INTRODUCTION
Hypertension and diabetes, as common chronic diseases worldwide, are considered to be the main risk factors for cardiovascular and cerebrovascular diseases (1). According to the Report on Cardiovascular Health and Diseases in China 2019, the number of hypertensive patients in China has reached 245 million, and continues to increase rapidly (2). In recent 30 years, the prevalence of diabetes in China has soared from 0.67 % in 1980 to 11.2 % in 2017 (3). Due to the same risk factors, hypertension and diabetes often occur together. Both diabetes and hypertension are considered as major health problems that negatively impact the cerebral function (4-6). Currently, transcranial Doppler sonography (TCD) becomes a common method to evaluate the risk of cerebral arteriosclerosis and cerebrovascular diseases, and plays a key role in the effectiveness evaluation of atherosclerosis prevention and treatment trials.
Effective prevention and control of hypertension and diabetes is the focus of current research, among which diet plays an important role in the control of hypertension and diabetes. As early as 1997, a large hypertension prevention program in the United States (Dietary Approaches to Stop Hypertension [DASH]) made DASH diets specially designed for hypertension patients (7). Then numerous subsequent studies have found the DASH diet has a good control effect on blood pressure (8,9) and blood glucose (10). Besides, low-sodium salt was used to improve high blood pressure and reduce cardiovascular risk. Wu Yangfeng provided low-sodium salt containing 75 % sodium chloride free of charge to more than 20,000 hypertensive patients for five years, and the results showed that stroke, major adverse cardiovascular events and all-cause mortality were significantly reduced, suggesting low sodium salt has long-term safety and efficacy (11). Based on the DASH dietary principles, we formulated the Chinese Modified Dietary Approaches to Stop Hypertension (CM-DASH) diet according to the dietary habits of Chinese residents, and combined CM-DASH and low-sodium salt to explore the short-term effects of this dietary pattern on cerebrovascular function in patients with hypertension complicated with type 2 diabetes and the short-term control effect on blood pressure and blood glucose.
METHODS
PARTICIPANTS
Participants were recruited by using the following eligibility criteria: a) age ≥ 50 and ≤ 75 years old; b) residence near the hospital, no withdrawal or plan to go out during October to December 2021, possibility of regular follow-up; c) hypertensive patients with type 2 diabetes (the diagnostic criteria for hypertension are based on the Chinese Guidelines for the Prevention and Treatment of Hypertension, 2018 revised edition [1212] and the diagnostic criteria for diabetes are based on the Chinese Guidelines for the Prevention and Treatment of Type 2 Diabetes, 2017 edition [1313]) who currently regularly take antihypertensive drugs/hypoglycemia drugs; d) to strictly abide by the recipes and salt provided during the trial; and e) all the subjects and their family members living together signed the informed consent. The exclusion criteria were: a) patients with malignant tumor, acute myocardial infarction, stroke within three months or other serious diseases, and expected survival time less than one year; b) increased cortisol disorder or aldosteronism; c) acute diseases such as upper respiratory tract infection, fever, severe diarrhea; d) deaf-mute, dementia, and serious depression or other mental disorders which prevent from communicating normally; e) inconvenient movement and inability to be followed up on time; f) renal dysfunction or chronic kidney disease at stage 4 or above; g) abnormal liver function, with alanine aminotransferase (ALT) or aspartate aminotransferase (AST) levels greater than two times the upper limit of normal, or total bilirubin level greater than the upper limit of normal; h) abnormal blood potassium < 3.5 mmol/l or > 5.5 mmol/l, or current use of potassium-preserving diuretics; i) women who are pregnant or may become pregnant or other contraindications for the use of the trial meals; j) attending to participate in other clinical studies or current consumption of low-sodium diet; and k) other ineligible conditions as adjudicated by investigators. Early withdrawal criteria were: a) the subjects themselves or their family members request to withdraw from the study; and b) adverse reactions occurred in the subjects themselves, which may be related to the test as judged by the researcher.
