DGE could be related to some baseline patient-related characteristics, such as female gender, preoperative heart failure, a high body mass index (BMI), pulmonary comorbidities or a smoking history (3,4). However, there is scarce evidence available regarding predictive factors associated with DGE. This study aims to assess the predictive factors associated to DGE after a pancreatoduodenectomy in the cohort of patients included in the PAUDA clinical trial (5).
PATIENTS AND METHODS
This study was a retrospective analysis based on the cohort of the PAUDA clinical trial patients (5). In brief, this randomized clinical trial, conducted by our study group, was performed between March 2013 and March 2015 in our setting (PAUDA Trial; NCT02246205 [http://www.clinicaltrials.gov]). The primary objective was to compare the incidence of DGE among patients who underwent Roux-en-Y anastomosis or Billroth II reconstruction after pancreatoduodenectomy. No differences were found between both techniques regarding DGE (5). However, DGE was associated to a poor preoperative nutritional status (serum albumin concentration ≤ 35 g) and to hyperbilirubinemia (>200 µmol/L) in an exploratory bivariate analysis (5). DGE was defined according to the “International Study Group of Pancreatic Surgery” criteria (6).
The following data was gathered, among others: date of birth, gender, body mass index (BMI), comorbidities (diabetes mellitus, hypertension, chronic obstructive pulmonary disease), preoperative lab data (haemoglobin, albumin, bilirubin, creatinine), type of the surgery performed (pancreatoduodenectomy with Billroth II or Roux-en-Y gastroenteric anastomosis, vein resection); intraoperative data (time of surgery, intraoperative bleeding, hypotension); and postoperative data until discharge from hospital was also gathered: pancreatic fistula (yes/no), haemorrhage (yes/no), and abscess (yes/no).
STATISTICAL ANALYSIS
Baseline characteristics were summarized using standard descriptive statistics, and a descriptive analysis was carried out. Comparative bivariate analyses, to determine potential factors associated with the DGE were previously published (5). In the present paper, multivariate regression models were adjusted to different covariates (age > 60 years, male gender, Roux-en-Y gastrojejunostomy, preoperative albumin < 35 g/L, preoperative bilirubin > 200 µmol/L, patients with postoperative haemorrhage, patients with intra-abdominal abscess, patients with pancreatic fistula). The association between potential explanatory variables and DGE was tested in 3 steps: firstly, a bivariate regression model was performed to obtain an indication of the relevance of the explanatory variables in the risk of DGE; secondly, factors showing a p-value of less than 0.100, factors that were not significant on bivariate analysis but previously reported to be associated with DGE by other authors (pancreatic fistula and Roux-en-Y pancreaticoduodenectomy) were further scrutinized for associations using the Pearson correlation coefficient (r) in order to avoid collinearity problems; at last, the third step involved a multiple regression model using a stepwise selection of variables. A p-value of 0.050 or less was considered statistically significant. Statistical analyses were performed using SPSS® software version 18 (IBM, Armonk, New York, USA).
RESULTS
DGE was diagnosed in 36 (45 %) out of 80 patients (DGE group). Patients' baseline characteristics as age, sex, body mass index or comorbidities, preoperative albumin and bilirubin, as well as their intra- and post-operative data, including technical aspects as venous resection, operating time, type of gastroenteroanastomosis; and postoperative complliations or mortality, along with others; were analysed in a bivariate study (5). The number of patients older than 60 years old in the DGE group was greater than in the group without DGE [32 (89 %), 28 (64 %), respectively, p-value: 0.009]. Likewise, the number of patients with a preoperative albumin < 35 g/L [18 (50 %); 11 (25 %), respectively, p-value: 0.036]; preoperative bilirubin > 200 µmol/L [14 (39 %); 8 (18 %), respectively, p-value: 0.039]; postoperative haemorrhage [7 (19 %); 1 (2 %), respectively, p-value: 0.011]; postoperative intraabdominal abscess [12 (33 %); 5 (11 %), respectively, p-value: 0.017]; and postoperative biliary fistula [5 (14 %); 0 (0 %), respectively, p-value: 0.011], was also greater in the DGE group.
Table 1 shows the predictive factors of DGE in patients undergoing pancreatoduodenectomy. In the univariate analysis, age over 60 years, preoperative bilirrubin > 200 µmol/L, and the presence of preoperative haemorrhage and intra-abdominal collection were associated with a higher risk of DGE.
Table I. Risk factors for delayed gastric emptying.
