INTRODUCTION
Systemic arterial hypertension (SAH) has a high worldwide prevalence (1). In Brazil, a study conducted with adults in Brazilian capitals reported SAH in 24.50 % in 2019 (2). There is evidence in the literature that SAH prevention, as well as diabetes, considerably reduces the risk of developing cardiovascular diseases (CVD) (3). Thus, a simple and low-cost method, such as anthropometric measurements and indices, could be used as an important cost-effective strategy for screening SAH in primary care.
As obesity plays an important role in the etiology of SAH, the use of body adiposity indicators can assist in its identification in individuals with excess body adiposity (4). Among the various measures described in the literature, body mass index (BMI) and waist circumference (WC) are well documented as SAH indicators (5,6). Nevertheless, some limitations must be considered regarding the use of these measures, such as the inability of BMI to discriminate body composition differences taking into account sex and ethnicity (7), since body adiposity degree may not be the same in different individuals (8), and the fact that WC does not consider height, since there is evidence of an inverse association between height and health risk (9).
Other indicators have been used to verify the predictive capacity of SAH compared to BMI and WC (4,10-13), such as the waist-to-height ratio (WHtR) (4,11), waist-to-hip ratio (WHR) (4,11), body adiposity index (BAI) (11,14), and neck circumference (NC) (12), among others. Despite the wide use of these indicators, some limitations should be highlighted: for example, the fact that WHR has specific cutoff points for different ethnic groups and sex (15). On the other hand, a meta-analysis published in 2012 (10) showed that WHtR is better for the identification of cardiometabolic risks when compared to BMI and WC, despite being questioned for having a single cutoff point to classify different groups (16).
Due to the limitations presented by body adiposity indicators, new indexes have been proposed seeking to identify a simple and easy-to-use equation for clinical and epidemiological purposes. In this sense, a new equation has been recently proposed to assess body fat, namely Relative Fat Mass (RFM) (17). This equation was based on the height/waist ratio, creating a linear equation as a way to estimate fat percentage in adult individuals of both sexes. The validation of RFM was performed for the American population and did not involve its relationship with cardiovascular diseases, which reinforces the need to verify the response of this indicator in other populations, and its predictive capacity in comparison to other indicators of body adiposity for SAH.
Thus, the need to verify the response of new body adiposity indicators is justified, as well as the need to compare their effectiveness in relation to indicators already consolidated in the literature. According to the World Health Organization (18) there is a constant need to monitor risk factors for chronic non-communicable diseases, especially those that have a greater impact on morbidity and mortality from chronic diseases worldwide, and that can be modified in primary health care. Therefore, the aim of this study was to analyze the predictive capacity of the new body adiposity index, RFM, for high blood pressure levels and to compare it with indicators already consolidated in the literature such as BMI, BAI, WC, NC, WHR and WHtR.
METHODS
STUDY POPULATION
This is a cross-sectional study based on the “Cardiovascular Risk Factors In University Students” study, developed in a private higher education institution. All students regularly enrolled in the institution in 2017 and the first semester of 2018 were eligible.
The sample size was calculated using the Epi-Info software, considering: reference population of 1,800 college students; estimated prevalence of 24.50 % (2), expected sampling error of 3.50 %; effect of study design estimated at 1.6, to which was added 10 % relating to losses or refusals and 10 % for the control of confounding factors, yielding a final sample of 845 individuals. The final data included 896 subjects in the age group of 18-40 years.
MEASUREMENTS
Assessment of blood pressure
Blood pressure was measured on a single occasion with two measurements, with a 10-minute interval between measurements, with the individual sitting for at least 5 minutes and according to Brazilian recommendations (19). When the difference between the first and second measurements showed values greater than 10 mmHg, a third measurement was performed and the average of the two closest values was recorded. An automatic wrist sphygmomanometer (Omron HEM 629), duly calibrated, was used. Values obtained after the two measurements were summed up and the average of the readings was recorded. Individuals with systolic blood pressure (SBP) greater than 140 mmHg and/or diastolic blood pressure (DBP) greater than 90 mmHg or known to be hypertensive were classified as having high blood pressure levels (1,19).
