INTRODUCTION
Cardiovascular diseases (CD) are a common cause of mortality and morbidity in the world 1. According to the World Health Organization (WHO) data, an estimated 17.7 million people died from cardiovascular diseases in 2015, representing 31% of all global deaths 2. Evidence shows that dietary and lifestyle factors are the most important determinants of mortality and morbidity among CD 3. Further, unhealthy dietary habits and lifestyles that affect physical and psychosocial health are known as risk factors for the development of life-threatening diseases 4. Several cohort studies have shown that greater adherence to the Mediterranean diet is associated with lower mortality 5,6. Furthermore, few studies have been published about the effect of the diet on the health related quality of life (HRQL) 4,7,8.
Mediterranean diet (MD) has shown a significant beneficial effect on human health over the last 50 years 9. The most common features of the MD include high amount of whole grains, fresh vegetables and fruits, legumes; olive oil as a source of fat; fish, poultry, milk products, eggs and moderate amount of wine and low amount of red meat 10. In a meta-analysis study, greater adherence to the MD was associated with a reduction in metabolic syndrome, type 2 diabetes mellitus (DM), hypertension, heart diseases, systemic and chronic inflammation, risk of cancer and a healthier and a longer life 11,12,13.
In addition, as the incidence of chronic diseases has increased with globalization, quality of life has been affected negatively 14. The short form of quality of life (SF-36) was reported to be used to evaluate the quality of life as a determinant of medical treatment states and follow-up of the patients 15. There are many studies evaluating the HRQL of participants with cardiovascular diseases and obesity, as well as other chronic diseases 16,17,18. However, in the literature, there has not been adequate study to evaluate HRQL and Mediterranean diet 4,7,8. The aim of this study was to assess the relationship between MD adherence and HRQL and anthropometric measurements in coronary artery disease patients.
MATERIALS AND METHOD
PARTICIPANTS
This cross-sectional study was carried out in 55 females (over 50 years) and 84 males (over 40 years) who were diagnosed with coronary artery disease in Ankara, Turkey. The patients with a history of coroner artery stenosis (diagnosed by coronary angiography imaging by a cardiologist) were included in the study. The data on the patient demographics (educational level, smoking and alcohol use, coronary artery disease history in the family) was collected through face-to-face interviews by the researchers. Participants were excluded if they reported a personal chronic disease (except type 2 diabetes, dyslipidemia and hypertension); pregnant and lactating women and patients with pacemaker were also excluded. The sampling was performed from February to December 2016. The study procedures were approved by the Ethical Commission of the University of Gazi in meeting number 77082166-604.01.02 (on January 13th, 2016) and were carried out in accordance with the Declaration of Helsinki (1989) of the World Medical Association. All participants were informed about the aims of the study and provided a written informed consent.
PROCEDURES
Adherence to the Mediterranean diet
Mediterranean diet was assessed with a 14-item questionnaire of Mediterranean diet adherence, which was developed by Schröder et al. in 2011 19. Each question was scored either 0 or 1 point. The adherence to MD was evaluated after being diagnosed of CAD.
Health-related quality of life
The most commonly used tool to evaluate HRQL is the SF-36 survey. The assessment is based on the last four weeks of the participants. This questionnaire contains 36 items, which consist of eight multi-items including physical function, physical role, pain, general health, emotional role, mental health, social function and vitality. The first four items are considered in the physical health score and the last four items are considered in the mental health score 20. For each parameter, scores are coded, summed and transformed to a scale from 0 to 100. Higher scores suggest better functioning.
ANTHROPOMETRIC MEASUREMENTS, BODY COMPOSITION AND BIOCHEMICAL MEASUREMENTS
Anthropometric measurements (body weight [kg], height [cm], neck [cm], waist and hip circumference [cm]) and body composition of all participants were measured in accordance with the techniques by the WHO 21). Body composition (lean body mass [kg], percent of body fat and body water [%], fat free mass [kg]) was measured through a Tanita® BC 532N. The body mass index (BMI) was calculated through the following formula: BMI = body weight (kg) / height (m2). Waist/hip and waist/height ratios were also calculated. The BMI values of the participants were classified into three categories according to WHO classification: underweight (<18.5 kg/m2), normal weight or healthy (18.5-24.9 kg/m2), overweight (25.0-29.9 kg/m2), and obese (≥30.0 kg/m2) (25).
