Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.103 no.1 Madrid ene. 2011
LETTERS TO THE EDITOR
Anal Melanoma with satellite implantations on the lower rectum
Melanoma anal con implantaciones satélites en recto distal
Key words: Anal melanoma.
Dear Director:
Melanoma of the canal anal is a rare malignancy and due to the site of the lesion and the lack of early presenting signs and symptoms, the diagnosis is usually delayed (1, 2, 3). There is a peak incidence during the seventh decade of life and a marked predominance of female patients, being the hemorrhage, anal pain or anal mass the main complaints.
Histologically, it is characterized by a great cellular variability, being able to mimic several other histological types. Thus the immunohistochemical stains, such as S 100 protein and the HMB-45, became a useful instrument in establishing the correct diagnosis.
Although it's a situation that folows with a very low long-term survival, there is no consensus in the best treatment option (3,5,6).
Case report
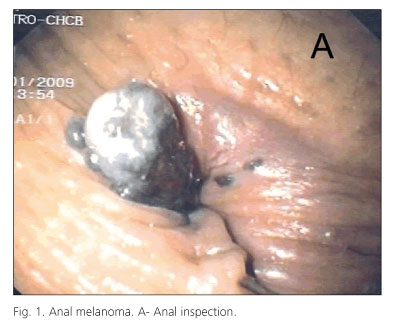
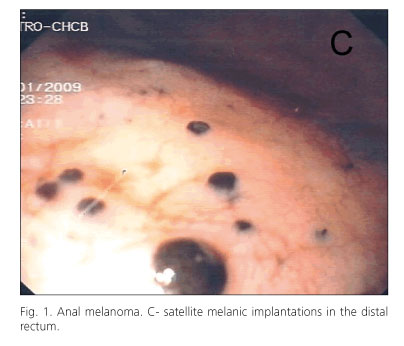
A 81-year-old female patient presented in our institution with anal pain and tenesmus during the last month. She referred personal history of diabetes mellitus and congestive heart failure. The ano-rectal examination showed a brownish anal mass extruding the anal canal, and the digital examination revealed a circular hard and painful tumor. The fibroscopy showed a pigmented ulcero-vegetant lesion in the anal region and several other little pigmented lesions on the lower rectum (satellite lesions?). The histopathological examination of the anal lesion and one of the melanotic lesions on the rectum showed the same pattern of pleomorphic cells with melanic pigment in their cytoplasm and positive expression for S 100 protein and HMB-45, thus confirming the diagnosis of melanoma. The computed tomography showed an increase fat density in peri-rectal area, pelvic adenopathies and several milimetrical hepatic nodular formations, suggestive of liver metastasis. The patient had a good control of anal pain with the prescribed analgesia and she was referred to medical oncology. However, the patient died two weeks later after de diagnosis of melanoma, in the context of pneumonia.

Discussion
Malignant melanoma of the anus is a rare and aggressive neoplasia and in the reviewed literature we did not found more than two cases of anal melanoma with satellite lesions in the lower rectum (1). Accordingly with the current AJCC staging system, the presence of satellite lesions on cutaneous melanoma had an adverse prognostic impact and evolves a new stage of disease, but we still don't know their significance in mucosal melanomas. The most important treatment modalities are surgery, irradiation and chemo-immunotherapy. The surgical approach seems to be the best option given is curative-potential in the earlier stages and the ability to achieve complete local excision in-palliative conditions, bringing a positive impact in quality of life (1,2,3,4,5,6,7). Although there aren't still consensues, it's reasonable that surgery in palliative setting is crucial in the treatment of rectal obstruction, incontrollable bleeding or pain. In our case, none of these situations was observed and the patient had a bad clinical status, so we chose a conservative treatment. Chemo-immunotherapy and radiotherapy can be used as adjuvant or palliative intention but they had brought disappointing results (1,3). Despite these results, chemotherapy seemed to be the only option to our patient. In the past few years it has been associated immunotherapeutic agents to the chemotherapy schemes, such as IL-2 and INF, but this option has not been associated with enhanced survival rate.
In view of mucosal melanomas, early detection and more effective local and systemic therapeutic approaches are necessary to improve survival of these patients.
P. Duarte, R. Ramos, C. Vicente, C. Casteleiro-Alves
Gastroenterology Department. Centro Hospitalar Coba da Beira. Covilhã, Portugal
References
1. Heyn J; Volkenandt M et al. Malignant melanoma of the anal region. Clinical and Experimental Dermatology 2007; 32: 603-607. [ Links ]
2. Balicevic D.; Tomic K.; Kruslin B. et al. Synchronous anorectal melanoma. Worl J Gastroenterol 2006; 12: 3453-3455. [ Links ]
3. Ishizone S; Miyagawa S et al. Surgical treatment for anorectal malignant melanoma: report of five cases and review of 79 Japanese cases. Int J Colorectal Dis 2008; 23: 1257-1262. [ Links ]
4. Seya T; Tajiri T et al. A Case of rectal malignant melanoma showing immuno-histochemical variability in a tumor. J Nippon Med Sch 2007; 74: 377-381. [ Links ]
5. Belli F; Leo E. et al. Melanoma of the anorectal region: the experience of the National Cancer Institute of Milano. Journal of Cancer Surgery 2009; 35: 757-762. [ Links ]
6. Droesch J; Mann G. et al. Wide excision or abdominoperineal resection as the initial treatment for anorectal melanoma? American Journal of Surgery 2005; 198: 446-449. [ Links ]
7. Wom Kim K; Lee MG et al Primary Malignant Melanoma of the Rectum: CT findings in eight patients Radiology 2004; 232: 181-186. [ Links ]
8. Mohr P; Buzaid A et al Staging of cutaneous melanoma Annals of Oncology 2009; 20: vi14-vi21. [ Links ]














