INTRODUCTION
Lymphoid follicular proctitis (LFP) is a rare rectal benign lymphoid disease. Patients with LFP often present with special clinical, endoscopic and histological features. Local steroid and/or oral sulfasalazine therapy and mesalazine suppository therapy have been reported 1,2,3,4. Here, we report the case of a patient diagnosed with LFP with endoscopic findings that were dramatically resolved with the administration of mesalazine enemas in less than one month.
CASE REPORT
A 35-year-old man was admitted to our hospital due to intermittent rectal bleeding associated with stools; there was no diarrhea, malaise, fever, weight loss or other systemic symptoms. The patient denied a history of sexually transmitted diseases, anal intercourse and surgery.

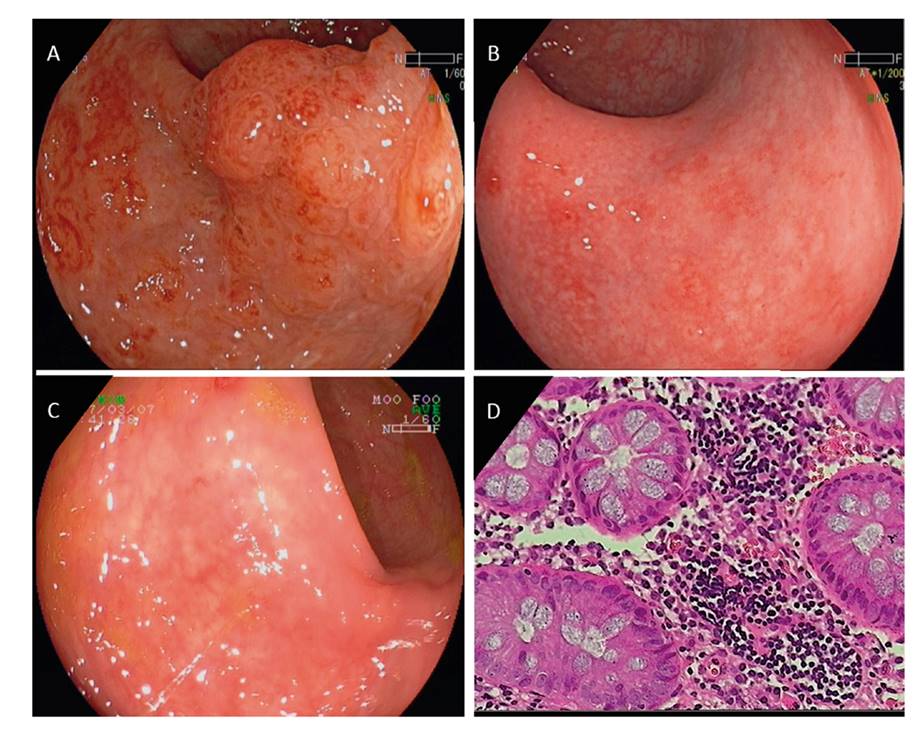
Fig. 1 A. Congested nodules on the lower rectal segment. B. Nodules of variable sizes were detected using an indigo carmine spray. C. Endoscopic ultrasonography showed thickened mucosal and submucosal layers of the rectal wall. D. Biopsy specimens showed dense, abnormal lymphoid infiltrate (HE ×40). E. ESD was performed. F. Histologic examination of ESD specimens showed an excess of infiltrating lymphocytes in the lamina propria of the mucosa (HE ×80).
Total colonoscopy demonstrated nodular mucosa with a top pinpoint-like ulcer from the rectum to the border between the sigmoid flexure and the rectum, whereas the bowel above the rectum was free of lesions. The nodules congested together on the lower rectal segment and occupied 2/3 of the rectal lumina (Fig. 1A). Indigo carmine staining confirmed a pit pattern II type (Fig. 1B). Upper endoscopy, immune function tests and immune-immunoglobulin analyses were normal. Endoscopic ultrasonography showed thickened mucosal and submucosal layers of the rectal wall (Fig. 1C). Biopsy specimens identified dense, abnormal lymphoid infiltrate (Fig. 1D), although immunohistochemical staining demonstrated no evidence of malignant changes. Endoscopic submucosal dissection (ESD) was performed in order to obtain more specimens for histopathological diagnosis and confirm the diagnosis (Fig. 1E). Histologic examination revealed marked lymphoid follicular hyperplasia with prominent germinal centers and a conserved mantle zone. There was an excess of lymphocytes infiltrated in the lamina propria of the mucosa but lymphoepithelial lesions and neutrophils were absent (Fig. 1F). DNA tests for Chlamydia, ureaplasma, cytomegalovirus and Epstein-Barr (EB) virus were negative. Therefore, a diagnosis of LFP was made. The patient was treated with mesalazine enemas of 4 g q.d. Three days later, the patient was asymptomatic. A sigmoidoscopy performed one week after the start of the mesalazine treatment showed a slight improvement of the endoscopic findings (Fig. 2A), with only a few aphthous ulcers left on the rectum 20 days later (Fig. 2B). All the lesions disappeared two months later (Fig. 2C) and histological examination showed no evidence of hyperplastic or atrophic changes and lymphocyte infiltration (Fig. 2D).
