Introduction
19.5% of people suffer from some mental disorder throughout their lives, most commonly mood (11.5%) and anxiety (9.4%), according to data from the epidemiological study European Study of the Epidemiology of Mental Disorders (ESEMeD-Spain) (Haro, Palacín, Vilagut, Martínez, Bernal, Luque, et al., 2006). Recent data show an increase in these percentages in the Region of Murcia, (Spain) , where the lifetime prevalence of mental disorders is 33%, the most prevalent being anxiety disorders (15%) and a major depressive episode and dysthymia (14.6 %) (Navarro-Mateu, Tormo, Salmerón, Vilagut, Navarro, Ruíz-Merino, et al., 2015). With respect to the previous study (ESEMeD-Spain), these data represent a statistically significant increase in anxiety disorders and disorders in general.
Depression and anxiety (D&A) significantly reduce life quality, social functioning and work performance (Olatunji, Cisler, and Tolin, 2007), accounting for between 18% and 39% of total Primary Care Consultation (Ministerio de Sanidad y Consumo, 2007). According to data from the European Epidemiological study (ESEMeD) in primary care (PC), depression is more common than anxiety (13.4% and 9.4%), with generalized anxiety showing the highest percentage of anxiety disorders (8.5%), followed by panic (2.2%) and agoraphobia (1.5%)) (Tylee & Walters, 2007).
Almost half of people suffering from D&A have not been treated in any service in the last twelve months (Fernández et al., 2006). Of those receiving treatment, between 55% and 75% do so in PC, and from the family physician (FP) who refers patients to mental health in 5% to 10% of cases (The ESEMeD/MHEDEA 2000 investigators*, Alonso, Angermeyer, Bernert, Bruffaerts, Brugha, et al., 2004). An influential UK study (Layard, Clark, Knapp, & Mayraz, 2007), presents similar figures: FP treating 89%, psychiatry 8% and psychology 3%. According to these authors, 97% of people with D&A receive pharmacological treatment but most abandon it, as psychological treatment, their treatment of choice, is not available.
D&A are very common in PC, however, this does not mean they are properly recognized and treated. The FP correctly recognizes 22% of cases of depression and only a quarter of diagnosed cases are truly positive (Fernández, Pinto-Meza, Bellón, Roura-Poch, Haro, Autonell, et al., 2010). These data do not differ greatly from those of UK studies (Thompson, Ostler, Peveler, Baker, & Kinmonth, 2001). In a recent meta-analysis (Mitchell, Rao, & Vaze, 2011), the FP correctly diagnosed depression in 47.3% of cases and noted it in 33.6%. There is even greater difficulty in diagnosing anxiety disorders, as only one in ten cases is correctly detected in PC (National Collaborating Centre for Mental Health (Great Britain) & Royal College of Psychiatrists, 2011). In a study carried out in Spain (Fernández et al., 2012), the FP correctly diagnosed 23% of specific anxiety disorders. Therefore, accuracy in the diagnosis of anxiety and depression disorders in PC is generally low. The information system in our region, - Oficina Médica Integrada para Atención Primaria (OMI-AP) (Integrated Medical Office for Primary Care) organizes care very diffusely through the International Classification of Primary Care codes (CIAP-2; WONCA, 1999) which hinders correct diagnosis.
Most people treated for depression and anxiety in primary care (77.6%) do not receive minimally adequate treatment (Fernández et al., 2006). This percentage is hardly better in mental health, mainly due to the excessive frequency of common mental disorders, which unfortunately accounts for delays between individual appointments.
