Current research has pointed out the importance of early experiences for lifelong health and wellbeing (Shonkoff & Fisher, 2013). In particular, early positive experiences provided by parental figures have shown long-term effects on a child's later development and health (Van IJzendoorn & Bakermans-Kranenburg, 2017). Likewise, exposure to toxic environments has a negative effect on the developing brain, which can jeopardise a child's development and wellbeing (Luby et al, 2013). Consequently, evidence-based interventions (EBIs) have been proposed that are focused on the promotion of healthy environments and the prevention of child maltreatment in the family context (Shonkoff & Fisher, 2013).
For EBIs to be more effective in the early years of life, a multisector approach involving the support network of childhood education, social services, and the healthcare system is recommended to increase their universal application as a prevention strategy (Spoth et al, 2013). In particular, primary care services have been considered a universally accessed and non-stigmatised setting that is particularly suited to implementing preventive EBIs, which may complement more intensive selective and indicated interventions conducted by other services (Briggs, 2016). Healthcare providers can inform parents about community resources such as home visiting programmes and parent support groups that can help prevent child maltreatment, provide information about child development, and offer strategies for dealing with a variety of parenting challenges. Yet, in a review of European national policies on child maltreatment prevention, of the 68 policies analysed only 11 (16%) involved the health sector in prevention activities at policy and programme levels (Ramiro-Gonzalez et al, 2019). The present study illustrates one way to activate the contribution of the primary care system to the support network, reporting the feasibility and effectiveness of an early universal programme combining an online course with face-to face parenting support.
The Family-Centred Care (FCC) model currently endorsed in healthcare settings (Shields, 2015) represents an opportunity to incorporate preventive EBIs conveying parenting support into the portfolio of primary care services. This model is characterised by a professional-family relationship rooted in respect and information sharing, in which both parts collaborate to share responsibility for a child's healthcare (Fordham et al. 2012). However, there is still a lack of consensus about a practitioner's particular role in the FCC model (Coyne, 2013) and training needed to ensure they deliver quality parenting support (Fix et al, 2018). The Council of Europe's (2006) Recommendation (Rec 2006/19) on policy to support positive parenting has noted the co-responsibility of states to provide psycho-educational parenting support from a multiagency work perspective. In addition, this recommendation has endorsed prevention quality standards that EBIs (e.g, positive parenting programmes) should meet, such as a manualised description and rigorous implementation and evaluation (Gottfredson et al, 2015; Rodrigo et al, 2015).
Despite the opportunity offered by the FCC model, a recent meta-analysis of primary care-based interventions aimed at parents of children younger than 36 months only identified six programmes promoting positive parenting behaviours (Shah et al, 2016), indicating the paucity of evaluation studies with EBIs in this area. The parenting programmes reviewed have been mainly delivered through face-to-face activities at group meetings (e.g, Triple P, Incredible Years) and, to a lesser extent, through one-to-one consultations at paediatric check-ups and home visits (e.g, IY® Well Baby Programme, Healthy Steps). Half of these interventions have used paediatricians, whereas the rest have incorporated other healthcare professionals (e.g, nurse practitioner or social worker) or even external specialists, which in the latter case may jeopardise programme sustainability. To overcome this barrier, some countries (e.g, United Kingdom and Netherlands) have integrated comprehensive parenting support into their primary care services through programmes such as Family Nurse Partnership (Asmussen & Brims, 2018; Mejdoubi et al, 2015), that are implemented by primary care providers.
The recent arrival of web-based programmes in healthcare settings has shown their potential advantage in terms of cost-effectiveness, universal availability, high fidelity, and feasibility (Glascoe & Trimm, 2014; McGoron & Ondersma, 2015). However, some challenges remain. First, web-based parenting programmes have generally been centred around specific health topics such as sleep (Cook et al, 2015; Mindell et al, 2011), feeding (Bensley et al, 2011), or behavioural problems (Baumel & Faber, 2017; Breitenstein et al, 2015; McGrath et al, 2013), while a more global approach to foster a child's healthy development has been less explored. Second, web-based programmes spontaneously attract mainly highly educated mothers with considerable experience in the educational use of Internet (Dworkin et al, 2013), with other sectors of the population less likely to benefit from these resources. Finally, completion rates of universal online courses are usually low (Callejas et al. , 2018; Wangberg et al. 2008). To overcome these barriers, the use of hybrid methods combining online activities with face-to-face sessions has been proposed to foster parental involvement and improve adherence to the programme (Glascoe & Trimm, 2014).