DISCUSSION
LFP was first reported by Ball in 1890 5. The tendency for LFP to occur in the lower third of the rectum was reported in 1961 6, however, the pathogenesis is still unclear. A congested, granular and nodular mucosa without ulceration may be found by colonoscopy. It should be noted that nodular mucosa with a top pinpoint-like ulcer was detected in this clinical case. When combined with the pit pattern type using indigo carmine staining, the endoscopic features might favor the differential diagnosis of benign and malignant disease.
Malignant lymphoma, as a lymphoid hyperplasia disease, should be excluded first. It is rare for primary lymphomas to only affect the rectum. The pathological characteristics of lymphoma include significant cytologic atypia, immature lymphoblastic cells scattering beyond the germinal centers and infiltrating through the muscularis propria 2,7. In this clinical case, the provisional diagnosis of low-grade rectal lymphoma was suspected due to the histological examination, although further immunohistochemical examination excluded malignant changes. To reduce the artifacts, ESD was performed to obtain more specimens. The histological examination showed significant lymphoid follicular hyperplasia with prominent germinal centers and a conserved mantle zone. Among LFP patients, mitotic figures are frequent in the germinal centers and absent in the surrounding lymphoid tissue 6. The lamina propria of the mucosa also contains abundant lymphocytes. The lymphoid infiltrates are usually located in the mucosa and the submucosa, whereas lymphoepithelial lesions and neutrophils are absent. Crypt abscesses, crypt distortion, ulceration and granulomas are rarely found in LFP. This may contribute to the differential diagnosis of LFP and inflammatory bowel disease when combined with the clinical and endoscopic features 8.
LFP should also be distinguished from infectious proctitis, especially for Chlamydia trachomatis. Chlamydia trachomatis proctitis is a sexually transmitted disease and patients always have a history of anal intercourse. The endoscopic findings are characterized by hemisphere granular mucosa, and erosion on top of the granule can also be detected occasionally. DNA tests of pathogens can aid diagnosis. In this clinical case, Chlamydia trachomatis, ureaplasma, cytomegalovirus and EB virus were assessed using DNA tests but the results were negative.
There is no consensus for LFP therapy. Although Arai et al. reported that the symptoms and endoscopic findings could be resolved by oral mesalazine administration 9, most previous studies have shown poor effects of oral sulfasalazine administration or topical corticosteroid therapy 3,8. Three studies that included ten cases showed an obvious regression with sulfasalazine or mesalazine suppository 500 mg b.i.d. treatment 1,2,4. Toyoda et al. reported that the clinical symptoms subsided after two weeks of therapy and obvious regression of the rectal lesion was obtained three months later 4. Shami and Waxman reported a mild improvement of the rectal nodularity after one month of treatment and a complete resolution after eleven months 2. Seo GS et al. suggested an average treatment period of 12 months 1. Recently, Gim et al. suggested that pure endoscopic resection was an alternative and effective therapy 10. The incidence of local recurrence is low 6 and no cases in the Seo GS et al. study progressed to other diseases such as ulcerative proctitis or lymphoma 1. In this clinical case, a slight improvement of the rectal nodularity was obtained after one week of treatment and endoscopy revealed a normal rectal mucosa one month later. To our knowledge, this is the first report using a mesalazine enema for LFP therapy. Its therapeutic effect was further identified via follow-up. Mesalazine enema works better than its suppository since the enema makes contact with a larger area of the colon mucous membrane and is absorbed more easily. The long-term outcome of this patient will be observed via further follow-up.
In summary, LFP is a rare rectal inflammatory disease distinguished from ulcerative colitis. Rectal bleeding is the most common clinical symptom and the endoscopic characteristics are congested, granular and nodular mucosa, which is confined to rectum. Histopathological examination shows the polymorphic nature of the infiltrate, absence of significant atypia and abnormal and coalescing hyperplastic lymphoid follicles without acute inflammation. The pathogenesis is unknown. The differential diagnosis includes inflammatory bowel disease, malignant lymphoma and infectious enteritis. Mesalazine enemas could be a promising therapeutic option for LFP therapy. However, the underlying mechanism is unknown.