INTRODUCTION
Projections indicate that acquired immunodeficiency syndrome (AIDS) is in the world ranking of health problems. However, human immunodeficiency virus (HIV) infection rates continue to rise, with an estimate of 37.7 million people living with HIV worldwide and 1.5 million new cases recorded in 2020 (1). In Brazil, from 1980 to June 2021, 1,045,355 cases were detected, with a decrease in the detection rate in Brazil since 2012 (2).
Invariably, antiretroviral therapy (ART) has profoundly changed the natural history of HIV infection, dramatically reducing AIDS-related morbidity and mortality (2-4). However, there is evidence of important adverse effects of ART such as dyslipidemia, glucose intolerance and hypertension, all recognized as risk factors for cardiovascular disease (CVD). The combination of these effects with chronic inflammation, immune activation and changes in coagulation factors present in the syndrome potentiates the development of CVD and metabolic syndrome (MS) in people living with HIV (5,6).
Recent studies have suggested the use of neck circumference (NC) as an indicator of cardiometabolic risk and truncal obesity, as well as body mass index (BMI) and waist circumference (WC) and hip circumference. Both have a positive relationship with the components of MS, overweight and obesity (7-9).
Several authors refer to NC as an effective, inexpensive and easily applied measure to assess CVD risk and upper body fat accumulation, suggesting that it can be used as a screening tool. However, its use in clinical practice is precluded because there is no international consensus regarding ideal cut-offs (10-13).
The identification of cardiometabolic risk and early morphological changes in people living with HIV, through the assessment and diagnosis of nutritional status, helps to establish effective interventions to treat these complications (14) with appropriate actions that can improve long-term care and provide better prospects for their quality of life (15).
Given the scenario that maintains HIV infection as a serious public health problem worldwide, and considering the potential role of nutrition in the health status of people living with HIV, the knowledge of the nutritional aspects involved in this pathology has a great importance, as well as the establishment of effective nutritional indicators with high predictive value of related comorbidities. In this context, the objective of the present study was to investigate the relationship of NC with other anthropometric indicators and to assess cardiometabolic risk and truncal obesity by proposing cut-off points for people living with HIV.
MATERIAL AND METHODS
DATA SOURCES AND STUDY POPULATION
The data presented come from a study with 233 individuals of both sexes living with HIV who were assisted at a reference center for infectious and contagious diseases between September 2017 and July 2019.
The eligibility criteria for participating were being in use of ART, age between 20 and 59 years old, not in use of vitamin or mineral supplementation, and no diagnosis of metabolic diseases, bone diseases, chronic renal failure, liver diseases, gastric diseases or disabsorptive syndromes and neoplasy. Pregnant and lactating women were not included.
The study was approved by the Ethics Committee of the Federal University of Piaui (review no. 2,100,110), and followed the recommendations defined in the Resolution of the National Health Council of Brazil no. 466 of 2012 and in the Operational Norm no. 001 of 2013. All the participants signed the informed consent form.
ANTHROPOMETRIC MEASUREMENTS
Participants were evaluated by trained researchers who applied the interview (socioeconomic, clinical information) and collected anthropometric data. All measurements were performed in triplicate and followed the recommendations of the Food and Dietary Surveillance System of the Brazil Ministry of Health (16).
Body weight (kg) was measured on a digital scale (Seca®, Brazil), with the patient barefoot and wearing light clothing. Height (m) was measured with a portable vertical stadiometer (Seca®, Brazil) with the participant standing upright and the head aligned in the Frankfurt plane.
BMI (kg/m2) was calculated by dividing weight (kg) by height (m) squared. Nutritional status was classified by BMI according to the World Health Organization (WHO) criteria: thinness ≤ 18.5 kg/m2; eutrophic > 18.5 and ≤ 24.9 kg/m2; overweight ≥ 25 and ≤ 29.9 kg/m2; and obesity ≥ 30 kg/m2.