'Gaining Health and Wellbeing from Birth to Three' Programme
The Gaining Health and Wellbeing from Birth to Three programme (herein GH&W) is aimed at training parental figures in personal, caregiving, and socialisation skills that foster a young child's healthy development and wellbeing. The GH&W has three main features. First, it is conceptually grounded in the developmental system model (Guralnick, 2011, 2013), according to which parental support should be centred on the promotion of parent-child transactions (attachment bonds), family-orchestrated child experiences (daily stimulating routines), and health and safety activities provided by the family (health promotion activities). All should be adjusted to the child's developmental stage to set a safe and stimulating scenario with plenty of learning opportunities. Second, healthcare providers should guide and support parental figures as health promoters and co-responsible agents of their child's health and wellbeing (Farber et al, 2017). This means that the intervention should promote parents' self-regulatory aspects in their attempts to organise and manage their child's routines and behaviour, such as parental agency, sense of competence, internal locus of control, and parental ability to manage childrearing goals (Sanders & Mazzucchelli, 2013). Finally, parental support should be embedded as much as possible within the practitioner-family collaborative FCC approach aimed at promoting parental autonomy, which in turn has a positive impact on proper use of primary care services (e.g, reducing over-use rates).
The GH&W is a hybrid programme composed of three modalities: online, group-based, and individual support. The programme can be used in childhood education, social services, and primary care system. A brief description of each modality follows.
Online course (http://aulaparentalidad-msssi.com/), sponsored by the Spanish National Prevention and Health Promotion Strategy in 2013. This course is freely available on a Moodle platform with four modules addressing attachment bonds, feeding, physical activity and play, and sleeping routines, designed for three age ranges: zero to one, one to two, and two to three years old. The modules follow the same structure: a) a video-clip introduction of the topic; b) developmental landmarks involved in each topic (vignettes or illustrations), c) parent-child daily scenes around each topic (vignettes or video-clips) where parents are asked to label the scene and predict the consequences; d) a recall exercise, in which participants respond to true/false statements with feedback; and e) links to additional online resources with evidence-based content. Downloadable leaflets with take-home messages are also available. The GH&W follows an experiential methodology adapted to web contents based on the presentation of a variety of everyday situations to promote parents' reflection about their role and their impact on their child's development (Suárez et al, 2018). The full programme takes an average of eight hours to complete.
Workshop group (adapted from Rodrigo et al, 2017), sponsored by the Health Service of the Canary Islands regional gorvernment. This modality included four face-to-face group sessions based on the experiential methodology (Rodrigo et al, 2010) in which parents perform several activities based on the GH&W web-based materials guided by a facilitator (paediatrician, nurse, or social worker). The structure of each session was as follows: a) welcome and introduction to the topic; b) my routine, where parents identify new abilities of their child associated with the topic contents and reflect about their perceptions and feelings related to parenting role; c) a personal commitment to try at home involving an improvement to their routine as a parent; and d) a wrap-up and summary of main ideas and acknowledgment of group participation. The first session also included an introduction activity and the last session had the final assessment and a farewell activity. Each session lasted an hour and was run weekly by a leader and a co-leader. Participants were encouraged to have completed or at least initiated the corresponding module of the online course before the workshop session.
Individual support. This included individual professional (paediatrician or nurse) support at regular check-ups as a further reinforcement of the group session. After regular welcome, the practitioner applied a Teachable Moment Technique, that uses brief spaces of communication as opportunities marked by an increased capacity for health-promoting changes (Lawson & Flocke, 2010). The practitioner opened informal exchange with the parent(s), exploring doubts, concerns, and perceived strengths in the parenting role. Then, the practitioner turned to a reflection-and-change opportunity moment, in which the parent(s) reflected on and committed to setting short-term goals in their family routine. As in the workshop, parental figures were given printed leaflets with information on child-rearing and development, as well as on age-appropriate stimulation activities.
Aims
The study took place in the Canary Islands (Spain), which provided the proper organisational setting for the first implementation of the GH&W hybrid version in public primary care services. The aims of this study were: a) to evaluate the feasibility of the GH&W hybrid version for primary care services and b) to evaluate the effectiveness of the GH&W comparing three cumulative intervention levels in the centres: level 1, online course dissemination only, level 2, dissemination plus workshop group intervention, and level 3, dissemination and group support plus individual intervention. To test programme effectiveness, two strategies were followed. First, a variable-centred approach was used, by evaluating within each intervention level pre-post participants' changes in health promotion activities, parental self-regulation, satisfaction with the service, and satisfaction with family life. Second, a person-centred approach was used, by exploring participants' patterns of individual pre-post changes across outcomes and their relation to the level of intervention received.