Anthropometric data
To evaluate height, a metal stadiometer (Welmy®, in-wall, Santa Bárbara D'Oeste, SP, Brazil), with an accuracy of 1 cm was used. Body mass was obtained using a TANITA digital scale (model Iron Man BC-554®) with a capacity of 200 kg and an accuracy of 100 g. Subjects were wearing as little clothing as possible, barefoot, and had no metal objects on, according to the procedures described by the manufacturer. WC was measured with an inelastic measuring tape (Sanny®, São Paulo, SP, Brazil) with an accuracy of 0.1 mm, at the midpoint between the last rib and the iliac crest. The cutoff points proposed by the World Health Organization (18) for WC were adopted. To perform these measurements the subject was asked to be barefoot, with arms along the body and head in the horizontal plane of Frankfurt.
NC was measured immediately below the laryngeal prominence, using cutoff points proposed for the Brazilian population (20). Hip circumference was measured at the level of the maximum posterior extension of the gluteus in a horizontal plane. Circumference measures were taken with subjects in orthostatic position using a Sanny® inelastic measuring tape (São Paulo, SP, Brazil) with 0.1-cm accuracy.
RFM was calculated based on height and waist circumference using the following equation (17):
RFM = 64 - (20 × [height in meters / waist in meters]) + (12 × sex)
Where: male sex = 0; female sex = 1.
After anthropometric measurements, BMI (body mass/height2) (18), BAI (hip circumference / height x √height - 18) (21,22), WHR (18) and WHtR (23) were calculated. BMI was classified according to the WHO scoring system (18). Percentage body fat values estimated by BAI and RFM above 25 % for men and 35 % for women were considered as excess body adiposity (24). For WHR, cutoff points of 0.85 for women and 0.90 for men (18) were adopted, while for WHtR a cutoff point of 0.50 was used for both sexes (23).
DATA COLLECTION AND ETHICAL PROCEDURES
Data collection took place in a private room and all evaluators were trained to perform measurements. Participants were informed about the data collection procedures and study objectives, and signed an informed consent form. The project was approved by the Ethics Committee for Research with Humans of the Federal University of Viçosa (58964616.4.0000.5153).
STATISTICAL ANALYSIS
Descriptive statistics were used to characterize data, and counts and proportions were used for categorical variables. Due to the differences between sexes described in the literature, analyses were performed with stratification by sex. Differences in proportions were identified using the Chi-square test. Pearson's correlation between anthropometric indexes and SBP and DBP were calculated to identify relationships between variables. A logistic regression model was used to verify the association between high blood pressure levels and anthropometric variables. Receiver-operating characteristic (ROC) curve analysis was adopted for each adiposity index to assess the ability to correctly discriminate high blood pressure levels. The significance level adopted was 5 % (p < 0.05). Data were entered twice and analyzed using the Stata 13.1 software.
RESULTS
This study involved 896 individuals, 421 men (46.99 %) and 475 women (53.01 %) with a mean age of 22.16 years (SD, 4.01). The proportion of high blood pressure levels was 21.32 %, this being significantly higher in men (34.68 %, p < 0.01). Table I describes the proportion of individuals with increased values. Compared to women, men had a higher proportion of increased BMI (p < 0.01), BAI (p < 0.01), WHtR (p = 0.03), SBP (p < 0.01) and DBP (p < 0.01), while women had a higher proportion of increased RFM (p < 0.01) and WC (p < 0.01).
Table I. Description of anthropometric indexes and systolic and diastolic blood pressure in university students, according to sex. Brazil, 2017/2018 (n = 896)

RFM: relative fat mass; BMI: body mass index; BAI: body adiposity index; WC: waist circumference; NC: neck circumference; WHR: waist-to-hip ratio; WHtR: waist-to-height ratio; SBP: systolic blood pressure; DBP: diastolic blood pressure. p-value obtained from the Chi-squared test.