Routine biochemical parameters, serum lipid profiles (total cholesterol, LDL, HDL, triglycerides) and fasting blood glucose levels of the participants during the last three months were recorded from the hospital records retrospectively.
STATISTICAL ANALYSIS
Statistical analyses were performed using SPSS 22.0 (Chicago, IL) software. The variables were investigated using visual and analytical methods (Shapiro-Wilk test) to determine whether or not they were normally distributed. Descriptive values were given as number (n), percent (%), mean (x), standard deviation (SD), median and interquartile range (IQR). The continuous variables were not normally distributed (non-parametric tests) and the Mann-Whitney U test was used to compare means. Non-parametric Spearman's rank correlation analysis was performed to determine the relationship between numerical variables. A p-value of less than 0.05 was considered to show a statistically significant result.
RESULTS
The present study included 139 participants, whose mean age was 63.0 ± 9.7 years for males and 63.1 ± 10.1 years for females. Diabetes, dyslipidemia and hypertension incidences were lower in male participants (39.3%, 44.0% and 64.3%, respectively) than in female participants (69.1%, 63.6% and 81.8%, respectively) (p < 0.05). Also, 22.6% of all the male participants were smokers versus 5.5% of female participants. An educational level longer than eight years was found in 59.5% of male participants and in 10.9% of female participants. Both smoking habits and educational levels were statistically significant according to gender (p < 0.05) (data not shown).
Anthropometric measurements and body compositions of participants by gender are given in Table 1. According to BMI classification, 6.0%, 53.5% and 40.5% of male participants were normal, overweight and obese, respectively; whereas 1.8%, 14.5% and 83.6% of female participants were normal, overweight and obese, respectively (data not shown).
Table I. Anthropometric measurements and body compositions of participants by gender

BMI: body mass index; IQR: interquartile range.
Some biochemical parameters and the MD adherence of participants by gender are shown in Table 2. Fasting blood glucose, HDL and total cholesterol levels of female participants were found statistically higher than those of male participants (p < 0.05). Adherence to the MD was assessed and the median values were found statistically higher in male participants (p < 0.05) (Table 2).
Table II. Adherence to the Mediterranean diet
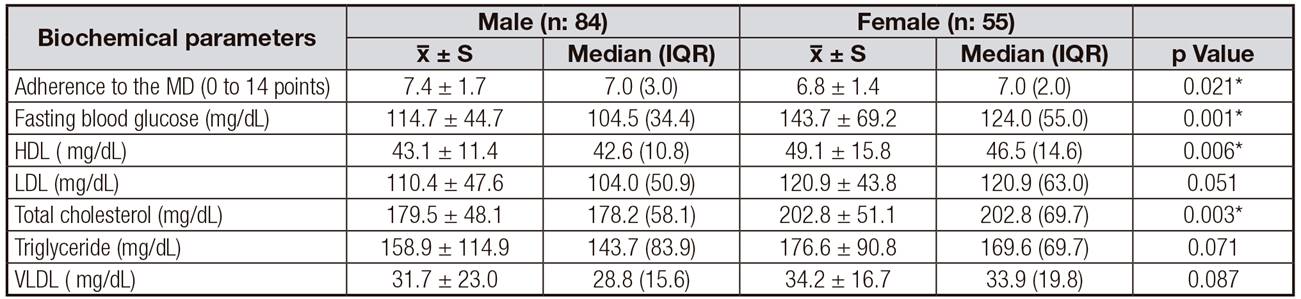
IQR: interquartile range; MD: Mediterranean diet; HDL: high density lipoprotein; LDL: low density lipoprotein; VLDL: very low density lipoprotein.
*Significance was calculated with the Mann-Whitney U test for ordinary data analyses participants according to gender expressed median. p < 0.05.