Method
Recruitment and Procedure
Primary care centres. First, an initial pool of 21 centres in Tenerife and 17 centres in Gran Canaria was selected by the Public Health Management according to the demographic area. The heads of the centres were informed about the project in a meeting with the research team. After that, they had a month to consult with their professional staff and decide whether or not to participate in the experience. A total of 20 primary care centres (8 in Tenerife and 12 in Gran Canaria) joined. Second, primary care centres were randomly assigned to one of the three intervention levels. The centres kept the following geographical proportions: 1:1:2 (urban/peripheral/rural) and 1:1 (north/south) to achieve a representative sample of the areas and similar rates of families with children up to three years old.
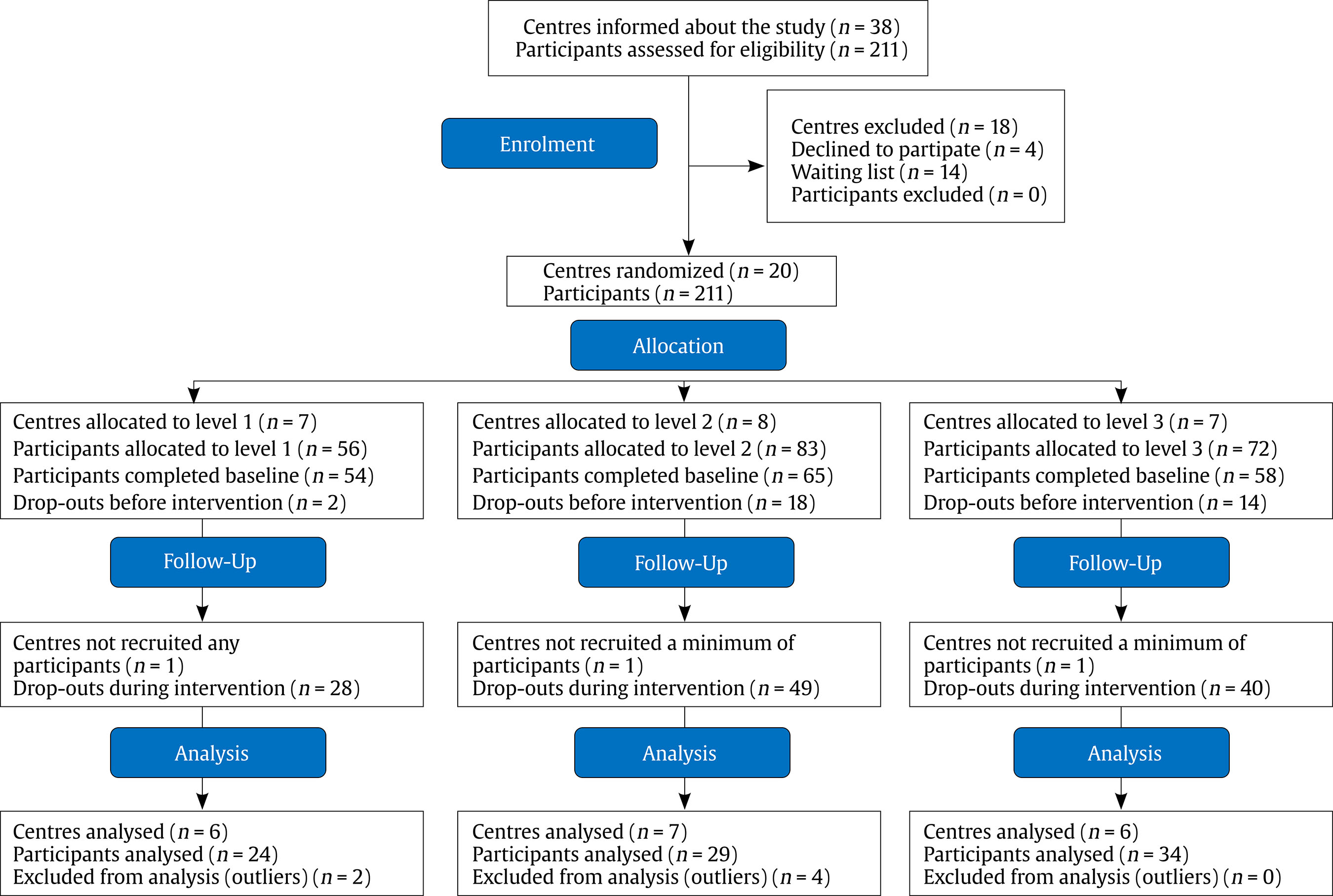
Primary caregivers. The professional healthcare informed those parents who met inclusion criteria (having a child < 36 months old and being current users of the Canary Islands Health Service) about the possibility of joining the study. A total of 211 participants signed up for the study, all of them were eligible; 177 of them completed the baseline. Finally, 87 primary carers (39 in Tenerife and 48 in Gran Canaria) completed the intervention and the follow-up assessments. They were recruited by 50 practitioners (paediatricians, nurses, and social workers) at regular medical check-ups and consultations (see Figure 1 for flow diagram).