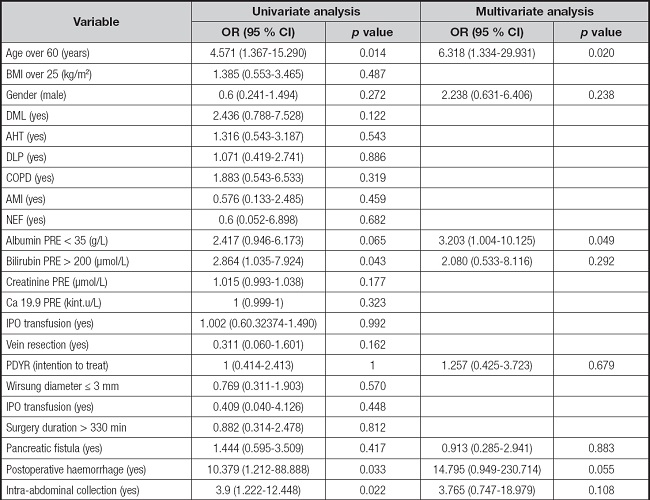
BMI: body mass index; PRE: preoperative; DML: diabetes mellitus; AHT: arterial hypertension; DLP: dyslipidemia; COPD: chronic obstructive pulmonary disease; AMI: acute myocardial infarction; NEF: nephropathy; Ca 19.9 PRE: preoperative CA 19.9 levels; PDRY: Roux-en-Y pancreaticoduodenectomy; IPO: intraoperative or postoperative.
In the multivariate analysis two risk factors were associated with DGE: the patient's age at the time of surgery (the older the patient, the greater the risk of DGE) and preoperative hypoalbuminemia (serum albumin concentration ≤ 35 g/L). A tendency to present DGE was observed in patients who had a postoperative haemorrhage or a postoperative abscess.
DISCUSSION
To our knowledge, only a few studies have performed an in-depth assessment of the predictive factors of DGE in patients undergoing pancreatoduodenectomy, especially when it comes to preoperative risk factors (3,4). In fact, severe postoperative complications as pancreatic fistula or intra-abdominal abscess have been associated with DGE (4,7), however, preoperative variables are not demonstrated as DGE risk factors in published multivariate models. Our study provides evidence that the patient's age at the time of surgery and preoperative hypoalbuminemia are independent risk factors for DGE after the surgery.
ADVANCED AGE AND DGE
The relationship between pancreaticoduodenectomy and DGE is controversial. Our results provide evidence that cephalic pancreaticoduodenectomy was associated with DGE in patients older than 65 years. These results are in accordance with those from other authors who found associated DGE after a pancreatic surgery (8) or after a pancreaticoduodenectomy in the absence of postoperative pancreatic fistulae or intra-abdominal infection (9). In contrast, some other authors did not find such an association (3,4,10,11). However, it is noteworthy that the association between DGE and liquid diets could be due to an impaired gastric fundus function in elderly patients (12), which could be correlated with our findings.
HYPOALBUMINEMIA AND DGE
Malnutrition was associated with a worse pancreatic surgery outcome (13). Hypoalbuminemia, as a variable used to assess malnutrition, was linked to a greater incidence of surgery-related complications and with a greater mortality rate after pancreatic surgery (14). However, its clinical use has been also extended to determine the severity of disease, disease progression, and prognosis in various types of cancer as colorectal cancer, breast or lung cancer.
To our knowledge, although, as above mentioned, the PAUDA trial found hypoalbuminemia (serum albumin concentration ≤ 35 g/L) to be related with DGE in the bivariate analysis, this is the first time that preoperative hypoalbuminemia was highlighted as an independent risk factor for the development of DGE in patients undergoing a cephalic pancreatoduodenectomy. In fact, the scarce data available on this issue would rather suggest otherwise (i. e., that preoperative hypoalbuminemia and DGE are not associated) (10).
On the other hand, it is widely known that cephalic pancreatic masses often present with cholestasis and hyperbilirubinemia. Both factors combined (usually present among elderly patients) may lead to severe hypoalbuminemia, which should be sought for and avoided prior to surgery. Hence, preoperative albumin, preoperative biliary drainage and nutritional support must be considered and studied prior to pancreatoduodenectomy (15). We believe an outstanding preoperative care should be provided in order to achieve good results.
LIMITATIONS
The main limitation of our study is that the nutritional status was not assessed in the study (screening or nutritional assessment; GLIM criteria for diagnoses…). The albumin levels are only a proxy of the nutritional status of the patients.
In summary, the patient's age at the time of surgery and his/her preoperative nutritional status are independent risk factors to the development of DGE after pancreatoduodenectomy. However, it must be remembered that the neoplastic disease influences the appearance of hypoalbuminemia in surgical patients. Besides, advanced age is also a risk factor for a higher rate of surgery-related comorbidities. Nonetheless, the patient's age at the time of surgery is not an avoidable risk factor that we can act on. Therefore, pancreatic surgery in elderly patients should be managed in a personalized way. On the other hand, a poor preoperative nutritional status (based on serum albumin concentration) is a possibly avoidable risk factor for DGE and was also associated with greater mortality rates. Therefore, efforts should be made to treat nutritional deterioration before the surgery.














