Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.108 no.11 Madrid nov. 2016
https://dx.doi.org/10.17235/reed.2016.3841/2015
CASE REPORTS
Hirschsprung disease with debut in adult age as acute intestinal obstruction: case report
Enfermedad de Hirschsprung en el adulto que debuta como obstrucción intestinal aguda. A propósito de un caso
José Antonio López-Ruiz, Luis Tallón-Aguilar, Laura Sánchez-Moreno, José López-Pérez, Felipe Pareja-Ciuró, Fernando Oliva-Mompeán and Javier Padillo-Ruiz
Emergency Surgery Unit. Department of General and Gastrointestinal Surgery. Hospital Universitario Virgen Macarena. Seville, Spain
ABSTRACT
Hirschsprung's disease is characterized by absence of ganglion cells in submucosal and myenteric plexus of distal bowel. Most cases become manifest during the neonatal period, but in rare instances, this disease is initially diagnosed in adult age. It usually presents as severe constipation with colonic dilatation proximal to the aganglionic segment. The treatment is surgical, removing the aganglionic segment and restoring continuity of digestive tract. The disease rarely presents as an acute intestinal obstruction. We report a case not previously diagnosed, which presented as a massive colonic dilatation with a maximum diameter of 44 cm, with imminent risk of drilling that forced to perform an emergency surgery. We include a review of existing literature.
Key words: Hirschsprung disease. Megacolon. Intestinal obstruction.
RESUMEN
La enfermedad de Hirschsprung consiste en la ausencia de células ganglionares en los plexos submucosos y mientérico del intestino. Suele diagnosticarse en el periodo neonatal, siendo muy poco frecuente que se descubra en el adulto. Suele presentarse como estreñimiento severo con dilatación cólica proximal al segmento agangliónico. El tratamiento es quirúrgico, extirpando el segmento agangliónico y restableciendo la continuidad del tubo digestivo. En muy raras ocasiones, esta enfermedad se presenta como un cuadro de obstrucción intestinal aguda. Presentamos el caso de un paciente, no diagnosticado previamente, que debutó como un cuadro de dilatación cólica masiva, con un diámetro máximo de 44 cm, con riesgo de perforación inminente, lo que motivó la realización de una cirugía urgente. Incluimos una revisión de la literatura existente al respecto.
Palabras clave: Enfermedad de Hirschsprung. Megacolon. Obstrucción intestinal.
Introduction
Hirschsprung's disease (HD) is a malformation of the large intestine characterized by the absence of ganglion cells in submucosal and myenteric plexus, which produces a functional obstruction and dilatation proximal to the affected segment (1). This congenital disease is usually detected in neonatal period. It is rarely diagnosed in adult age. Approximately 300 cases have been reported in literature. These patients tend to have milder forms of the disease, in which hypertrophy of innervated proximal colon compensates the functional obstruction by lack of innervation of the distal area (2). We report a case of a 54-year-old male patient that was admitted in the Emergency Department because of a massive megacolon that required a total colectomy with ileum-rectal anastomosis.
Case Report
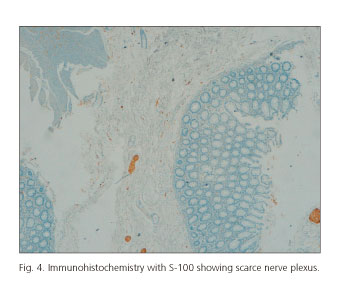
A 54-year-old male was admitted in the Emergency Department by generalized abdominal pain accompanied by anorexia of several days duration. Previous history of meningioma operated in 1998, intestinal resection in childhood (unknown etiology), chronic constipation, smoker of 20 cigarettes per day and moderate drinker. The patient reported difficulty for expelling gases, although he expelled stools without pathological products. No nausea or vomiting. No fever. Exploration showed a hemodynamically stable patient, eupneic with blood pressure 138/97 and heart rate 100 beats per minute. Abdomen was very distended and tympanic, with previous laparotomy scar, painful on palpation diffusely. Peritoneal irritation was not found. Peristalsis was present. Abdominal X-rays showed a dilated colon occupying abdominal cavity. Laboratory studies revealed leukocytosis with left deviation and elevated C-reactive protein. A CT scan was performed, showing a massive dilatation of sigmoid colon, which compresses liver to the right upper quadrant, stomach into the left upper quadrant and bowel loops into the right flank (Figs. 1 and 2). A transition zone was appreciated in distal sigmoid colon. Rectum had a normal size. Peripheral aerial imagery was found in the dilated segment, gas-like wall, which is thickened in this segment. Given these findings, emergency surgery was decided. A midline laparotomy was performed, finding a massive dilatation of sigmoid colon, attaining a diameter of 44 cm at its more dilated portion. The rest of the colon was also dilated. Rectum had normal caliber. It was decided to perform a total colectomy with ileum-rectal anastomosis. After 24 hours, the patient