The consumption of anxiolytics and hypnotics has been increasing in Spain since 2000, despite high quality guidelines discouraging their use as the first and second choice in treatment of anxiety and depressive disorders (National Collaborating Centre for Mental Health (Great Britain), National Institute for Health and Clinical Excellence (Great Britain), British Psychological Society, & Royal College of Psychiatrists, 2011); National Collaborating Centre for Mental Health & National Institute for Clinical Excellence, 2005; National Collaborating Centre for Mental Health, National Institute for Health and Care Excellence, British Psychological Society, & Royal College of Psychiatrists, 2013). In twelve years the use of anxiolytics has increased by 37% and hypnotics by 66%. These figures contrast with those of neighboring countries in comparable periods: from 2003 to 2012 the consumption of anxiolytics increased by 34% in Spain and 4% in Italy and decreased by 6% in France. Hypnotic consumption also increased by 47% in Spain compared to 15% in Italy and 1% in France (Vicente et al., 2013).
In the Region of Murcia (Spain), the consumption of anxiolytics, hypnotics and antidepressants in defined daily doses (DDD) has continued to be on the rise. In a previous study (Martín, Garriga, & Egea, 2015) we found that the usual practice with D&A disorders is to use pharmacological therapy in PC, referring to mental health those cases that do not respond well to such treatment (Martín et al., 2015). Following the 2011 earthquake in Lorca, (Spain), a high percentage of adults with post-traumatic stress disorder (PTSD) or adaptive disorders received pharmacological treatment. Despite guidelines being against its use and accessible psychological treatment available in their own center, almost 60% of adults were medicated, compared to 0% of children who, in some cases, had severe PTSD.(Martín, Garriga, Egea, & Sainz, 2012).
The common relationship model between PC and mental health in Spain is referral: the doctor briefly notes the reason for referral on a consultation sheet that, at best, is returned by the mental health professional with indications regarding diagnosis and follow-up. This usually consists of an administrative procedure, which is often insufficient and unsatisfactory. Therefore, several alternative models have been proposed, such as training, interconsultation and liaison or collaborative models (Bower & Gilbody, 2005; Cape, Whittington, & Bower, 2010; Lipowski, 1971; Von Korff & Goldberg, 2001). In order to include psychological treatments in PC, the most frequently used model is integration, where, although the doctor does not lose responsibility for the patient, the current problem is treated by a mental health professional in the primary care center (PCC) (Gilbody & Bower, 2007).
The Layard Report (Layard et al., 2007) laid the groundwork for "Improving Access to Psychological Treatment" (IAPT), encouraging the recruitment of several hundred PC psychologists in the United Kingdom to perform empirically based treatments on depression and anxiety. The aim of these brief and evaluable treatments was to solve the problem in at least 50% of cases. As for duration, in the UK, psychological therapies of six sessions in PC are quite common, contrasting with the average duration of 12 to 24 sessions in specialized care (Cape, Whittington, Buszewicz, Wallace, & Underwood, 2010). In the UK, the integration of psychological treatments in primary care has been applied through a stepped care model of lower to higher intensity degree: self-help, guided self-help (1-2 h.), brief individual therapy (6 h.) and individual therapy of 16 hours. First, lower-intensity techniques are applied by less expert professionals, with more complex techniques and the clinical psychologist being used only if the first steps fail.
In our model, clinical assessment and accurate diagnosis are key to stepped interventions; not only due to difficulties in recognizing D&A disorders in primary, but also because of the convenience of using protocols designed for specific disorders, applied by professionals trained in such techniques, as recommended by high quality clinical practice guidelines (CPG). For example, guidelines from the British National Institute for Health and Care Excellence (NICE) recommend Barlow's Panic Control Treatment or Clark's Cognitive Therapy as first choice in the treatment of panic disorder with or without agoraphobia, cognitive- behavioral therapy (CBT) focused on trauma for post-traumatic stress disorder, or CBT developed specifically for social phobia in all cases, with medication being the second or third option (National Collaborating Centre for Mental Health (Great Britain) et al., 2011); National Collaborating Centre for Mental Health & National Institute for Clinical Excellence, 2005; (National Collaborating Centre for Mental Health (Great Britain) et al., 2013).
