INTRODUCTION
The growing epidemic of obesity is associated with an increased demand for bariatric surgery to treat this condition. Currently, Roux-en-Y gastric bypass (RYGB) surgery is one of the most widely performed surgical techniques in the world 1. Bariatric surgery is the most efficient treatment for obese patients, resulting in long-term weight loss, and is associated with improvements in health and quality of life in most patients 2,3.
Weight loss success following RYGB surgery occurs due to the combination of restriction of the gastric corpus to a 15 to 30 ml pouch, malabsorption promoted by the derivation of the duodenum and the proximal jejunum, and the change in the basal metabolic rate 4,5. Hormonal mechanisms are also involved in weight loss, such as reduction of ghrelin secretion (an orexigen hormone) and increased secretion of peptide YY and GLP-1 (glucagon-like peptide-1), both being anorexigenic hormones 6,7.
A common definition of successful postoperative outcome is a 50% loss of excess weight, where excess weight is defined as preoperative weight minus ideal weight. Maximum weight loss is usually achieved between 12 and 24 months postoperatively 8.
Although most patients have successful weight loss after bariatric surgery, a small group (20-30%) are unsuccessful in this objective. In this subpopulation, weight recovery tends to begin between 18 and 24 months postoperatively, leading to a decrease or the reverse of improvements in comorbidities and to a decline in quality of life 2.
The factors involved in weight recovery are still not very well elucidated. The literature suggests that they may be related to a higher preoperative body mass index (BMI), to gastric pouch dilatation caused by increased volume intake, and to a sedentary lifestyle 9,10. Another important factor, which may also be related to the failure of weight loss, is the presence of inadequate food habits, such as the high consumption of simple carbohydrates and the low consumption of high protein foods, since patients report more difficulty in ingesting this group of foods, and the consumption of highly caloric liquids and snacks, which lead to a progressive increase in caloric intake 11,12-13.
In view of the above, this study aims to analyze whether feeding behavior, evaluated by caloric intake, and dietary preferences and tolerances, can be considered as determinant factors of weight loss results in obese patients submitted to RYGB surgery.
MATERIAL AND METHODS
This is a cross-sectional study with retrospective and prospective data, approved by the Research Ethics Committee of the Onofre Lopes University Hospital (HUOL) under number 30955114.1.0000.5292. Prior to inclusion into the study, all participants signed the informed consent form.
The research was conducted with patients undergoing RYGB laparoscopic surgery, from the Obesity Surgery and Related Diseases Department (SCODE) at the HUOL, Federal University of Rio Grande do Norte (UFRN), in the Northeast of Brazil. The patients were submitted to surgery according to the criteria established by the Brazilian Ministry of Health.
Data collection was performed at the SCODE nutrition department, in routine visits, from 2015 to 2016, and preoperative data, weight, height, and preoperative BMI, as well as the minimum BMI attained and its respective postoperative time, were collected retrospectively from the patients' charts.
One hundred and five patients of both sexes were included in the study, aged between 18 and 70 years, and registered in the SCODE, with preoperative BMI of ≥ 35 kg/m² and at least two years postoperative, operated between 2006 and 2014. After the data collection, the patients were divided into two groups: the success group (64 patients), who had ≥ 50% of excess weight lost (EWL), and the failure group (41 patients), who had ˂ 50% EWL. EWL was calculated by dividing the weight loss (kg) by weight excess (preoperative weight minus ideal weight) and multiplying the result by 100.
Participants were weighted on a digital scale and had their height measured on a stadiometer (both from Filizola, São Paulo, Brazil). Obesity was defined according to the World Health Organization (WHO) classification and based on BMI, defined as body weight (kg) divided by the square of height (m).
Patients diagnosed with psychiatric illness, pregnant women, patients with complications that could lead to food intolerance, such as stenosis, and other surgical procedures that could lead to weight loss were excluded from the study.
At the time of the consultation, a validated and structured questionnaire was applied to assess the existence and degree of food tolerance 12. Average calorie, micronutrients and diet composition were calculated by the Avanutri (Três Rios, RJ, Brazil) software, and as an instrument for data collection for this analysis, a 24-hour dietary recall was applied, where the patients reported all food and drink consumed during the day before the interview, with their respective home measurements. Also, for this analysis, a three-day food record was applied, where participants were advised to record all food and drink consumed and their respective home measurements on three sheets of paper (one for each day), with times and distribution of meals throughout the day. For the analysis of macro and micronutrients, the use of supplements was not considered.
For food preference evaluation, the qualitative food frequency questionnaire (QFFQ) was applied. The participants reported the average habitual frequency of consumption of each item, by its respective unit of time (times/week). For this study, the frequency of consumption of fruits, vegetables, fried foods, desserts and simple carbohydrates (CHO) (bread, pasta, rice, biscuits, potatoes and flour) was analyzed.