Measures
Participant profile
Sociodemographic datasheet. It was composed of ten items, including adults' and children's sex and age, primiparous, residence area, family structure, educational level, employment status, and perception of child health status.
Use of Internet questionnaire (Callejas et al, 2018). This survey measure consisted of seven questions divided into two sections. First section was Internet experience that was based on two items: “How often do you go online?”, answered in a 0-4 scale, where 0 = at least once a month, 1 = once or twice a month, 2 = three or four times a month, 3 = once or twice a week, 4 = three or four times a week or more; “How long do you spend online each time?”, answered in a 0-4 scale, where 0 = less than 30 min, 1 = 30-60 min, 2 = from 1 to 2 h, 3 = more than 2 h, 4 = most of the day. Second section was educational use of the internet, which was based on five items: “Have you ever done any of the following activities related to child-rearing issues? –look for information about early childhood education, look for an online educational game, seek guidance on child development, look for family health-related information, and conduct searches on parenting topics?” to be answered in a 0 (never) to 3 (very often) scale for each category.
Feasibility outcomes
Online course datasheet (all levels). This section evaluated course duration (1 item, “Duration of the activity”), course utility (1 item, “The design of didactic materials has helped me to understand and assimilate contents in an easier way”), course accessibility (1 item, “I found it easy to access and manage activities in the virtual classroom”), satisfaction with the course (1 item, “Overall satisfaction with the course”), by means of a 1-10 scale and dosage (partial completion/total completion).
Face-to-face workshop datasheet (only level 2 and level 3). This section evaluated workshop duration (1 item, “Duration of the activity”), utility (6 items, e.g, “The activity has allowed me to reflect on new objectives of change in my daily life”), accessibility (1 item, “Session schedule”), overall satisfaction (1 item, “Satisfaction with workshop”) by means of a 1-4 scale and dosage (low: l-2 sessions attended, high: 3-4 sessions).
Intervention outcomes
Educational and Health-promoting Activities Inventory (EHAI) (adapted from Acuña & Rodrigo, 1996). Based on the original inventory, we created a 0-3 years old version according to the GH&W programme content. This is a behavioural inventory composed of 15 items and four activity domains with a Likert scale registering the frequency from 1 (never) to 4 (always). First domain, attachment bonds, assessed practices related to emotional expression and responsiveness to child signals and promotion of child's exploring behaviours (3 items, e.g, “We give each other hugs and kisses”). Second domain, feeding, evaluated mealtime habits as a learning opportunity (3 items, e.g, “My child eats with us or see us eating together”). Third domain, physical activity and play, assessed frequency of activities in which parental figures fostered the child's active role and interactions in play situations (6 items, e.g, “We go for a walk to get some fresh air”). Fourth domain, sleeping, evaluated stability and adequacy of the sleeping routine (3 items, e.g, “Before we go to sleep, we do some quiet activity”). Each domain included statements of healthy and unhealthy (reverse scoring) routines.
Me as a Parent (MaaP) (Hamilton et al, 2015). This was translated into Spanish using the forward and backward translation procedure with an expert panel revision following the international guidelines (Acquadro et al, 2009). In a recent review, the MaaP was considered as one of the most appropiate instruments for assessing parental self-regulation perceptions (Wittkowski et al, 2017). It was composed of 16 items with a Likert response scale from 1 (totally disagree) to 5 (totally agree) divided into five factors. Factor 1, self-efficacy (4 items, α = .87), consisted of parents' sense of own effectiveness in overcoming specific parenting problems (e.g, “I have confidence in myself as a parent”). Factor 2, self-sufficiency (4 items, α = .70), consisted of parents' self-confidence in solving problems on their own (e.g, “I know how to solve most problems that arise with parenting”). Factor 3, self-management (4 items, α = .75), consisted of setting a goal, monitoring its attainment and evaluating their own performance (e.g, “I am good at making plans and arranging fun and educational activities for my child to engage in”). Factor 4, personal agency (4 items, α = .50), consisted of parents' locus of control in their child's development (e.g, “How my child turns out is mainly due to luck”).
Satisfaction with Parental Support received in Primary Care (SAPS-PC) (Callejas et al, 2020). This consisted of 14 items assessing the satisfaction with service in four factors, using a Likert scale from 1 (strongly disagree) to 4 (strongly agree). Factor 1, appropriateness of service (4 items, α =.79), evaluated general satisfaction with the service (4 items, e.g, “Overall, I am satisfied with the support we received at the consultation”). Factor 2, collaboration with family (3 items, α =.75), evaluated professional collaboration with the parental figures (e.g, “Professionals understand how I feel”). Factor 3, discontent with the service (4 items, α =.77), evaluated their discontent with the support received (e.g, “I feel that the support I am getting here is not helpful”). Finally, factor 4, parental capacity (3 items, α =.71), evaluated professional practices of prompting parental competences (e.g, “Professionals make me feel empowered as a parent”).