The aim of this article is to empirically analyze the stepped intervention model (by diagnosis and severity) in the population of primary care centers (PCC) with psychological disorders referred to a clinical psychologist, integrated in the PCC. We also try to see if there are different points of departure among participants according to geographic dispersion and the clinical psychologist integration type at the health center.
Method
Participants
A total of 566 people participated, users of six PCCs, distribution according to socio-demographic variables, see Table 2 (second column).
These participants were referred by family physicians (FP) from these centers to clinical psychologists (CPs) and resident internal psychologists according to the following distribution: 198 users to a clinical psychologist (CP) at Lorca PCC, 203 to a clinical psychologist at two PCCs Cartagena, and 165 to four resident internal psychologists from four PCCs: Cartagena (30), Murcia-Centre (13), Murcia-El Carmen (55) and Espinardo 67).
The socio-demographic profile of the patient referred from FP to PC is middle-aged (37 years) minimum 6 years and maximum 91 years, female (70%), and single (37.4%) married (35.8 %) unemployed (23.7%) or without permanent employment contract (19.5%) (Table 1).
Procedure and instruments
These participants proceed from PCCs in three localities of the Region of Murcia (Spain), two inland: Murcia (441,354 inhabitants) and Lorca (92,865 inhabitants) and one coastal: Cartagena (216,665 inhabitants). In each location there are differences in the CP’s type of integration in the PCC, and the input and experience of the clinical psychologist in the PC team:
1) Group 1 (previous integration and full-time at Lorca PCC): a full-time clinical psychologist and previous integration for a year in the PC team and working from Monday to Friday (data collected in an eight and a half month period - February to November 2012).
2) Group 2 (no previous integration but with shared work between two PCCs in Cartagena): Recent incorporation of a full-time clinical psychologist divided between two centers. Covering one year and two months from December 2011 to February 2013.
3) Group 3 (no previous integration and with part-time clinical psychologists in training, in PCCs in Murcia capital (82% of data) and 1 PCC in Cartagena): Recent incorporation of four clinical psychologists in training) one day a week for one year and one month (data collected from October 2011 to November 2012).
Psychological intervention followed a common evidence-based assessment and treatment protocol developed by the research group (Table 2). All therapists were experts in clinical interview, test administration and correction and were trained in the proposed treatments. They received a dossier containing all documentation regarding the protocol for each disorder and an SPSS v15 data file with the variables of this study.
Table 2: Evaluation and Treatment Protocol for patients referred to Clinical Psychology in Primary Care.
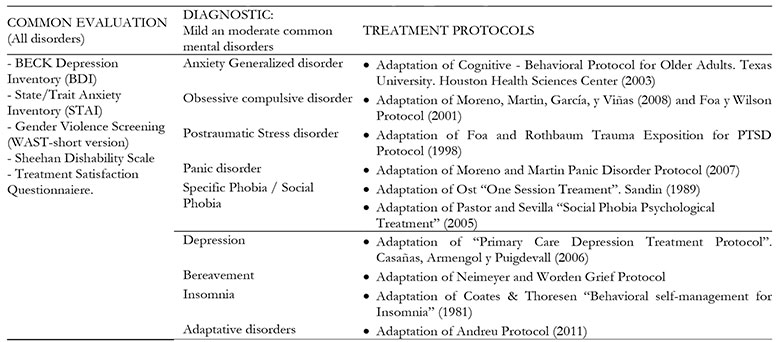
Prior to incorporating the clinical psychologist, a meeting was held in each PCC explaining the work model and referral criteria. These criteria were for users who presented mild or moderate depression symptoms, generalized anxiety, panic attacks with or without agoraphobia, posttraumatic stress, adaptive disorders, obsessive-compulsive disorders, simple phobias and social phobias. At the FP’s request, cases involving bereavement and non-organic insomnia were considered for assessment. The FP could ask the clinical psychologist directly and / or use the computer system. The FP did not take part in the selection of users beyond the criteria shown. Informed consent was requested from all patients, guaranteeing confidentiality of results and exclusive use of data for research purposes.