Practitioners of physical activity were those considered doing a minimum of 150 minutes per week, according to the WHO recommendation 14.
The Stata 11 program (Stata Corp., College Station, TX, USA) was used for statistical analysis. The Student's t-test was used to compare demographic, anthropometric and nutritional variable averages. For food journal record analysis, the three day record average was used. The Chi-square test was used to compare the proportion of subjects who practiced physical activity, and the Mann-Whitney test was used to compare the weekly consumption amount of the food groups. The significance level adopted was p < 0.05.
For multivariate analysis, a stepwise backward logistic regression model that included all variables that have shown some evidence of association with the dependent variable in a univariate analysis at the p < 0.15 level was used. The final model retained only those variables significant at the p < 0.05 level. Results are presented as odds ratios with 95% confidence intervals.
RESULTS
Of the total of 105 patients, 84% were female and 16% were male. The mean age of the participants was 43.3 ± 11.4 years in the success group (n = 64), and 43.4 ± 10.7 years in the failure group (n = 41) (p > 0.99). The analysis showed no influence on the final weight loss result of the mean preoperative BMI comparison. The success group presented a mean of 48.8 ± 8.36 kg/m², and the failure group 49.9 ± 6.93 kg/m² (p = 0.47).
There was no statistically significant difference in mean postoperative time between the success group (47.9 ± 25.0 months) and the failure group (56.2 ± 26.9 months) (p = 0.11). There was a statistical difference in relation to minimum BMI achieved by the groups (p < 0.001), and in the period of time they achieved this minimum BMI (p = 0.01), as the failure group demonstrated to cease losing weight earlier than the success group, as we can observe in Table 1.
Table I. Characteristics of the study population
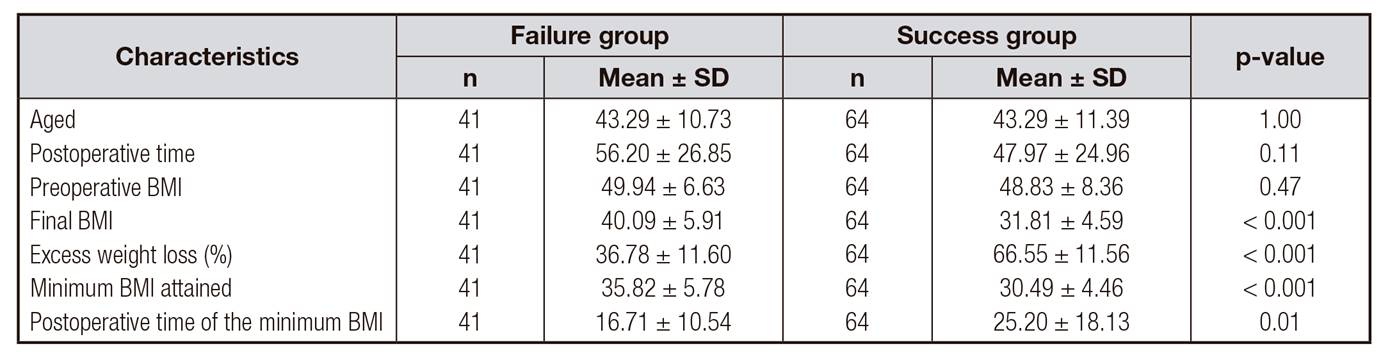
BMI: body mass index. Failure group: patients with EWL < 50%. Success group: patients with EWL ≥ 50%. Postoperative time: months. Data are presented as mean ± standard deviation.
The analysis of mean caloric intake showed no significant difference between the groups (R24h, p = 0.27) (food journal record, p = 0.95) (Fig. 1), as well as in the diet composition (Table 2). The frequency of weekly consumption of desserts was twice as high in the success group as in the failure group (Table 3).

Figure 1. Comparison of caloric intake between groups. Failure group: patients with EWL < 50%. Success group: patients with EWL ≥ 50%.
Table II. Analysis of diet composition

Failure group: patients with EWL < 50%. Success group: patients with EWL ≥ 50%. Data are presented as mean ± standard deviation.