All circumferences were measured with inelastic tape measures (Seca®, Brazil). WC was measured at the midpoint between the lower edge of the costal arch and the iliac crest at the middle axillary line (17). The cut-off point for cardiometabolic risk used was ≥ 94 cm for men and ≥ 80 cm for women, according to the WHO (18).
NC was measured above the cricothyroid cartilage and just below the laryngeal prominence with the individual sitting and with the head positioned in the Frankfurt horizontal plane. The cut-off points to indicate abnormality in the adult population adopted in the study were ≥ 39 cm for men and ≥ 35 cm for women because they are considered as the most ideal in studies to determine individuals with central obesity and metabolic syndrome (11,19,20).
The arm circumference (AC) was obtained at the midpoint between the acromion and the olecranon. The anatomical point was also used to measure the triceps skinfold (TSF) on the back of the arm, while the subscapular skinfold (SSF) was measured obliquely in relation to the longitudinal axis, following the orientation of the costal arches, being located two cm below the inferior angle of the scapula. A calibrated adipometer (LANGE®) was used to collect skinfolds (accuracy of 1 mm). The sum of the folds (Σfolds) was defined by the sum of TSF and SSF, while the arm muscle circumference (AMC) was obtained as suggested by Frisancho (42): AMC = [AC - (TSF x π)]² / (4 x π).
LABORATORY ANALYSIS
The determination of viral load and TCD4+ concentrations was performed at the Central Public Health Laboratory of the State of Piaui (LACEN – PI). The material used for the viral load tests was plasma, and the quantification was carried out through polymerase chain reaction (PCR) in real time. The TCD4+ lymphocyte count was performed using flow cytometry.
STATISTICAL ANALYSIS
Data were tabulated in the Microsoft Office Excel software spreadsheet and analyzed using the statistical package Stata® version 12. Results were presented in means and 95 % confidence intervals (95 % CI) for continuous variables and frequency and percentage for categorical variables. The normality of continuous variables was tested using the Shapiro-Wilk test. The difference in age, anthropometric measurements, TCD4+, ART time and disease time means between males and females was verified using the Mann-Whitney test. The Spearman's correlation coefficient between NC and anthropometric and clinical indicators was evaluated.
In order to assess NC performance in determining cardiometabolic risk in patients with HIV from WC and BMI (default), ROC curve analysis was applied by evaluating the area under the ROC curve (AUC) and 95 % CI. Sensitivity and specificity of NC in relation to WC and BMI were calculated.
Positive and negative predictive values (PPV and NPV, respectively) were also considered in the selection of cut-off points, as both estimate the probability of disease based on the gold standard (WC and BMI) (21). PPV indicates the probability of a person with a positive test actually having the condition while NPV is the opposite (22). The cut-off points presented were those that had the most appropriate balance between sensitivity and specificity taking into consideration the likelihood ratio and the positive and negative predictive values of the tests. Tests with p value < 0.05 were accepted as statistically significant.
RESULTS
In the present study (n = 233), 134 participants (57.5 %) were men and 99 (42.5 %) were women, with a mean age, respectively, of 37.3 years (95 % CI: 35.6-39.0 years) and 39.9 years (95 % CI: 38.2-41.7 years), with a statistically significant difference between sexes (p = 0.038). Regarding the clinical aspects, it was observed that the individuals presented immune activity (TCD4+) and viral load without significant difference between sexes (p = 0.893 and p = 0.456, respectively).
The mean time since diagnosis was 76.4 months (95 % CI: 67.5-85.3 months), and the average antiretroviral therapy (ART) use duration was 68.4 months (95 % CI: 60.3-76.6 months), with no statistically significant difference between sexes (p > 0.05). Clinical data categorized by sex are presented in table I. Regarding therapeutic regimens, there was a predominance in the use of nucleoside reverse transcriptase inhibitors (48.5 %) with lamivudine and tenofovir being the most used. In second place of predominance was the class of integrase inhibitors (29.61 %) with a higher prevalence of dolutegravir. The class of protease inhibitors (21.89 %) had a lower predominance of use, with atazanavir and ritonavir being the most cited. No significant association was observed between NC and antiretroviral treatment (p = 0.901), as well as with abdominal WC (p = 0.153) (not shown in the table).