presented hemodynamic instability, with severe abdominal pain. CT scan was performed, showing signs of peritonitis caused by dehiscence of ileum-rectal suture. Emergency surgery was indicated, performing an anastomosis resection and end ileostomy. Postoperative evolution was torpid, with difficulty feedback by adynamic ileus and infection of surgical wound. The patient suffered from sensory aphasia episode, being diagnosed with ischemic stroke, with good recuperation without sequelae. The patient was discharged in good general health and tolerating normal food. The pathologist's report showed the existence of ulceration foci with acute inflammation in the submucosa. Observing the Meissner and Auerbach plexus with immunohistochemical techniques and enolase S-100, loss of neurons (ganglion cells) and lower density of such plexuses were observed with respect to a normal colon (Figs. 3 and 4). There was neuronal dysplasia with scarce presence of ganglion cells on both edges of resection. Pathological diagnosis was Hirschsprung disease.
Discussion
Hirschsprung's disease affects about 1 in 5,000 live births and usually presents in neonatal period. Only a small number of cases remain undiagnosed after 5 years of age (2). Only 300 cases of HD have been described in adults, with male predominance in a 4:1 rate (1,3). The age of patients ranges from 10 to 73 years old. Fifty per cent of the patients are younger than 30 years of age (3). Nowadays its incidence in adult is unknown as this diagnosis is often overlooked in adult population (4).
The primary defect is absence of ganglion cells in Meiss-ner plexus (submucosal) and Auerbach plexus (myenteric) in the affected segment of large bowel. This is the result of a lack of migration of neuroblasts from the neural crest to the large intestine during embryonic period. Other proposed mechanisms include defects in the neuroblast differentiation and accelerated destruction of ganglion cells in the intestine (4). Over eight mutations have been detected in this disease, being RET proto-oncogene the most frequent one (50% of familial cases and 20% of sporadic) (5). Aganglionic segment remains permanently contracted, while proximal segment retains peristalsis, resulting in hypertrophy, megacolon and sometimes perforation of normally innervated segment (2).
Symptoms include constipation refractory to treatment, often from childhood, varying degrees of abdominal distention and pain (83-86%), with frequent palpable fecal mass (50-56%), or fecal impaction (25-36%). Abdominal pain and defense are common (40-80%). Most patients seek regularly enemas for defecation (73-92%), whose frequency ranges from once a week to once every 2 months (3). Fecal incontinence is not typical in adults, unlike children.
The diagnosis of HD in adults is much harder than in children, due to their rarity as they are often short or ultrashort aganglionic segments, which produce mild symptoms in early stages of the disease. Plain films typically show a massive expansion of proximal colon, with a small distal segment. A CT scan is a useful tool, not only to show the transition zone, but to exclude other causes of chronic constipation and megacolon in adults, such as colorectal cancer, volvulus, stricture, slowing of colonic motility, Chagas disease, anatomical or functional obstruction to defecation or idiopathic megacolon (2). The diagnosis is made by barium enema, anorectal manometry and rectal biopsy. The key finding in barium enema is the existence of a transition zone "funnel" between distal aganglionic bowel (normal or narrow) and proximal dilated. Not displaying this transition zone does not exclude the diagnosis of HD. Anorectal manometry shows lack of relaxation of internal anal sphincter in response to rectal distension. Confirmation of diagnosis is provided by rectal biopsy of narrow segment (93% sensitivity and 100% specificity) (6). The rectal biopsy should be made on the back side of rectum, about 6 cm height, and it shows absence of ganglion cells, nerve fibers hyperplasia and an increased level of acetylcholinesterase (7).
The treatment is surgical, in order to remove the aganglionic segment and restore digestive continuity. The surgical approach will depend on length of aganglionic area, length and reversibility of colonic dilatation, and nutritional status of patient. In our case, we are in a situation of irreversible dilatation of entire colon, so we opted for a total colectomy, restoring intestinal transit by ileo-rectal anastomosis. Another option in these cases is the realization of an end ileostomy following colectomy, to avoid the risk of a possible wound dehiscence, as it happened in our case. The disadvantage of this technique is that it requires a new intervention to restore the intestinal transit. The choice of either technique will depend on general condition of patient and abdominal conditions (existence of pollution, peritonitis, etc.).