Table III. Frequency of weekly consumption per food group
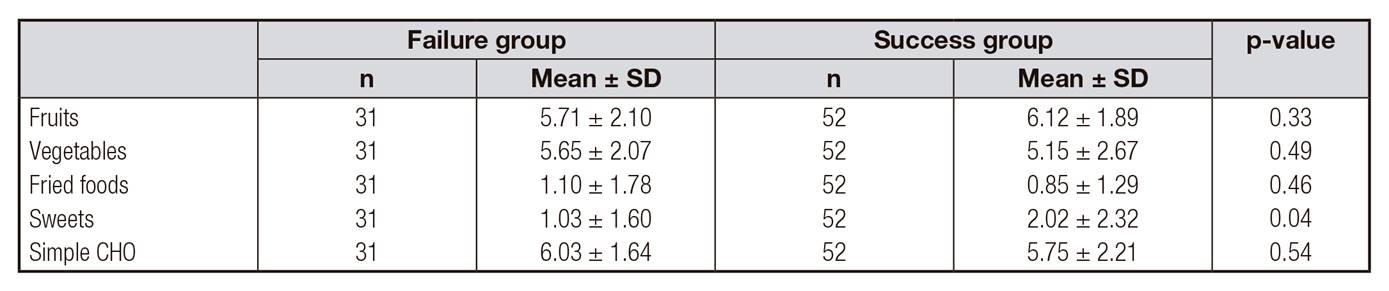
Simple CHO: bread, pasta, rice, biscuits, potatoes and flour. Failure group: patients with EWL < 50%. Success group: patients with EWL ≥ 50%.
The groups presented a good degree of food tolerance, the success group with a score of 22.9 ± 3.40 and the failure group with 22.5 ± 2.52, (p = 0.88). Only two patients in the success group reported daily vomiting (Fig. 2).
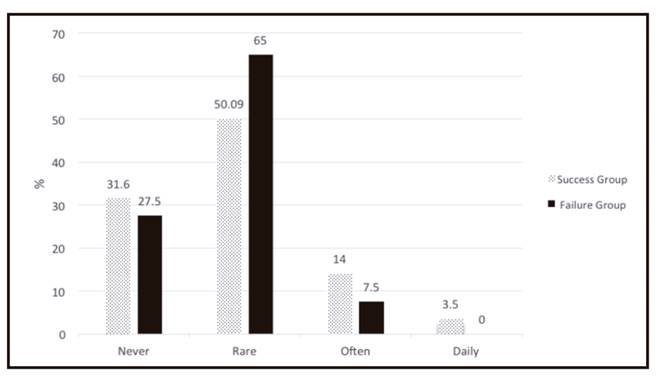
Figure 2. Occurrence of regurgitation and vomiting among participants. Failure group: patients with EWL < 50%. Success group: patients with EWL ≥ 50%.
Only 18 patients from the success group (34%) performed physical exercise, and ten patients (32.3%) from the failure group (p = 0.87).
In multivariate analysis, the initial model included all the following variables: postoperative time, final BMI, minimum BMI attained, postoperative time of the minimum BMI, maximum EWL%, carbohydrate (24-hour dietary recall) and B12 vitamin (24-hour dietary recall). In the final model (Table 4), a lower final BMI was associated with weight loss success (OR 0.264, p < 0.001). In subjects with the same final BMI, a higher minimum BMI attained (OR 4.851, p < 0.001) and a higher maximum EWL% (OR 1.515, p < 0.001) were associated with greater likelihood of weight loss success.
DISCUSSION
Weight regain among patients after bariatric surgery is already a known fact among researchers. Some studies have shown that it usually occurs after the second postoperative year 15.
The literature suggests that low postoperative dietary adherence is increasingly and consistently identified as a predictor of poor results of weight loss after surgery 16. However, our study did not find the same result since there was no statistical difference in the average amount of calories consumed daily and diet quality in the studied groups.
Wardé-Kamar et al. 17 performed a study with 69 patients with a mean duration of 30 ± 8 months postoperative of RYGB, and observed a weight loss at the time of the study of 48 ± 17 kg (4 to 114 kg), with a %EWL of 58 ± 17%. It was also observed that 61% of the patients were successful in postoperative weight loss. Diet composition analysis showed that 22 ± 6% of the total calories were protein, 44 ± 11% were carbohydrates and 33 ± 11%, fat.
In relation to carbohydrate consumption, we observed a higher percentage of consumption than the Wardé-Kamar et al. study. 17. However, there is still no consensus regarding the macronutrient standard to be followed for healthy weight loss after bariatric surgery 18.
Comparing successful and unsuccessful weight loss patients, one study found that patients with %EWL ≥ 50% consumed fewer calories than patients with %EWL < 50%, although this was not significant (1,657 ± 649 kcal vs 1,888 ± 600 kcal , p = 0.24) 17, corroborating our study.
Another study in patients with a mean of 4 ± 1.43 years postoperative reported that they had a daily calorie consumption of 1,885 ± 412 kcal 16.
Sjostrom et al. 19 also suggest that energy intake may influence weight regain. They reported a mean daily intake of 2,900 kcal, 1,500, 1,700, 1,800, 1,900, 2,000 kcal/day: pre-surgery, six months, one year, two years, three years, and between four and ten years post-surgery, respectively.