The following scales were used:
- Beck Depression Inventory. Comprises 21 items to assess the intensity of depression. Each item is valued from 0 to 3 points depending on the alternative chosen. The total score of the 21 items varies from 0 to 63. Its reliability is 0.83 (Cronbach's alpha coefficient) (Beck, Ward, Mendelson, Mock, & Erbaugh, 1961).
- State / Trait Anxiety Inventory (STAI). Evaluates in the general population (adults and adolescents) the current level of anxiety and predisposition of the person to respond to stress. It consists of 40 items, half from the State subscale (measuring current mood), and the other half from the Trait subscale (measuring usual mood). The scoring of each scale, ranging from 0-30, translates to centiles by sex, based on available scales. The State subscale has a reliability coefficient of 0.90-0.93 and the Trait subscale 0.84-0.87 (Seisdedos Cubero & Spielberger, 1997).
- Sheehan Disability Scale (SDS), Spanish adaptation (Bobes, Badía, Luque, García, González, & Dal-Ré, 1999). Comprising 5 items; the first three assess disability, the fourth assess stress perceived through subscales that score from 0 to 10 and the fifth assess social support perceived in a percentage subscale of 0% to 100%. It presents a Cronbach alpha value of 0.72 and intraclass correlation coefficient for total disability, perceived stress and perceived social support of 0.87, 0.63 and 0.75, respectively.
- Woman Abuse Screening Tool - short version (WAST-short) (Fogarty & Brown, 2002). A self-administered screening questionnaire of two items to detect violence against women. A score of "1" is assigned to each of the most extreme responses (great difficulty and a lot of tension) and a "0" rating to the other response options. The final score ranges from "0" to "2" and both "1" and "2" scores are deemed a positive screening result.It shows sensitivity of 91.4% and specificity of 76.2%, with its positive predictive value 40.2 and negative 98.1. The positive coefficient variation is 3.84 and negative 0.11.
From the evaluation, a stepped intervention model was used based on diagnosis and severity, structured in five levels (Figure 1):
Level 1. Normalization (or indication of non-treatment): For demands not constituting a psychopathological disorder (e.g., sadness following the death of a relative or after a relationship breakup), normalization of symptoms with a monthly follow-up appointment is proposed.
Level 2. Group therapy: If the disorder is mild or moderate, brief psychological treatment (five to eight sessions) is proposed, with an empirical and clearly detailed basis to allow its replication.
Level 3. Individual treatment: For moderate anxiety and depression disorders or for inability or unwillingness to take part in group treatment. Although duration can be changed according to needs, an average treatment of 8 sessions is advised, which can be shorter for specific phobias and longer for moderate depression (12 sessions).
Level 4. Referral to mental health: if following initial assessment, or during treatment, any disorders are considered severe and / or another psychopathological diagnosis is detected.
Level 5. Emergency referral: when the reason for consultation is urgent or critical, such as self-harm or doing harm to others or active psychotic symptoms.
Design and statistical analysis
An epidemiological, cross-sectional, multicentric study carried out between October 2011 and February 2013 in six Primary Care Centers PCC in the Region of Murcia (Spain) (three in Murcia, two in Cartagena and one in Lorca).
Sociodemographic variables (age, sex, marital status, living status, education level, profession, employment status) and some clinical variables (psychotropic use, work leave, gender violence screening and clinical diagnosis according to ICD-10) are compared through percentages and adjusted residuals, according to the three types of CP integration in the PCC.
In the quantitative clinical scales (depression, anxiety and disability) the means were compared using ANOVA with Bonferroni post hoc tests with an Alpha significance level (p <.05) according to CP integration type in the PCC and the level of intervention offered. The effect size for each pair of comparisons between groups was obtained using Cohen's d. Following the interpretation of these indices proposed by Cohen (1988), the d between 0.50 and 0.79 would indicate a moderate effect, and large above 0.80.