Satisfaction With Family Life Scale (SWFLS) (Zabriskie & Ward, 2013; Spanish version by Caycho-Rodriguez et al, 2018). This consisted of five items (α = .85) assessing an individual's global judgment of family satisfaction on a Likert scale from 1 (strongly disagree) to 7 (strongly agree). The structure was composed of one factor resulting from the sum of all items (e.g, “I am satisfied with my family life”).
Ethical Considerations
The study received approval of the Ethical Committee of University of La Laguna (CEIBA 2017-0258). All primary caregivers and healthcare professionals provided written informed consent to participate.
Intervention and Procedure
The implementation followed the Quality of Implementation Framework standards regarding setting adaptations and readiness, structure organisation, technical assistance, and process evaluation (Meyers et al, 2012). Consequently, the intervention took place in four phases: 1) assignment of centres to the intervention level; 2) training of practitioners according to the intervention level; 3) starting of the intervention; and 4) programme evaluation.
Once the twenty centres had been assigned to intervention levels, a member of the research team set up a meeting with the head of each centre to support the intervention planning. Then, practitioners received specific training according to the intervention level. Practitioners in level 1 centres were given a 30-minute talk introducing the online GH&W programme to promote its use among their patients. Practitioners in level 2 centres received a 5-hour training session on “positive parenting” support principles, online and group GH&W support, and group facilitator skills required to run the workshops. Practitioners in level 3 centres received an extra 2-hour session on the content of individual support. Professionals also had access to an online platform where they could raise queries and review additional training materials, and were offered supervision and had contact with the research team throughout the process. At the end of the experience, practitioners took part in focus groups and gave feedback on the implementation process, as reported in another study in progress. Training and supervision was provided by a psychologist, member of the research team, who had experience in delivering positive parenting programmes and family intervention. The whole process ran from March 2018 to June 2019. For data collection, participants could complete questionnaires using either printed or online forms.
Evaluation Design and Data Analysis
The evaluation followed a cluster randomised control trial design (Brown et al, 2017) to assign centres to the three intervention levels (six in level 1, seven in level 2, and six in level 3). A quasi-experimental design with comparable pre-post groups was used to evaluate the effectiveness of the intervention at each level. Participants completed the online course datasheet (all levels) and the face-to-face workshop datasheet at programme completion.
In preliminary analyses, missing data at item level were extrapolated using missing value analysis. When more than 10% of the items from a questionnaire were missing, the case was excluded from the corresponding analysis. When less than 10% of the data were missing, SEM standard operating procedure was performed to impute data, having checked that data were missing at random using Little's MCAR test.
For the first aim, to evaluate the programme feasibility, ANOVAs and chi-square tests were performed comparing duration, utility, accessibility, satisfaction, and dosage between online course and face-to-face group and individual activities among intervention levels. For the second aim, to explore changes within each intervention level following a variable-centred approach, paired t-tests were performed to examine mean differences between pre-test and post-test measures in health promotion activities, parental self-regulation, satisfaction with the service, and satisfaction with family life. To explore patterns of individual change following a person-centred approach, k-means cluster analyses were performed considering typified change scores of health promotion activities (4 domains), parental self-regulation (4 factors), satisfaction with the service (4 factors) and satisfaction with family life (1 factor). One-way ANOVAs by cluster membership were performed with Bonferroni post-hoc comparisons to examine whether profiles differed significantly in outcome variables. All the variables were standardised to z scores to prevent the different scales from influencing results of analyses. The relationship between cluster membership and intervention level, the sociodemographic profile, and centre area was analysed by means of chi-square analyses with adjusted residuals. This procedure allowed us to identify the cells in which the z scores were greater than +1.96 (higher than would be expected by chance) or less than -1.96 (lower than expected by chance). Statistical analyses were performed with SPSS statistics software, version 25.
Results
Participants' Characteristics by Intervention Level
Participants were mainly mothers, around 34 years old, primiparous, with a healthy child, two-parent family structure, employed, a variety of education levels and living in urban areas. Although there were some differences among users' demographic profiles (e.g, family structure, employment status) recruited in each level, none of them were significant (see Table 1). Furthermore, participants who dropped out of the intervention did not differ significantly except in employment status, χ2(1, 210) = 6.67, p = .01, where the dropout group reported a higher employment rate than the group that completed the intervention. The study retention rate was 41%.