Post-RYGB patients eat less and feel less hungry. These changes may represent a superior efficacy in weight loss compared to other surgical procedures. The exaggerated release of intestinal hormones (PYY and GLP-1) post-RYGB has been suggested as a potential mediator in changes in food preferences and weight loss. Their anorexigenic properties are already being explored to treat obesity 20. Changes in appetite are already evident a few days after surgery, since postprandial PYY and GLP-1 levels already begin to increase two days after the operation, and they influence appetite reduction, which explains the lower intake of calories and the weight loss.
In patients with unsuccessful weight loss, postprandial PYY and responses to GLP-1 are attenuated in comparison to patients with good postoperative weight loss. Inhibition to respond to intestinal hormones, including PYY and GLP-1, after gastric bypass results in the return of appetite and increased food intake 20,21-22. This fact may justify the increase in food intake and the weight regain in many patients.
The literature suggests that preoperative BMI can be considered as a predictor of failure of surgery 23. However, in our study, no difference was observed between the groups in relation to initial BMI, corroborating with a study by Shantavasinkul et al. 24, who reported that preoperative BMI is not a predictor of postoperative weight regain. This same study observed that patients who ceased to lose weight earlier, on average one year postoperatively, presented weight gain. Our study also found this association, demonstrating that the patients in the failure group reached their minimum weight with a mean of 16 months postoperative, long before the patients in the success group, who reached minimum weight with a mean of 25 months postoperative.
In our study, we found no difference between people who do physical activity, and weight loss, even though it is an important factor in maintaining weight loss. This finding is in agreement with a study by Faria et al. 25, who observed that only 20% of the sample practiced physical activity, and found no correlation with weight loss. However, the use of different tools to evaluate physical activity makes it difficult to compare studies. The literature reports that higher levels of physical activity, which were not observed in our study, may be effective in improving and maintaining weight loss 26,27-28.
Patients undergoing bariatric surgery may present difficulties in dietary adaptation after surgery 11,29. In a study conducted by Pedrosa et al. 30, the occurrence of food intolerance in 205 patients submitted to RYGB was analyzed, and it was observed that vomiting was the main symptom associated with food intolerance. Valezi et al. 31 investigated the degree of food preference and tolerance according to the gender of patients after bypass, and observed that the only significant result was in relation to fruit consumption, which was higher among women. In our study, fruit and vegetables consumption was similar between groups, with a mean weekly consumption of 5.71 ± 2.10 in the failure group and 6.12 ± 1.89 in the success group (p = 0.33). A study by Wardé-Kamar et al. 17 showed that fruit and vegetables consumption reached approximately 180 kcal per day, which is equivalent to two servings of fruit and 2-3 servings of vegetables per day. This same group further reported a consumption of sugary drinks which corresponded to 7% of total calories consumed. In our study, the consumption of desserts was twice as high in the success group, not presenting an association with the final result of weight loss.
The elevated consumption of simple carbohydrates, and low consumption of dietary sources of protein, can be associated to unsuccessful results, since this last group of foods is considered to be difficult to ingest by the patients 11. In our study, patients presented a good dietary score 32 and reports of daily vomiting occurred in only 3% of the patients in the success group, corroborating the study by Godoy et al. 32. Furthermore, in a study conducted by Wardér-Kamar et al. 17, it was observed that 62% of the patients had spontaneous vomiting and 27% induced vomiting.
Dietary protein may influence some factors in the regulation of body weight such as satiety 33, energy expenditure and body composition 34. The patients in our study presented adequate protein intake, being greater than the established in the guidelines of the American Association of Clinical Endocrinologists, the Obesity Society, and the American Society for Metabolic and Bariatric Surgery that recommend at least 60 g of protein per day and up to 1.5 g/kg of ideal weight per day 35.
In a systematic review by Ito et al. 36, four studies were found where the patients had a protein intake lower than 60 g/day and significant loss of lean mass. Another study, with patients with a mean of 30 months postoperatively, reported a mean protein intake of 1.7 g/kg of ideal weight/day 17. Raftopoulos et al. 37 suggest an association between low protein intake and low lean mass, and report that a daily intake of protein greater than 1 g/kg per day is feasible and may provide benefits in increasing weight loss, reducing body fat and improving lean mass 37. This corroborates the present study, which suggests that a greater amount of daily calories originating from proteins may be related to greater weight loss 25.
There is no data in the literature that accurately evaluates the postoperative period of RYGB 38. This can underestimate the amount of food consumed by this population, since patients do not usually report their actual intake, which can imply a false result, reaching a variation of 20% to 50% in the total calories consumed 39 . Another limitation of the study was the non-standardization of the RYGB surgical technique due to the improvement of surgical technique over the years, change in size of the gastric pouch and of intestinal deviation.