Physical component summaries (PCS), mental component summaries (MCS) and the subscales of SF-36 of participants by gender subscale are shown in Table 3. The median values of the component summaries (PCS, MCS), PF, PR, Pain, GH, ER, MH,SH and vitality in the male participants were significantly higher than the female participants (p < 0.05).
Table III. Physical component summaries (PCS), mental component summaries (MCS) and the subscales of SF-36 participants

IQR: interquartile range; ER: emotional role; GH: general health; MCS: mental component summary; MH: mental health; PCS: physical component summary; PF: physical function; PR: physical role; SH: social health.
*Significance was calculated with Mann-Whitney U test for ordinary data analyses of the participants according to gender. p-value: a< 0.001; b< 0.01; c< 0.05.
The correlation between component summaries (physical, mental) and the subscales of the SF-36, adherence to the MD scores and anthropometric measurements-body composition was presented in Table 4.
Table IV. The correlation between component summaries (physical, mental) and the subscales of the SF-36, adherence to the MD scores and anthropometric measurements-body composition

BMI: body mass index; PCS: physical component summary; PF: physical function; PR: physical role; GH: general health; MCS: mental component summary; ER: emotional role; MH: mental health; SH: social health; MD: Mediterranean diet. The Spearman's rank correlation coefficient test was performed. p-value: a< 0.001; b< 0.01; c< 0.05.
With regard to PCS and antropometric measurements-body composition were not correlated between the groups both male and female (except: waist/height ratio and PCS were correlated in female). In male, PF was found negatively correlated with waist circumference and waist/height ratio. In female, the negative association between the PR and BMI, in addition, pain and waist/height ratio were found. Generally, among subscales of SF-36 and antropometric measurements-body composition significant correlation were found as a unique sample not dividing according to gender. The association between PCS scores, its subscales (except GH and FR), MCS of the participants and waist circumference (cm), BMI (kg/m2), waist/height ratio and body fat (%) were found negative, whereas a positive significant correlation was found between the aforesaid scores and percent of body water, as well as the fat free mass (kg) (p < 0.05) for all participants. A negative correlations were found between ER and waist/height ratio, percent of body fat. MH were negative correlated with BMI, waist/height ratio, percent of body fat (p < 0.05). A significant negative correlations were found between SH and waist circumference, BMI, percent of body fat. Vitality scores were negatively correlated with waist circumference, BMI, waist/height ratio and percent of body fat; positively correlated with fat free mass.
When anthropometric measurements were assessed by age, gender and educational level, considered to affect the physical component summary, the R2 value of the model was 0.46 and it was statistically significant (p < 0.05).
The physical health score was found lower especially in female participants (β = -0.504), low educated participants (β = 0.287) and the participants with higher neck circumference (β = -0.193). No correlation was found between HRQL of the participants and biochemical parameters (p > 0.05) (data not shown).
The association between adherence to the MD and SF-36 was shown in Table 5. In terms of gender, the relationship between physical function and adherence to the MD were found only in female participants (r = 0.261; p = 0.018). Adherence to the MD of the participants was positively correlated with PCS (all subscales) and most MCS (except emotional role, social health subscales) (p < 0.05). However, no gender-based association was found (p > 0.05). No statistical association was found between adherence to the MD and biochemical parameters either based on gender or not (p > 0.05) (data not shown).