Bivariate correlation coefficients between anthropometric variables and SBP and DBP were analyzed. Pearson's correlation coefficients revealed positive and significant associations (p < 0.01) between anthropometric measurements and SBP and DBP (Table II). Table II shows the correlation matrixes stratified by sex. In males and in females, correlations between RFM and SBP and RFM and DBP were higher only among those observed between BAI and SBP, BAI and DBP, WHR and SBP, and WHR and DBP (p < 0.01 for all).
Table II. Correlation matrix between the anthropometric indexes and systolic and diastolic blood pressure in university students, according to sex. Brazil, 2017/2018 (n = 896)

RFM: relative fat mass; BMI: body mass index; BAI: body adiposity index; WC: waist circumference; NC: neck circumference; WHR: waist-to-hip ratio; WHtR: waist-to-height ratio; SBP: systolic blood pressure; DBP: diastolic blood pressure. *p-value < 0.01, obtained from Pearson's correlation test.
In males, all anthropometric parameters were associated with high blood pressure levels, with WC showing a greater association in the unadjusted analysis (OR, 3.66; 95 % CI, 2.29 to 5.83). After controlling for age, it was observed that all parameters remained positively associated (Table III), with WC remaining as the indicator with the greatest strength (OR, 3.66; 95 % CI, 2.28 to 5.08). In females (Table III), BMI was the indicator that showed the greatest association with high blood pressure levels (OR, 5.08; 95 % CI, 2.69 to 9.61). Although it lost strength in the association after adjustment for age, BMI was still the marker with the highest association for high blood pressure levels (OR, 5.06; 95 % CI, 2.67 to 9.59).
Table III. Logistic regression, unadjusted and adjusted for high blood pressure levels with anthropometric indexes in university students, according to sex. Brazil, 2017/2018 (n = 896)
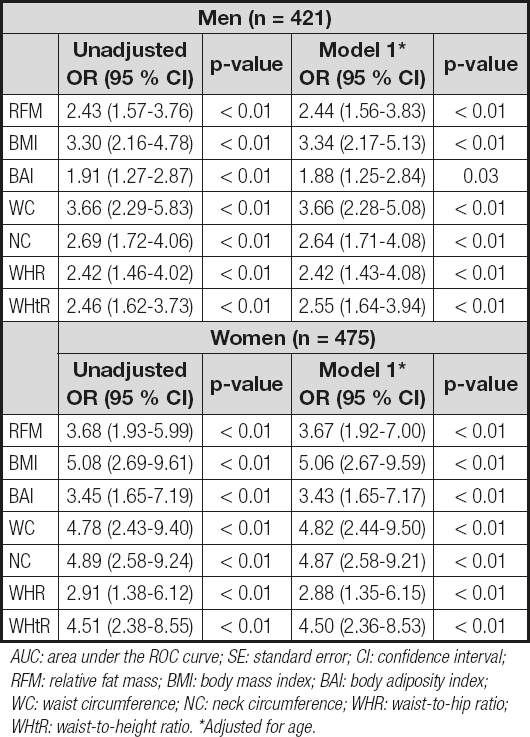
AUC: area under the ROC curve; SE: standard error; CI: confidence interval; RFM: relative fat mass; BMI: body mass index; BAI: body adiposity index; WC: waist circumference; NC: neck circumference; WHR: waist-to-hip ratio; WHtR: waist-to-height ratio. *Adjusted for age.
The use of the ROC curve to assess areas under the curve (AUC) and 95 % confidence intervals in the prediction of high blood pressure levels is shown in table IV. Although BMI showed an area under the upper curve in males (0.69; 95 % CI, 0.63 to 0.74), in females BMI (0.75; 95 % CI, 0.67 to 0.82) showed an area under the curve similar to NC (0.75; 95 % CI, 0.67 to 0.82); this was not statistically different from all other anthropometric indicators.