STUDY DESIGN
This eight-week single-arm trial was undertaken at the Health Management Center of the Second People's Hospital affiliated to Chongqing Medical University. The study protocol was approved by the Ethics Committee of Chongqing Medical University (2021080). Trial registration: Chinese clinical trial registry (ChiCTR2000029017), http://www.chictr.org.cn/.
From June to September 2021, 66 patients with hypertension complicated with type 2 diabetes were selected from the Health Management Center of the Second People's Hospital affiliated to Chongqing Medical University. Patients and their families signed informed consent forms. In the coming eight-week period, patients were asked to eat 5 g/day low-sodium salt (developed by Chongqing Shanshun Biological Technology Co., Ltd.; name: sodium limit standard salty flavin; executive standard: Q/SWS0025S; food production license number: SC10650012000709; main ingredients: potassium chloride [56 %] and sodium chloride [23 %]) plus CM-DASH diet. The CM-DASH diet is based on the dietary energy estimation table of DASH, combined with the Chinese Residents' Balanced Diet Pagoda (2019), dietary habits and food availability of Chinese residents, including 4-5 servings of fruits and vegetables a day, 2-3 servings of low-fat dairy products, 6-8 servings of whole grains, fewer than six servings of meat, poultry and fish a day, eating nuts 4-5 times a week, and choosing foods that are low in saturated fat, potassium, fiber and sodium. The subjects were asked not to change their lifestyle or medication habits.
STUDY PROCEDURES AND OUTCOME MEASURES
Volunteers were invited to the Health Management Center for a baseline survey to determine eligibility. If eligible and willing to participate, height, weight, waist circumference and hip circumference were measured and used to calculate body mass index (BMI) and waist-to-hip ratio.
CEREBROVASCULAR FUNCTION
Cerebrovascular function was measured with transcranial Doppler sonography (TCD) with Lipon TDD-IIX2P TCD detector (frequency of 2-8 mhz) before and after the intervention. TCD examination method referred to the Standard Guidelines for Operation and Diagnosis of Transcranial Doppler Ultrasound (2008) (14):
Comparing the blood flow rates of each artery of the subjects before and after the intervention, including anterior cerebral artery (ACA), middle cerebral artery (MCA), internal cerebral artery (ICA), vertebral artery (VA) and basilar artery (BA). Peak systolic velocity (VP), mean flow velocity (VM) and end-diastolic velocity (VD).
The above arterial pulsatility index (PI) and vascular resistance index (RI) were compared before and after intervention.
CLINIC INDICATORS OF CHRONIC DISEASES
Blood pressure, blood glucose and blood lipids were measured before and after the intervention:
Before blood pressure measurement, subjects were required to sit still for 30 minutes. Systolic blood pressure (SBP) and diastolic blood pressure (DBP) were measured for three times using the medical upper arm electronic blood pressure instrument (Omron HEM-7130) at an interval of three minutes. The average value of the last two times was taken as the measurement value. Blood pressure control target refers to the National Primary Hypertension Prevention and Treatment Management Guidelines (2020 edition) (15) (SBP < 130 mmHg and DBP < 80 mmHg).
Fasting blood glucose (FBG) and postprandial blood glucose (PBG) were measured using a medical blood glucose monitor (Dale C, GM505RAB). Blood glucose control target refer to the Guidelines for the Prevention and Treatment of Type 2 Diabetes Mellitus in China (2020 edition) (3) (FBG < 7.0 mmol/l and PBG < 10.0 mmol/l).
Fasting venous blood samples were collected before and after the intervention from all enrolled participates to assess lipid profile including triglycerides (TG), total cholesterol (TC), high-density lipoprotein (HDL-C) and low-density lipoprotein (LDL-C). Blood lipids control target refers to the Guidelines for Primary Care of Dyslipidemias (2019) (16) (TC < 5.2 mmol/l; LDL-C < 3.4 mmol/l; HDL-C > 1 mmol/l and TG < 1.7 mmol/l).