Table V. Association between adherence to the MD and SF-36
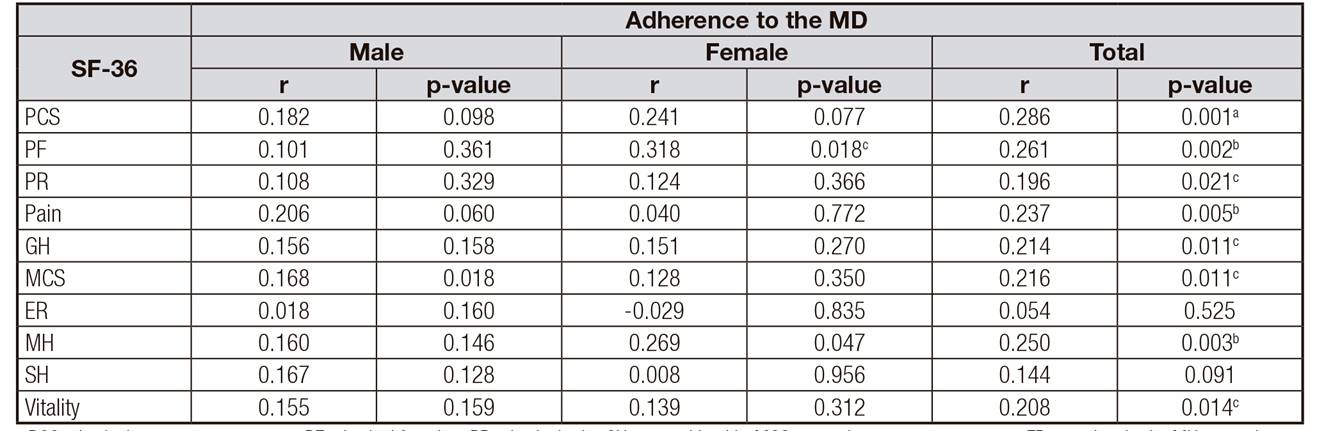
PCS: physical component summary; PF: physical function; PR: physical role; GH: general health; MCS: mental component summary; ER: emotional role; MH: mental health; SH: social health.
*The Spearman's rank correlation coefficient test was performed. p-value: a< 0.001; b< 0.01; c< 0.05.
DISCUSSION
The relationship between MD and HRQL in the literature has generally been examined in epidemiological studies. However, adherence to the MD can be associated with survival and mortality. Therefore, in this study, the effect of MD on HRQL was examined in patients diagnosed with coronary artery disease.
The MD, in particular, is associated with a reduction in the risk of developing cardiovascular diseases 22. A systematic review reported that MD reduces the risk of cardiovascular disease by 8% to 45% in patients with acute myocardial infarction 23. Another study associated each one-point increase in adherence to the MD with a reduction in myocardial infarction risk by 18% 24. In a study conducted in 110 individuals with cardiovascular disease, the mean score of adherence to the MD was 9.3 25. In our study, the median value of adherence to the MD score was lower than the aforesaid value by 7.0, both in male and female participants; however, adherence of male individuals was higher (p < 0.05). Although adherence to the MD is generally low, a study conducted in Turkey indicates similar results with this study, with higher adherence to the MD in male individuals (21%) than in female individuals (19%) 26.
To the best of our knowledge, the present study was the first to investigate the associations between adherence to Mediterranean diet (MD), HRQL and anthropometric measurements in the patients with coronary artery disease. One of the key findings of the present study is that a direct linear association was found between adherence to MD and all physical and most mental quality of life. Consistent with this finding, a greater adherence to the MD was associated with better HRQL in cross-sectional studies conducted in Spain and Greece 8,27. Particularly, in a study conducted in Spain 8, a significant direct association was observed between adherence to Mediterranean diet and all the physical and most mental health domains (vitality, social functioning and emotional role). In a Greek study (27), a positive association between adherence to the Mediterranean diet and self-reported mental and physical health status was observed. The association is more obvious for mental than for physical health. By contrast, another study in Spain 28 assessed the association between Mediterranean diet and HRQL in two prospective cohorts of old-age individuals. The UAM-cohort was used to develop an eight-item index of Mediterranean diet (UAM-MDP). The Seniors-ENRICA cohort Mediterranean diet adherence was measured with the PREDIMED score and the Trichopoulou's Mediterranean Diet Score (MSD). In the UAM-cohort, no significant associations between the UAM-MDP and the PCS or the MCS were found. In the Seniors-ENRICA cohort, a higher PREDIMED score was associated with a slightly better PCS. when compared with the lowest tertile of the PREDIMED score. However, the PREDIMED score was non-significantly associated with a better MCS score. The MSD did not show an association with either the PCS or the MCS. The SUN project study concluded that a directly linear association is present between physical-mental health and MD, and this association is particularly stronger in physical health. Thus, the discrepancies between the present study and previous studies in relation to the observed correlations between adherence to MD and HRQL were hypothesized to be due to the consumption of different food groups, different age groups, population-specific preferences and socioeconomic status. The relation between quality of life and diet was associated with consumption of healthy food or nutrients with lower quantity and mental-physical health. In this study, both low adherence to MD score and the low quality of life scores may explain the correlation between them.