Statistical analysis was performed using the SPSS package, v15.
Results
As mentioned in the previous section Participants, during the study period FPs referred 566 people between October 2011 and February 2013. 88% (496 people) attended the first assessment interview. The reason for non-attendance of the remaining 12% could not be verified. There are significant differences in the non-attendance percentages between the three groups according to CP integration type in the PCC (Chi square = 43.27; p <.001), the lowest percentage corresponding to group 1 with 2%, followed by group 2 with 12.3% and group 3 with 24.8%.
In the comparative analysis of the socio-demographic data according to PCC location, significant differences were found in different variables, among those, due to involvement in the study, a greater percentage of people separated, unemployed and with fewer permanent contracts in Cartagena (Group 2) (adjusted residuals > ± 1.96) (See Table 1).
Of the 496 interviewed, 50% received pharmacological treatment and 10% were on sick leave for reasons of consultation. Of the 343 women referred who attended the first interview (69.2%), 223 were screened for gender violence (65%), with 17% proving positive.
The characteristics of people by region and CP integration type are detailed in Table 1.
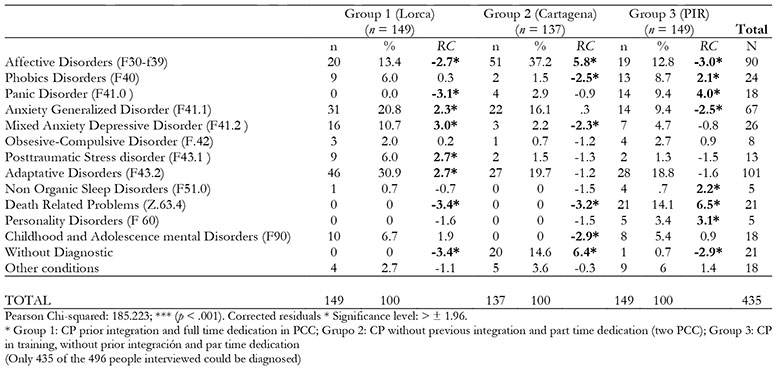
Applying CIE-10 (29) criteria, the most commonly diagnosed disorders were: adaptive (23%), affective (21%) and generalized anxiety (15%), with the rest below 6% (Table 3). Significant differences were found in the distribution of diagnoses according to location and CP integration type (see adjusted residuals in Table 3). In group 1 (Lorca), generalized anxiety disorders, mixed anxiety and depression, posttraumatic stress and adaptive disorders predominate; In group 2 (Cartagena) a greater number of affective disorders is observed without established diagnosis; and there is greater variability in group 3 with resident internal psychologists, with a relatively high percentage of panic and bereavement disorders (adjusted residuals > ± 1.96).
Table 3: CIE-10 Diagnostics. Comparison between groups for CP incorporation*. Frequencies, percentages, corrected residuals and Chi-squared test.
In accordance with the stepped intervention level, of the 496 interviewees, 94 (18.9%) received "no treatment indication" (level 1), 350 were referred to treatment at the PCC (levels 2 or 3) (70.6%) and 51 subjects were referred to mental health centers (level 4) (10.3%) only one was referred as an emergency (level 5) (0.2%).
A total of 376 subjects completed the questionnaires and scales mentioned, 36 belonging to the non-treatment indication group (level 1), 317 to the PCC treatment group (levels 2 or 3), and 23 were referred to mental health centers (level 4). Significant differences were found in ANOVA (see Table 4) in all scales according to the level of therapy offered and following the logic of the stepped procedure: lower scores for indication of non-treatment, intermediate for treatment in primary care and higher for those referred to mental health centers.
Table 4: Pretest Inventory Scores for Stepped Intervention level*. Frecuencies, Means and Typical deviations and ANOVA (F).