URINARY EXCRETION
Twenty-four-hour urinary excretion was measured before and after the intervention. The subjects were asked to maintain their current diet and collect urine for 24 hours under the direction of the researchers. After the collection was completed, the researchers recorded urine volume and took samples for sodium and potassium urine tests and calculated the ratio of sodium to potassium.
STATISTICAL ANALYSIS
SPSS24.0 statistical software was used for statistical analysis. The count data were expressed by N (percentage %) and tested with Wilcoxon signed-rank test. The measurement data of normal distribution were expressed by mean ± standard deviation (X ± SD) and tested with paired t-test. Non-normal data were expressed by median (first quartile, third quartile) and tested with Wilcoxon signed-rank test. α = 0.05.
RESULTS
PARTICIPANTS
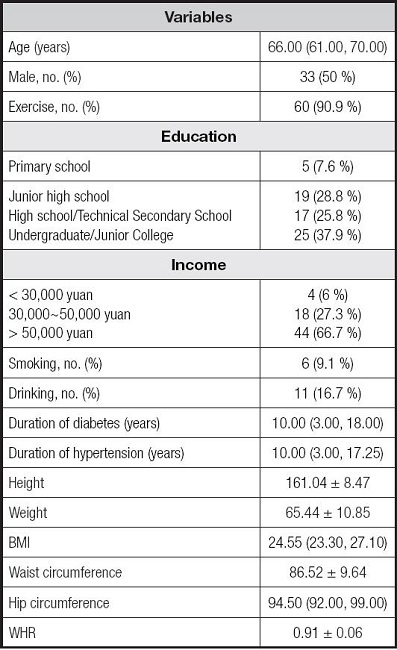
Participants' baseline characteristics are shown in table I. They were all patients with hypertension and type 2 diabetes, with a mean age of 66 years, a mean course of hypertension of ten years and a mean duration of diabetes of ten years. Fifty-nine subjects (29 males and 30 females) completed the eight-week dietary intervention. Seven participants withdrew prior to the last measurement. There were no serious adverse events to report.
CEREBROVASCULAR FUNCTION
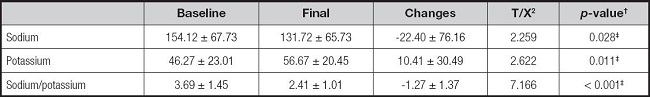
Compared with baseline, PI and RI of ACA decreased significantly (-0.08 ± 0.22, p = 0.005; -0.04 ± 0.09, p = 0.004); PI and RI of MCA decreased significantly (-0.10 ± 0.27, p = 0.006; -0.04 ± 0.11, p = 0.004); VP, VM, VD of ICA increased significantly (4.00 ± 8.98, p = 0.001; 4.64 ± 7.04, p < 0.001; 4.94 ± 7.6, p < 0.001), PI and RI of ICA decreased significantly (-0.11 ± 0.25, p = 0.001; -0.04 ± 0.10, p = 0.001); VP, VM and VD of VA increased significantly (3.83 ± 12.07, p = 0.019; 4.68 ± 8.46, p < 0.001; 4.96 ± 8.00, p < 0.001), PI and RI of VA decreased significantly (-0.17 ± 0.30, p < 0.001; -0.06 ± 0.11, p < 0.001); VD of BA increased significantly (2.52 ± 7.32, p = 0.011) and PI of BA decreased significantly (-0.08 ± 0.27, p = 0.029) (Table II).
Table II. Effect in transcranial Doppler sonography tests*.
ACA: anterior cerebral artery; MCA: middle cerebral artery; ICA: internal cerebral artery; VA: vertebral artery; BA: basilar artery; VP: peak systolic velocity; VM: mean flow velocity; VD: end-diastolic velocity; PI: pulsatility index; RI: resistance index.
*Values are expressed as mean ± SD.
†Paired t test.
‡p < 0.05.