Table I. Mean (95 % CI) and proportions of clinical and anthropometric variables of people living with HIV, according to sex.

ART: antiretroviral therapy; TA: duration of ART; TD: time of disease; ND: non-detectable; BM: below minimum limit; NRTI: nucleoside reverse transcriptase inhibitors; PI: protease inhibitor; INI: integrase inhibitor; WC: waist circumference; NC: neck circumference; BMI: body mass index.
As for the anthropometric variables, according to table I, higher means in men for weight (p < 0.001), height (p < 0.001), WC (p = 0.01) and NC (p < 0.001) were observed. It is noteworthy that there was a higher percentage of cardiometabolic risk (according to WC) in men (75.4 %) than in women (56.6 %, p = 0.002), being observed the significant difference in the proportions of presence and absence of risk between the sexes.
In addition, there was no significant difference in the proportions of thinness, eutrophic, overweight or obesity between males and females (p > 0.05) (Table I). There was a high prevalence of excess weight in the individuals, with 30.9 % overweight and 9.9 % obese (data not shown in the table).
Table II shows that the NC had a statistically significant positive correlation with all anthropometric measurements of the study (WC, BMI, AC, AMC, TSF, SSF, sum of skin folds, p < 0.001) in both sexes, being stronger in men than in women, and showing higher correlation strength with WC and BMI, especially in males.
Table II. Correlation coefficients between neck circumference and anthropometric and clinical indicators of people living with HIV, according to sex.

WC: waist circumference; BMI: body mass index; AC: arm circumference; AMC: arm muscle circumference; TSF: triceps skinfold; SSF: subscapular skinfold; Σfolds: sum of TSF and SSF; TD: time of disease; TA: time of ART; ART: antiretroviral therapy;
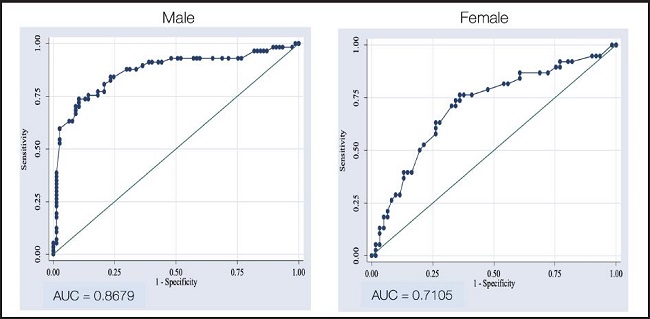
Table III presents the results of the performance analysis, and the NC cut-off points to assess cardiometabolic risk according to WC and BMI. It was noticed that the values selected as predictors of risk of cardiometabolic complications and truncal obesity considering WC and BMI among women were both ≥ 32.4 cm, while in men it was ≥ 39.6 cm and ≥ 38.1 cm, respectively. One can also observe according to the likelihood ratio (LR) that men with NC ≥ 39.6 cm are 6.37 times more likely to have cardiovascular and metabolic complications, while women with NC ≥ 32.4 cm are 2.2 times more likely.
Table III. Cut-off point values of NC to identify cardiometabolic risk and truncal obesity according to WC and BMI of people living with HIV, by sex.
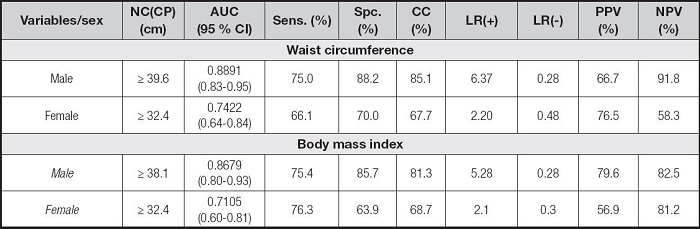
NC(CP): neck circumference cut-off point; AUC: area under the curve; Sens.: sensitivity; Spec.: specificity; CC: correctly classified; LR(+): positive likelihood ratio; LR(-): negative likelihood ratio; PPV: positive predictive value; NPV: negative predictive value.