Table IV. Area-under-the-curve analysis of high blood pressure levels and anthropometric indexes in university students, Brazil, 2017-2018 (n = 896)

AUC: area under the ROC curve; SE: standard error; CI: confidence interval; RFM: relative fat mass; BMI: body mass index; BAI: body adiposity index; WC: waist circumference; NC: neck circumference; WHR: waist-to-hip ratio; WHtR: waist-to-height ratio.
DISCUSSION
Some studies with Brazilian adults aimed to verify the predictive capacity of anthropometric indicators for predicting SAH (4,11,13), but this study included in its analysis the recent RFM index and compared its predictive capacity with other indicators already used in clinical practice in young Brazilian adults. RFM is one of the most recently proposed indicators and has been compared to more than 250 anthropometric measurements (17) to verify its ability to estimate fat percentage. Recently, a study conducted in a Chinese population (25) verified the predictive capacity of RFM when compared to other indicators to predict incident SAH, and RFM proved to be an indicator capable of predicting incident SAH, although it did not replace indicators such as BMI, WC, and WHtR, results that are similar to those observed in our study. In general, in our study, all indicators were associated with high blood pressure levels in both sexes, with WC in males (OR, 3.66; 95 % CI, 2.28 to 5.08) and BMI in females (OR, 5.06; 4 95 % CI, 2.67 to 9.59) being those with the highest association strength.
In our study, using a sample of university students, RFM was not the best indicator of high blood pressure levels. Although RFM had a high and significant OR in men (OR, 2.44; p < 0.01) and in women (OR, 3.67; p < 0.01), it was only higher than the association found for BAI (OR, 1.88; p < 0.01 and OR, 3.43; p < 0.01, respectively) and WHR (OR, 2.42; p < 0.01 and 2.88; p < 0.01, respectively) with high blood pressure levels. Although RFM is easy to apply, it involves a greater number of mathematical calculations when compared to other indicators, which can be a limiting factor for its use. In addition, WC measurement, used in the calculation of RFM, involves professional training and is scarcely used in clinical practice (26), which, in addition to the low association with high blood pressure levels, limits the use of RFM in relation to other indicators.
As already mentioned, RFM was recently proposed, so its consistency as a body adiposity indicator and its possible association with cardiometabolic risks indicators need further investigations. Among the few studies found, RFM was not able to overcome WC and WHR in predicting the risk of general mortality in a population-based cohort, and the authors highlighted that RFM can be a good tool to estimate body adiposity percentage, not being better than methods already established in the literature (27). In another study conducted in a Korean population to validate the diagnostic capacity of RFM as an indicator of body adiposity percentage, it was observed that the accuracy of this index is comparable to BMI, but RFM presented an incorrect classification rate lower than BMI for women (26). These data, as well as the results of our study, indicate that RFM seems to be able to estimate body adiposity percentage and, consequently, its association with CVD, but it does not seem to be better than other already consolidated indicators.
Regarding the best indicator for estimating high blood pressure levels, divergences in results require further studies involving new indexes such as RFM. For example, in a follow-up study (2.8 years) with the Korean population, it was observed that the increase in the baseline WHtR value was positively associated with the development of SAH (28). In a study with primary data from a cohort of adults from South Asia, it was found that WC and WHtR were the best indicators to identify adults with prevalent SAH (29). In male employees of a hospital in Argentina, BMI showed a greater predictive capacity for SAH when compared to WC and WHtR (30). In a large sample of Peruvian adults, WC was the best indicator of body adiposity to estimate high blood pressure in males (31). These variations in anthropometric indicators capable of predicting SAH can be attributed to the distinct characteristics of each population regarding sample selection and size, cutoff points, and body adiposity assessment (32). In our study, WC and BMI were, as the indicators with the highest association with high blood pressure levels, consistent with other studies. However, it is important to highlight that, in females, the strength of the association and the area under the NC curve was superior to those of the other indicators.