CLINIC BLOOD PRESSURE, GLUCOSE AND LIPIDS
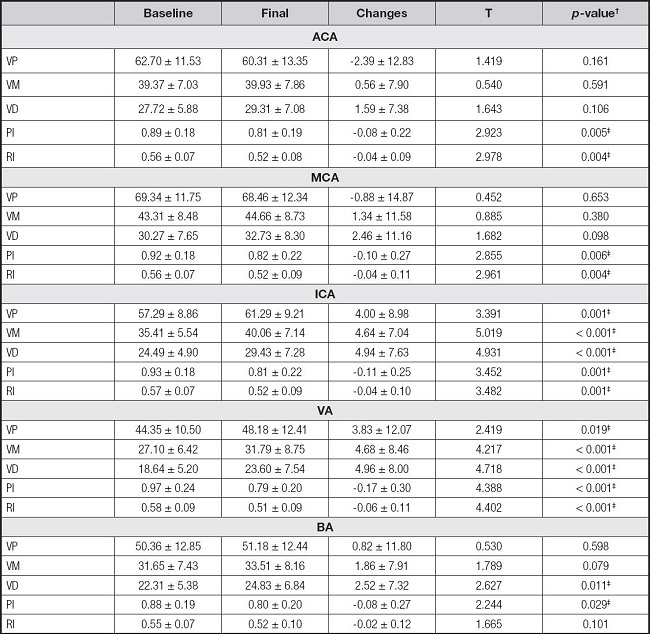
Compared with baseline, SBP, DBP, FBG and PBG decreased respectively (-16.36 ± 16.44, p < 0.001; -7.19 ± 8.32, p < 0.001; -1.60 [-2.80, -0.50], p < 0.001; -2.90 [-5.30, -1.00], p < 0.001), while HDL-C increased significantly (0.03 ± 0.11, p = 0.032). Blood pressure and blood glucose control increased significantly after intervention (p < 0.001) (Table III).
Table III. Effect in blood pressure and blood glucose control rate*.
SBP: systolic blood pressure; DBP: diastolic blood pressure; FBG: fasting blood glucose; PBG: postprandial blood glucose; TG: triglyceride; TC: total cholesterol; HDL-C: high density lipoprotein cholesterol; LDL-C: low density lipoprotein cholesterol.
*Values are expressed as mean ± SD or number, frequency (%).
†Paired t test or Wilcoxon signed-rank test.
‡p < 0.05.
24H-URINARY EXCRETION
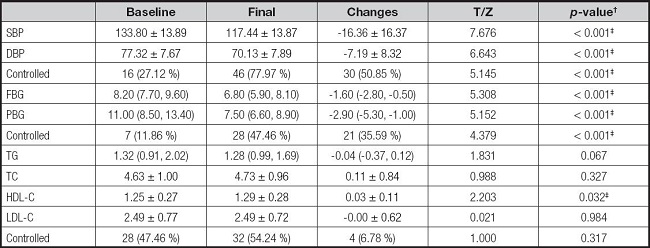
Compared with baseline, urinary sodium and sodium/potassium ratio decreased significantly (-22.40 ± 76.16, p = 0.028; -1.27 ± 1.37, p < 0.001) while urinary potassium increased significantly (10.41 ± 30.49, p = 0.011) (Table IV).
DISCUSSION
At present, the control strategy for chronic diseases such as hypertension and diabetes has changed from drug treatment to comprehensive intervention, including lifestyle management, blood pressure and blood glucose monitoring and health education. Nutritional therapy, as the core of lifestyle management, plays an indispensable role in the prevention and control of hypertension and diabetes, and should be throughout the management of hypertension and diabetes (15). The CM-DASH diet contains less total energy, fat, and cholesterol while it contains more protein and dietary fiber than the DASH diet. In addition, in order to meet the daily sodium requirements (< 2,300 mg) and potassium requirements (> 4,000 mg) of the DASH diet without changing salt habits, low sodium salt (23 % NaCl and 56 % KCl) was used in combination with CM-DASH diet to observe the intervention effect.