With respect to their internet profile, level 1 participants showed a more intensive use of the internet, with longer connection times and more searches related to early childhood education, educational games, and parenting topics as compared to participants in levels 2 and 3, and more searches related to child development issues compared to level 2 participants (Table 2). There were no significant differences between levels 2 and 3 in any variable.
Feasibility Outcomes and Intervention Level
With regard to the online course, level 2 and level 3 participants reported significantly higher scores of utility and satisfaction compared to level 1. Level 2 participants perceived the course to be more accessible compared to level 1 users. All participants rated the course duration positively. There was no significant difference regarding dosage, with 76% full completion in levels 2 and 3 and 50% completion in level 1. In face-to-face group activities, level 2 and level 3 participants reported similarly high levels of acceptance of workshop duration, activity utility, accessibility, satisfaction, and dosage (Table 3).
Changes in Parental Outcomes within Each Level
Within level 1, participants reported more frequent healthy activities after the programme in two dimensions: attachment bonds and sleeping habits, with medium effect sizes, and they were more satisfied with collaboration with the family at service level, with medium effect size. Participants in level 2 reported significant changes after the programme in three healthy activity domains: feeding, play, and sleeping, with medium and large effect sizes, and reported higher ratings after the programme in self-sufficiency regulation with medium effect size and satisfaction with the parental capacity at service level with medium effect size. Finally, participants in level 3 showed significant differences in almost all dimensions in health promotion activities with medium and large effect sizes, parental self-regulation with medium and large effect sizes, and satisfaction with the service with medium and large effect sizes. There were no significant differences in attachment bonds, discontent with the service, and satisfaction with family life (Table 4). No significant negative change scores were registered at any level.
Table 4. Pre-Posttest Means, Paired t-tests and Effect Sizes (Cohen d) within Each Intervention Level (n = 87).

Note. Effect sizes: small (d = 0.2), medium (d = 0.5), and large (d = 0.8) (Cohen, 1988)
*p < .05, **p < .01, ***p < .001.
Identifying Profiles of Programme Outcomes
Three patterns of change were identified (Table 5), showing significant differences in all variables except in attachment bonds. Cluster 1 was labelled as “initial stage” (n = 36) and was characterised by participants with small negative change scores (reductions in posttest scores as compared to baseline measures) with respect to those in clusters 2 and 3 in health promotion activities (mainly in physical activity and sleeping), small negative change scores in three factors of parental self-regulation and moderate negative change scores in satisfaction with family life with respect to cluster 3, and small positive changes in satisfaction with the service (collaboration with the family and support to parental capacity) with respect to cluster 2.
Table 5. Centre of the Final Clusters and Univariate Contrast of Variances among the Clusters according to Change Profiles (n = 87)
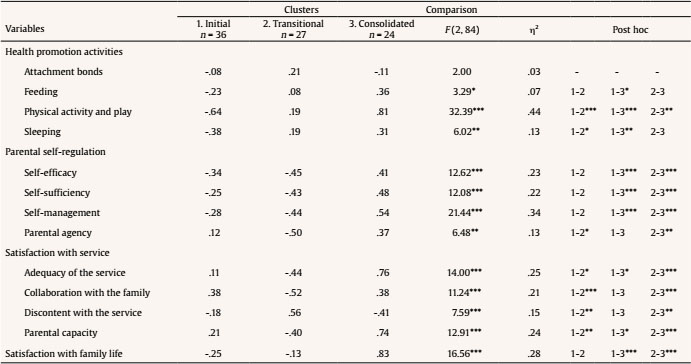
*p < .05, **p < .01, ***p < .001.
Cluster 2 was labelled as “transitional stage” (n = 27) and was characterised by participants with small positive changes in health promotion activities with respect to cluster 1, moderate negative change scores in all factors of parental self-regulation and of satisfaction with the service with respect to clusters 1 and 3, and small negative change scores in satisfaction with family life with respect to cluster 3.
Cluster 3 was labelled as “consolidated stage” (n = 24) and was characterised by participants with positive changes in all dimensions with respect to clusters 1 and 2, moderate and large changes in health promotion activities, moderate changes in parental self-regulation and satisfaction with family service, and large changes in satisfaction with family life.
Cluster Membership Related to Intervention Levels
Participants in cluster 1 were more likely to attend centres assigned to the level 1 intervention. Participants in cluster 2 were less likely to attend centres associated with level 3 intervention. Participants in cluster 3 were less likely to attend centres in level 1 and more likely to attend centres in level 3 (Table 6). No significant differences were found regarding participants' sociodemographic variables and the geographical area of the centre.