Several procedures have been designed to treat HD, of which the most important are the following (7):
- Swenson technique: The aganglionic segment is sectioned into the abdomen. This segment is everted and extracted by transanal way. Then we proceed to perform a resection and anastomosis between healthy colon and anal mucosa.
- Duhamel technique: In this case, the aganglionic segment is not removed, but a rear dissection is performed. The healthy colon is descended from behind of the aganglionic segment, performing the anastomosis between the two segments (Fig. 5). With this technique an extensive dissection of the anterior wall of the rectum is avoided, thus avoiding the risk of injuring adjacent structures.
- Soave technique: A resection of distal rectal mucosa of the aganglionic segment is performed, maintaining muscular wall of this segment. Then, normal colon is lowered through the aganglionic segment, making an anastomosis at level of Morgagni columns.
- Myomectomy: can be used in HD with ultrashort segment. It consists in a rear section of muscular wall of rectum starting from dentate line (by transanal way), which removes some of the top segment of internal anal sphincter, getting relief stenosis.
Given the low incidence of HD in adults, it is difficult to compare different procedures. In recent years, the Duhamel technique has been considered as the best option. Compared with the Soave and Swenson procedures, it is superior in terms of impotence rate, anastomotic dehiscence and reservoir function to minimize soiling (8). Myomectomy has the advantage of being technically easier and presenting a low morbidity, but it has worse functional outcomes and can only be used in ultra-HD (7,8).
We can conclude that HD is a rare entity in adults and should be suspected in patients with megacolon with a history of constipation refractory to treatment since childhood. As in our case, it may rarely occur as massive colonic dilatation with risk of perforation, which requires emergency surgery.
References
1. Bakari AA, Gali BM, Ibrahim AG, et al. Congenital aganglionic megacolon in Nigerian adults: Two case reports and review of the literature. Niger J Clin Pract 2011;14:249-52. DOI: 10.4103/1119-3077.84032. [ Links ]
2. Chen F, Winston J, Jain S, et al. Hirschsprung's disease in a young adult: Report of a case and review of the literature. Annals of Diagnostic Pathology 2006;10:347-351. DOI: 10.1016/j.anndiagpath. 2006.03.017. [ Links ]
3. Miyamoto M, Egami K, Maeda S, et al. Hirschsprung's disease in adults: Report of a case and review of the literature. J Nippon Med Sch 2005;72:113-20. DOI: 10.1272/jnms.72.113. [ Links ]
4. Fu CG, Muto T, Masaki T, et al. Zonal adult Hirschsprung's disease. Gut 1996;39:765-7. DOI: 10.1136/gut.39.5.765. [ Links ]
5. Martucciello G, Ceccherin I, Lerone M, et al. Pathogenesis of Hirschsprung's disease. J Pediatr Surg 2000;35:1017-25. DOI: 10.1053/jpsu.2000.7763. [ Links ]
6. Arshad A, Powell C, Tighe MP. Hirschsprung's disease. BMJ 2012;345:e5521. DOI: 10.1136/bmj.e5521. [ Links ]
7. Faucheron JL, Poncet D, Voirin D, et al. Maladie de Hirschsprung chez l'adulte. In: EMC. Techniques chirurgicales appareil digestif. Paris: Elsevier Masson SAS;2009. p. 40-602. DOI: 10.1016/S0246-0424(09)43191-1. [ Links ]
8. Vorobyoy GI, Achkasov SI, Biryukov OM. Clinical features, diagnostics and treatment of Hirschsprung's disease in adults. Colorectal disease 2010;12:1242-8. DOI: 10.1111/j.1463-1318.2009.02031.x. [ Links ]
![]() Correspondence:
Correspondence:
José Antonio López-Ruiz.
Emergency Surgery Unit.
Department of General and Gastrointestinal Surgery.
Complejo Hospitalario Virgen Macarena-Virgen del Rocío.
Av. Doctor Fedriani, 3. 41007 Sevilla, Spain
e-mail: wurdalach@gmail.com
Received: 18-05-2015
Accepted: 04-09-2015











 texto en
texto en