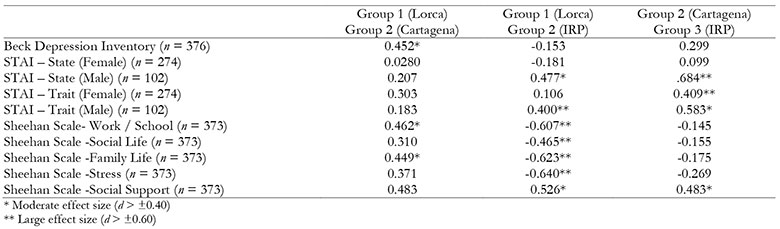
Table 5 shows the ANOVA of the results of clinical scales according to distribution of subjects by geographical location and CP integration type in PCC. In the post hoc analysis, there were significant differences in the Beck Depression Inventory between groups 1 (M = 18.6, SD = 10.434) and 2 (M = 23.3, SD = 11.596). In the STAI-state for males, a higher mean was observed for group 2 (M = 36.5, SD = 14.166) with respect to group 3 (M = 27.7, SD = 7.137) and in the STAI-trait for women, a higher mean was also obtained for group 2 (M = 38, SD = 9,831) compared to group 3 (M = 33.5, SD = 13.549). In all subscales of the Sheehan Disability Inventory between groups 2 and 3, with higher averages than group 1 (indicating lower disability index in group 1). Using Cohen's d as an effect size measure, all these differences present a magnitude of the mean effect (d> 0.40) or high (d> 0.60) (See Table 6)
Table 5: Pretest Inventory Scores for CP integration type in PCC* (Means and Typical deviations and ANOVA (F)).

Discussion
Referrals were generally as expected (Martín et al., 2015): adaptive, depressive or anxiety disorders comprised 79.3% of treated cases and only 10% of the assessed sample was referred to the mental health center for being severe cases or not meeting the agreed criteria.
Differences between groups according to CP integration type in the PCC were expected, since full-time integration and implementation eight months before the start of this study (Lorca) would positively influence the adjustment of referrals, due to the psychologist´s daily presence and a greater running of the process. Working daily with the PC team allows immediate feedback from the family physician’s referrals by being able to clarify the keys to what can be treated in PC and what should be referred to MH. In some cases the FP relies on the CP to assess complex cases and consider referral to MH. The lowest adjustment in referral occurs in the cases of lesser CP presence (one day a week) and recent incorporation (group 3), which also has the greatest diagnostic variability. The differences in points of departure between groups by location and CP integration type in the PCC are also evident in depression, anxiety and disability scales. The effect magnitude measured with Cohen's d is average or high in nine of the ten subscales used in comparisons between groups. The effectiveness analyzes performed with these data should explore the magnitude of the total change and change in each group (Garriga, Martín, Egea, Díaz, Campillo y Espinosa, sometido a publicación)
There are different points of departure among samples in sociodemographic and clinical variables according to location and CP integration type in the PCC. In Group 2 (Cartagena) we see a higher percentage of affective disorders as well as significantly higher depression and trait anxiety averages. This could be related to a significantly greater percentage of patients who are separated, unemployed or with transient disability in this group (group 2). In group 1 (Lorca) the highest percentage of adaptive disorders due to post-traumatic stress and generalized anxiety may be connected to the May 2011 earthquake which occurred in this area, since it coincides with the study data of delayed or chronic disorders observed a year after the earthquakes (Martín, Valera, Albacete, Sánchez & Egea, 2013). And in group 3 with resident internal psychologists the wide variability of diagnoses can be related to lower attendance frequency (one day a week) and to greater difficulty in imposing care criteria due to the professionals being in training.
Greater access to psychological interventions by integrating the CP in primary care reduces the medicalization of mild and / or moderate mental pathologies. 50% of patients referred to the CP were medicated. Although this may seem high, it is lower than the 89% collected in a previous study performed with patients with panic disorder and / or agoraphobia referred from primary care to mental health centers (Martín et al., 2009). In group 1, with a daily presence of the CP in the PCC and the stepped intervention already used there is a significantly lower percentage of people referred with medication (41%) than groups 2 (58.1%) and 3 (49.7%).