Discussion
The present study was designed to provide initial evidence of the feasibility and effectiveness of the universal web-based positive parenting programme GH&W in its hybrid version applied by healthcare professionals in primary care services. The GH&W attracted primary caregivers with a variety of educational levels. This finding represents an extention of the universal reach of the hybrid version when compared to the more selective online version of GH&W, for which a wider national sample found users to be highly educated (Callejas et al, 2018). Other variables of the sociodemographic profile (primiparous mothers, quite experienced with the Internet, living in two-parent families and urban areas) matched well the typical user profile of web-based parenting resources (Dworkin et al, 2013) in which fathers are usually absent (Suárez et al, 2018) and aligned with demographics report on family structure (Instituto Canario de Estadística, 2018).
The programme attracted mainly parental figures highly satisfied with their family life and with a good perception of their children's health. These results contrast with previous studies where parents who took up universal programmes were often less satisfied with their life (Lindsay & Totsika, 2017) and reported lower level of child wellbeing (Heinrichs et al, 2005). However, satisfied and healthy families are also recruited by universal programmes and can be benefited by strengthening their protective factors.
The enrolment rate of participants was lower than expected. Although we do not have information regarding the ones who dropped out, one potential reason is that parents did not expect to receive this kind of support in a primary care setting and consequently did not demand this service at the health centre. This explanation is based on the occasional observation that centres with prior experience with family activities reached larger audiences. Another possibility, based on the dropout profile characterised by families with higher employment rates, is that difficulties related to work-life balance may have acted as a barrier to participation in support programmes for families with young children. However, recruitment problems for universal interventions are common, since families are not part of selective or indicated groups referred by other professionals or services (Lindsay & Totsika, 2017). To overcome adherence issues, reminders and practice assignments have been effective to promote parents' adherence in web-based programmes (Breitenstein & Gross, 2013). Regarding employed parents adherence, occasional comments of professionals pointed out the pertinence of exploring parents' time preferences before running the programme and offering a morning and afternoon shifts as long as it is feasible.
With regard to our first aim of assessing the feasibility of the GH&W hybrid version, findings suggest that the programme was acceptable to parents. Participants who received face-to-face support in centres offering levels 2 and 3 perceived the online course to be more useful and reported a higher level of satisfaction than those in level 1, who were presented with the online course only. Likewise, both level 2 and level 3 participants rated face-to-face workshops as a highly satisfactory resource with useful and accessible activities. The programme duration was rated highly by all the groups, with overall attendance at face-to-face activities being high: most parents attended an average of at least three of the four workshop sessions. Complementary support received at group and individual sessions functioned as an effective scaffolding facilitated by experiential methodology, which made online activities more meaningful and practical, as compared to more directive models, such as simple talks and teaching 'the right way', which were less effective (Rodrigo et al, 2010).
With regard to our second aim of measuring the effectiveness of the GH&W, breaking down the hybrid version into separate intervention levels allowed for a straightforward interpretation of programme changes. Likewise, random assignment of centres to intervention levels and the similar sociodemographic profile of participants across levels reduced the probability of spurious alternative explanations for the results. The main finding obtained, using variable-centred and person-centred approaches, was gradual improvement in programme outcomes associated with the intensity of the intervention, though effect sizes were modest, in line with findings of a recent meta-analysis of brief universal programmes (Leijten et al, 2019). Moreover, participants' low gains in level 1 (dissemination of the online course) was accompanied by a general user profile characterized by more intensive global use of the Internet with longer connection times and higher frequency of educational searches than those of participants in levels 2 and 3, who obtained greater gains. Therefore, participants' greater experience with online educational resources without professional guidance of group and individual supports is not sufficient for rendering more positive results (Myers-Walls & Dworkin, 2015; Suárez et al, 2018). Additional forms of support provided by the GH&W programme prompted participants to set self-proposed goals by linking online content with reflections on their personal experience (Byrne et al, 2014; Lawson & Flocke, 2010).
Concerning health promotion activities, participants in level 1, of whom only half reported full completion of the online course, mainly improved on attachment bonds. It might be the case that they only visited the first module, which dealt with attachment bonds, since people who will drop out tend to do so early in an intervention (McGoron & Ondersma, 2015). By contrast, participants in levels 2 and 3, who were more likely to report full completion of the online course, showed improvements in the other domains (feeding, play, sleeping) involving more socio-cognitive and not only affective parent-child competences.
In relation to parental self-regulation, intensive face-to-face support made a difference, prompting significant changes in all areas, whereas participants who only took the online course did not show changes in perceptions of their competence as parents. Although web-based programmes are able to improve parental sense of competence (Suárez et al, 2018), this effect has been mainly related to participation in forums or to interactions with experts, features that were not available on the GH&W online course. Participants in level 2 perceived themselves to be more autonomous when solving parenting problems, whereas the addition of individual support made participants in level 3 more able to increase their sense of competence and be active in setting goals and monitoring their attainment. In this sense, research has shown that closer, individualised support allows for more meaningful reflections on self-perception of parental role (Rushton et al, 2015).