Some studies with Brazilian adults have been conducted to analyze the capacity of anthropometric indicators to predict blood pressure. In adults in the city of Vitória, state of Espírito Santo, Brazil, it was found that WHtR was the best applicable obesity index to identify hypertension (33). In another study with Brazilians residing in the Federal District, the conicity index, WHR and WHtR had a greater relationship with hypertension when compared to BMI in men, while in the female gender WHR and WHtR showed better results, although, after adjustment, no measure remained associated with high blood pressure values in women (11). In our analyses, all anthropometric indicators were associated with high blood pressure levels; however, WC in men and BMI in women showed better associations. Taking into account the simplicity of application and their low cost, these indicators seem to be a good alternative to identify high blood pressure levels.
In another study conducted with Brazilian adults to verify which indicator was more strongly associated with SAH, WC and BMI were also the primary associated indicators in men and women, respectively (34). Unlike our analysis, this study used only 4 anthropometric indicators, among them the visceral adiposity index (VAI), which estimates visceral fat dysfunctions with cardiometabolic risks (35). Although this index assesses visceral fat, which is more strongly associated with cardiometabolic diseases than other adipose tissue compartments (36), it was not superior to the other parameters evaluated (34). In addition, the measurement to be used in a screening should be the simplest and least expensive possible, and allow a reliable risk estimate, which is not the case with VAI, which requires the use of biochemical markers for its calculation, not always being accessible in clinical practice. In this sense, the findings of our study are relevant because they show the relationship of indicators that are easy to use and that do not require equipment and/or refined techniques for their application, allowing the use of these indicators in studies with large samples, in places where assessment resources are limited, and as screening tools.
Unlike the analyses carried out in Brazilian populations (11,34) and other studies (5,6,28), in addition to including the recent RFM index in our analysis, NC was included, which is a parameter that is easy to measure and requires only a measuring tape. Studies have shown correlation of NC with weight, BMI, and WC (37), and with visceral adipose tissue as assessed by means of computed tomography (38). Data from 2,732 individuals in the Framingham cohort also indicated that NC was associated with SAH (39). In our study, NC was one of the indicators with the highest association with high blood pressure levels, the third with the greatest association strength in males (OR, 2.64; 95 % CI, 1.71 to 4.08) and the second in females (OR, 4.87; 95 % CI, 2.58 to 9.21), surpassing RFM and other indicators already consolidated. NC can be a good alternative for use as a screening instrument since it only requires a measuring tape and the anatomical reference point is easy to locate.
When analyzing the predictive capacity of anthropometric indicators for high blood pressure levels, it was observed that BMI and NC were those that presented the largest area under the ROC curve in both sexes, but they were not significantly different from the other indicators. In addition, all indicators in males and BAI and WHR in females showed areas under the curve below 0.7, which is indicative of a low predictive capacity (40). The search for a measure that can adequately estimate body fat percentage and, especially, its association with cardiometabolic parameters requires further investigation.
Some strengths and limitations should be highlighted in order to interpret the results of this study. Methodological rigor was maintained, guaranteeing the internal validity of the study; in relation to SAH, this is the first known study that included RFM and compared its predictive capacity for high blood pressure levels with other anthropometric indicators already consolidated in the literature. In addition, the use of several low-cost and easy-to-use body fat indicators in large samples at the detriment of expensive and difficult-to-access equipment should be highlighted, as it allows a greater external validity. Despite these strengths, some limitations should be highlighted. As the population of this study was restricted to university students, the extrapolation of data to other groups should be performed with caution; however, it is important to highlight that the early identification of changes in blood pressure values can contribute to its control and prevention. The cross-sectional design requires care in inferring results, limiting the capacity to establish causal relationship between variables. Although the analyses have been adjusted by age, it is still possible that unmeasured variables may influence associations.
In conclusion, the findings of our study suggest that RFM is not the best indicator for predicting high blood pressure levels in university students, although it has shown positive associations. WC in men and BMI in women showed the best associations. This reinforces the idea of maintaining and using simple methods, applicable in daily practice, such as circumference measures, to the detriment of more complex approaches.