The NPV was high in most analyses, being useful to rule out the presence of NC-associated risk in the sample of this study.
Based on the ROC curve analysis (Figs. 1 and 2), the cut-off points for detecting the risk of cardiovascular metabolic complications were expressively more sensitive and specific for males. The AUC (95 % CI) for NC in the assessment of WC and BMI in men was 0.8891 (0.83-0.95) and 0.8679 (0.80-0.93), showing a good performance, while in women it was a poor performance, being 0.7422 (0.64-0.84) and 0.7105 (0.60-0.81), respectively.

Figure 1. Results of ROC curves of neck circumference in the evaluation of waist circumference as risk measures for cardiac metabolic complications in men and women with HIV, according to their sensitivities and specificities.
DISCUSSION
Some issues related to ART are still challenging as a result of numerous adverse effects such as increased weight and triglyceride, total cholesterol and LDL-c levels, as well as decreased HDL-c and changes in body fat deposition in individuals with HIV (6).
Regarding the general characteristics of the participants presented in table I, they are similar to those of other studies, with a higher prevalence of men, with a mean age greater than 35 years old, using ART (27,28,38).
Literature states that high NC values are predictors of upper body subcutaneous fat accumulation (23,24) as well as significantly associated with metabolic syndrome components (25) and with prognostic variables such as waist circumference and body mass index (11,26).
The role of body fat redistribution in HIV infection is most commonly related to therapy medications, risk factors for CVD, and inadequate lifestyle habits (27). Jantarapakde et al. (28) demonstrated in their study that the metabolic syndrome was significantly higher (p = 0.018) in the group that experienced ART (24.9 %) compared to the group that did not (15.9 %), highlighting the contribution of ART use on clinical outcome. Conditions such as insulin resistance, dyslipidemia and increased inflammatory markers are reported in patients with ART-induced lipodystrophy, although its role in the development of metabolic syndromes has not been elucidated. Studies indicate that these drugs repress the differentiation of adipocytes, as well as in the expression, secretion and release of adiponectin in adipose tissue, in which it plays a crucial role in glucose regulation and fatty acid oxidation (29-31). Evidently, the accumulation of upper trunk fat has also been identified as a strong determinant of insulin resistance and altered lipid profile in people living with HIV (5,7).
There is considerable concern in the literature regarding the “optimal” cut-off points of anthropometric indices in predicting cardiovascular risk factors, whether due to the different clinical conditions of individuals, ethnicity, body composition or other environmental and individual factors that make the use of NC difficult in the clinical practice due to the complexity of establishing a reference value that can truly conjecture and diagnose those risks (28,29).
NC is a screening tool suggested to identify overweight, accumulation of subcutaneous adiposity in the upper body, and risk of cardiometabolic complications. Because it is a simple, low cost and non-invasive prognostic variable, which is not influenced by respiratory movements and pre or postprandial period, it is more socially acceptable, especially by overweight and obese people (30,31).
However, it is important to point out that there is no national and international consensus so far for NC measures cut-off points, therefore studies establish values from the evaluated population and from results of other studies (32).
Ben-Noun et al. (31) proposed optimal cut-off points to identify adult subjects with BMI of overweight and obesity using the NC. Subsequently Onat et al. (20) also proposed cut-off points of ≥ 39 cm and ≥ 35 cm for NC in adult men and women, respectively. These reference values are probably the best to identify upper-body obesity and cardiometabolic complications, which justifies the choice to be used in the present study (11,19,20).
In the present cross-sectional analysis of population data of people living with HIV, the AUC between NC and WC and NC and BMI were high in man, but AUCs were poor for women. This also reflected in NC being significantly correlated with a variety of indicators that proved to be a satisfactory indicator for assessing risk of metabolic complications and upper-body subcutaneous fat accumulation with measurements adjusted by sex which were significantly associated and stronger in men than in women.