Xianbin D conducted an investigation on hypertension and diabetes among residents aged 35-75 in Chongqing, China, and found that the blood pressure and blood glucose control rates of patients with hypertension and diabetes were 15.54 % (17) and 16.17 % (18), respectively, which were similar to the baseline conditions of subjects in our study. Similar to the results of Appel LJ et al. (19-22), systolic blood pressure, diastolic blood pressure, fasting blood glucose and postprandial blood glucose were significantly reduced after eight weeks of intervention. Besides, the control rates of blood pressure and blood glucose were 77.97 % and 47.46 %, higher than baseline (p < 0.001). Blood pressure control rate increased by 50.85 % and blood glucose control rate increased by 35.59 %, indicating that 23 % low sodium formula combined with CM-DASH diet pattern can effectively and scientifically control blood pressure and blood glucose, and has good short-term efficacy.
Hypertension and diabetes are risk factors of cerebrovascular arteriosclerosis. In long-term hypertension, the impact of blood flow on the vascular wall will damage the intima of blood vessels, and after the endothelial function is damaged, the lipid in blood is more likely to deposit on the vascular wall, promoting the occurrence and development of atherosclerosis (23). Patients with diabetes mellitus are usually accompanied by endogenous hyperinsulinemia. Abnormally elevated endogenous insulin stimulates vascular smooth muscle cells, resulting in the increase of the micro RNA208 gene, which then inhibits cycle-dependent protein kinase P21 and stimulates abnormal proliferation of vascular smooth muscle cells, leading to atherosclerosis (24). When diabetes is combined with hypertension, the degree of damage to target organs will be multiplied; for example, the degree of damage to cerebrovascular will be increased by two times. TCD detection in patients with hyperglycemia complicated with diabetes can detect cerebrovascular diseases, especially early ischemic cerebrovascular diseases, so as to get timely treatment, prevent the occurrence of stroke and other diseases, and improve the quality of life. Yuhan K performed TCD detection on 892 patients with essential hypertension and found that, compared with non-hypertensive people, cerebral vascular blood flow rate was decreased while RI and PI were increased in hypertensive patients, and most obviously in hypertensive patients with glucose metabolism disorder (25). The conclusion of Yuhan K's study was consistent with the baseline situation of patients observed in this study. But after eight weeks of dietary intervention, subjects had significant improvement in hemodynamic indexes of ICA, MCA, ACA, VA and BA, indicating that 23 % low-sodium formula combined with CM-DASH diet can effectively improve cerebral vascular function.
Urine test results showed a significant decrease in urinary sodium and a significant increase in urinary potassium, suggesting that the participants' sodium intake was reduced and potassium intake increased through the eight-week dietary intervention. Potassium ion can promote sodium ion excretion, improve endothelial function and reduce plasma angiotensin by affecting the activity of sodium-chloride cotransporter and sensitivity of catecholamines (26). In addition, the DASH diet, which is rich in unsaturated fatty acids, protein and dietary fiber and low in saturated fatty acids, can improve lipid metabolism disorders and reduce lipid deposition on blood vessel walls, thereby delaying or improving atherosclerosis (27). In this study, eight weeks of dietary intervention increased HDL-C. The DASH diet, which includes plant-based, fiber-rich foods and natural antioxidants, reduces plasma concentrations of monocyte chemotaxis protein-1 (McP-1), thereby improving atherosclerosis to some extent (28).
CONCLUSION
Twenty-three per cent low-sodium formula combined with CM-DASH diet pattern can improve cerebrovascular function in community patients with hypertension complicated with diabetes, and has a good short-term benefit of blood pressure and glucose control.
Disclosure:
The Ethics Committee of Chongqing Medical University approved the research protocol (2021080). All subjects and their families signed an informed consent form. Approval date of registry and registration no. of the study/trial: 2020.1.11, Chinese clinical trial registry (ChiCTR2000029017) (http://www.chictr.org.cn/).