In relation to satisfaction with the service, participants in level 1 perceived a positive change in the perception of a professional as a collaborator, possibly as a result of being offered the online course as an extra resource available in the service. Participants in level 2 perceived a positive change in the service as a prompter of their parental capacity, in line with increased self-regulation in their autonomy. Finally, participants receiving the most intensive support in level 3 also reported positive changes in general satisfaction with the service, collaboration with the family, and parental capacity. This is a relevant finding indicating that level 3 intervention is closely aligned with the aims of the Family-Centred Care (FCC) model. Finally, satisfaction with family life was not significantly affected by any of the intervention levels, indicating that this is a far-reaching outcome that depends on a wider range of family dimensions (e.g, cohesion, adaptability, communication; Zabriskie & Ward, 2013) that were not directly tackled in this intervention.
A more fine-grained picture of programme effectiveness showed that participants do not all progress in the same way. Three patterns of change were identified corresponding to different stages in the learning process, labelled as “initial”, “transitional”, and “consolidated” stages. Initial stage (cluster 1, 41%) included participants who had not started yet to perform positive changes in health promotion activities and parental self-regulation but reported small improvements in service collaboration with the family and support for parental capacities. Transitional stage (cluster 2, 31%) included participants who began to achieve small positive changes in their health promotion routines but were less confident with their capacities as parents, reported less parental agency and were less satisfied with the service with regard to baseline scores. This is usually the case when parents are becoming more aware of the complexity of the parenting task (Byrne et al, 2014) and adopt a more critical view of the service as they begin to envision the possibilities of a collaborative framework (Callejas et al, 2020). Finally, consolidated stage (cluster 3, 28%) included participants who had performed a more complete process of knowledge building, having accomplished positive outcomes in parents' abilities as health promoters of their child development, increased self-regulation and satisfaction with the service. In future applications, the possibility of extending the number of workshop sessions should be considered to facilitate participants' progression towards this consolidated cluster. Typically, increases in both confidence in parenting capacities and parental self-efficacy were related to positive parenting skills (Albanese et al, 2019). Importantly, patterns of change were related to intervention levels and not to participants' sociodemographic profile or to the centre area, indicating that the type of intervention level makes a difference and revealing the generalisability of its effects. Participants in “initial stage” were more likely to attend level 1 centres, confirming that the online course per se was not so effective. Participants in the “transitional stage” cluster were less likely to attend level 3 centres, as they were distributed between levels 1 and 2. Participants in the “consolidated stage” were more likely to belong to level 3 and less likely to be in level 1, demonstrating that a global improvement was associated with more intensive intervention where individualised support seemed to be the key component.
Some limitations have to be acknowledged despite positive results obtained. First, the final sample size did not allow us to perform a latent profile analysis, which would have yielded more robust evidence of patterns of change in relation to intervention levels. Second, the evaluation relied on self-reported instruments, which are the easiest approach to take in universal settings, but additional measures, such as home observation and online activity record, would have increased the quality of evidence. Third, low study retention rate and lack of information of reasons for dropping out limit the development of tailored solutions to enhance adherence and engagement. Fourth, specific feasibility outcomes were not recorded for individual support, given the need to make intervention compatible with normal operations in a primary care centre, where time is limited and demand is great.
Conclusions
The GH&W hybrid version combining the online course with face-to-face group and individual activities was able to empower parents to become active and self-regulated agents of their child's health status and more satisfied with the service in terms of the FCC model. The hybrid design may help to overcome limitations of web-based EBIs as a universal strategy, and illustrates an affordable way to integrate these interventions into practitioners' regular practice by complementing attention received by families at regular check-ups. Several recommendations can be made to improve future implementation of the programme. First, more effort should be made to increase chances that both mothers and fathers will be similarly involved as mainstream consumers of childrearing content on the Internet. Second, to improve enrolment rate, the impact of wider mass media dissemination, a greater offering of timetables for sessions, and stronger collaborative strategies with other primary care professionals (e.g, general practitioner) and other services (e.g, social services, day care centres) should be tested. Eventually, this programme could also be applied in educational and social services, increasing chances for early prevention of child maltreatment. Finally, to scale up this experience, primary healthcare services should be prepared to efficiently adopt and integrate the GH&W hybrid modality in full into practitioner practices, to improve training provided to healthcare professionals, and to provide enough support for assuring its sustainability in the service. In fact, the evidence provided in this study constitutes the first step that allows considering the GH&W scaling up in all primary care centres in Canary Islands. This experience is also an example of best practice to place universal parenting support, especially for early years, at the forefront of European family policy to be applied across healthcare, educational, and social services.