Fitch et al. (27) conducted a study to verify the relationship between NC and cardiometabolic parameters in HIV-infected and non-infected adults and found that increased NC is strongly associated with HIV, BMI and visceral and subcutaneous abdominal adipose tissue areas in the whole cohort. Other authors have also shown that NC is directly associated with subclinical atherosclerosis in HIV-positive and negative people, and also occurs independently in traditional risk factors (smoking, hypertension, elevated LDL, above acceptable blood glucose, and abdominal adiposity) (5,33).
It is important to highlight that the values of cut-off points selected are specific to the population with HIV, nevertheless studies with this public are scarce in the literature. However, it is of great importance to this population because they present the aggravating factor of ART use that is associated with serious adverse effects, such as metabolic alterations, abnormal redistribution of body fat and strong predisposition to the onset of cardiovascular complications (27,34).
The present study describes for the first time in people with HIV the usefulness of NC to assess cardiometabolic risk and truncal obesity, by proposing cut-off points for this anthropometric variable, especially in men. Moreover, it is evidenced by its high correlation with anthropometric indicators of adiposity, being higher in man. Other authors also report tendencies that are similar to those found in different populations (19,20,27,35).
The good AUC values for NC in man found in the present study suggest high measurement accuracy, considering that a diagnostic test is only considered to be able to discriminate reliable results when the AUC is greater than 0.5 and closer to 1.0, indicating a greater ability to discriminate between individuals with and without risk (36,37,42). In women with HIV, the assessment should be done with caution.
All cut-off points selected in the study presented a balance between sensitivity and specificity of diagnosis. However, the optimal cut-off points of males showed better diagnostic accuracy rates than those of females. Other authors also use the ROC curve and LR analysis, which help in refining and choosing the diagnostic test (35,38).
Positive and negative likelihood ratios assist in the selection of the cut-off point value that is most associated with the risk of cardiometabolic complications and excess body fat, using WC and BMI. The usefulness of LR is to describe the accuracy of a test, since high LR + values provide strong evidence for the diagnosis of true positives while low LR- values exclude the possibility of false positives (35,37,38). Regarding the predictive values of the analysis, it is necessary to understand that they are not fixed characteristics of the test and cannot be generalized to populations with different prevalence of the disease (21).
The reference values for NC in people with HIV are non-existent, making it difficult to compare the cut-off points determined in the study, besides the impossibility of comparing the percentages of sensitivity and specificity, AUC, LR+, LR- and percentages of PPV and NPV. However, it presented sensitivity and specificity percentages similar to those of the study by Onat et al. (20) performed on Turkish adults who had their cut-off points adopted as a reference of risk classification for this article.
There are authors who state that increased NC contributes to the risk of metabolic syndrome, because, as it was previously discussed, this measure reflects fat deposition at an ectopic site, as observed in fatty liver or thoracic visceral adipose tissue which may include (basal areas of) neck and palate (20,39,40).
It is important to highlight some limitations that should be taken into consideration since a cross-sectional study limits to some extent its interpretation of the causality of the associations, besides the fact that correlations with imaging and lipid profile exams that directly quantify fat deposition and their reference values that guide the diagnosis for risk of complications were not performed. Relevant aspects include the use of statistical analysis of LR, PPV and NPV, which help in refining the results of the diagnostic test.
CONCLUSION
The results of this study showed that NC may be an indicator of health in people with HIV, as it is a screening tool capable of identifying the risk of cardiometabolic complications and upper-body fat accumulation, especially in man. The ease of application and low cost can make it feasible to be used in public health services and in epidemiological studies. We emphasize that further research with this population is needed to reach a consensus on specific cut-off points that help to identify early, through screening, people most vulnerable to developing such complications. In addition, investigations with more specific indicators that can better clarify the different findings between men and women are opportune.