As mentioned in the introduction, the family physician´s diagnosis of depression and anxiety corresponds to a very low percentage to the actual diagnosis of specific disorders (Fernández et al., 2010; Fernández et al., 2012; National Collaborating Centre for Mental Health (Great Britain) & Royal College of Psychiatrists, 2011). In a context of high diagnostic uncertainty, the clinical psychologist provides the rigor and experience to reach correct diagnosis, ruling out the presence of other mental disorders. Consequently, following assessment (clinical interview and scales) the psychologist decides in one or two sessions if treatment is not needed and/or to inform the patient that their symptoms are normal reactions (level 1 of the stepped intervention model); if they are mild and moderate anxiety and depression disorders that may not require pharmacological treatment and could benefit from brief group or individual intervention (levels 2 or 3), or whether moderate or severe disorders should be referred to mental health (level 4) .
Facilitating access to psychological intervention in a less stigmatizing environment by integrating the CP into the PCC increases the likelihood that the patient will attend treatment. 12% of non-attendance at the first appointment is in the lowest range of those collected in the literature, which range from 10% to 60% (García & Ortiz, 2002). In our study, the lowest percentage of non-appearance occurred in group 1 (2%), followed by group 2 (5.9%) and group 3 (24.8%). This coincides with the CP integration type in the PCC, which is present every day of the week in group 1, half of the days in group 2 and one day a week in group 3 made up of resident CPs. The fact that the population is seen by residents can increase the percentage of non-attendance at the first appointment (Campbell, Staley, & Matas, 1991), which along with the fact that residents worked fewer days at the PCC can explain why the percentage of absence is 12 times greater in this group than in group 1 and quadruple that in group 2.
Nowadays, it is imperative in any health setting and especially in primary care and mental health to introduce measures to detect gender violence. In our study, 17% of positive screenings were collected, higher than the percentages obtained in the population of women treated in PC, consistent with the consideration of psychopathological symptoms as risk indicators of gender violence in the primary care area (Plazaola-Castaño, Ruiz-Pérez, & Hernández-Torres, 2008). If after screening, gender violence was confirmed, clinical practice guideline recommendations on how to treat women abused by their partner (Garriga, Martín, Balanza, Bonilla, Cámara, Cánovas, et al., 2010) would be proposed
Among the limitations of the work are that it is an observational study that only allows generating hypotheses about associations or lack of specific association, that more specific studies should confirm or refute. As it is a multi-centric study in six PCCs and with several professionals there has been an unfortunate loss of data. It is also a cross-sectional study, with a small sample not representative of the region and biased as PCCs were not randomly chosen, which does not allow us to generalize conclusions.
However, the study’s strengths are its multicentric nature and, unlike previous studies (Harkness & Bower, 2009), psychological intervention is performed by clinical psychologists with different professional levels; specialist assessment, and then a more precise diagnosis, corroborated by psychometric tests, avoiding unnecessary interviews by unqualified personnel (Richards & Borglin, 2011).
Conclusions
The presence of the clinical psychologist in primary care provides diagnostic rigor and enables "normalizing" those symptoms not requiring medical or psychological treatment, symptoms which, even today, in a high percentage are treated with medication. Normalization allows more resources to be devoted to those patients most in need.
Access to psychological treatment reduces non-attendance at first appointment. Collaboration with family physicians can reduce the proportion of patients referred with medication in the medium term. This would allow the use of psychological treatments of mild and moderate anxiety and depression disorders as the first line of choice, as recommended by clinical practice guidelines.
Study data show that for integration of the clinical psychologist in PC, it is better they be full-time, like the rest of the staff. They also empirically support the convenience of including these professionals in PC, as is already the case in several Spanish autonomous regions (Duro, 2017).