Our study demonstrated that the mean and median value of adherence to the MD score in male was significantly higher (respectively 7.4 ± 1.7 and 7.0 (3.0)) than female (respectively 6.8 ± 1.4 and 7.0 (2.0)) (p < 0.05). Although adherence to the MD is generally low, a study conducted in Turkey indicate similar results with this study in terms that higher adherence to the MD in male individuals (21%) than female individuals (19%) 28. Greater adherence to a Mediterranean diet is associated with a significant improvement in health status, as seen by a significant reduction in overall mortality, mortality from cardiovascular diseases (14). A systematic review reported that the MD reduce the risk of cardiovascular disease by 8% to 45% in the patients with acute myocardial infarction 29. Another study associated each increase of one point in adherence to the MD with a reduction in myocardial infarction risk by 18% (30). A study conducted on 110 individuals, aged between 55 and 80 years, who were diagnosed with CAD, the mean score of adherence to the MD (14-items) was found 8.9 31. Consequently, we can say that little increases adherence to the MD score is a great importance in protection against CAD and quality of life.
Although the effect mechanism remains unclear, another essential component of HRQL is obesity 29. The second objective of this study was to study the association between HRQL and anthropometric measurements-body composition in coronary artery disease patients. In this study, HRQL scores (all subscales) of males were higher than those of females. In females, the higher prevalence of obesity (86%), dyslipidemia, hypertension, diabetes mellitus, median values of some anthropometric measurements (waist circumference, hip circumference, waist to hip circumference, BMI and percentage of body fat) and the lower MD scores can be attributed to the lower HRQL scores in comparison with men. Some studies found a negative association 30 or no association between BMI and mental health scores 31. A meta-analysis study which assessed the BMI and HRQL in adults reported that mental health scores of moderately overweight individuals are significantly higher than those of normal individuals; in addition, third grade obese individuals presented lower mental health scores. The same study found significantly lower physical health scores in individuals with higher BMI values 32. In the PreCIS study, a negative correlation was observed between physical-mental health scores and BMI-waist circumference 15. The majority of the studies associate higher BMI with bad physical function 33. Our data agree with previous findings in that inverse significant associations were found between BMI, waist circumference, waist/height ratio, percent of body fat and both physical and mental health scores (including subscale). Although coronary artery diseases are given as a more important mortality risk for men in the world, the increase in obesity and low educational level negatively affect the physical health components, especially in women, as seen in this study. No correlation was found between HRQL and biochemical parameters (p > 0.05). Further, there was no statistical association between adherence to the MD and biochemical parameters, either based on gender or not (p > 0.05) (data not shown). This can be attributed to questioning the short term.
CONCLUSION
In our study, we found that adherence to the MD may be associated with better mental and physical health in the participants with coronary artery disease in Turkish population. Furthermore, a significant association was found between physical and mental health state and anthropometric measurements.
The adoption of healthy dietary habits by the participants is considered as a possible contributor in both improvement of biochemical parameters and achievement of desired results in anthropometric measurements. Moreover, mortality related to coronary artery disease can be significantly reduced in patients highly adhered to MD. Further studies are needed to prove the long term effectiveness of this nutritional regimen in coronary artery disease. The present study outcomes will contribute to new evidence for the health benefits of the MD and may encourage public health policymakers to promote this dietary pattern.
LIMITATIONS
This study has some limitations. It only includes people who are living in central Anatolia, therefore it does not reflect the whole of Turkey. Consequently, further homogeneous and large studies which represent all society are needed. As the population of this study consisted of young consumers from central Turkey, the results cannot be generalized for all coronary artery disease patients or all ages. Performing the study in a large sample of patients would be useful.














