Background
The practice of Spanish hospital pharmacists has undergone an enormous transformation in the last few decades, to the extent that it cannot nowadays be conceived in isolation from the information and communication technologies (ICTs) that today underpin every sphere of telemedicine1, including both pharmacotherapeutic management and pharmaceutical care (PC). Moreover, in the last few years patients have become increasingly proactive, better informed and empowered, and are now demanding larger amounts of information about their health and greater access to healthcare services amid the growing digitization of health systems2.
In 2008, SEFH, like other national pharmacist associations3-5 designed, under the banner “Safely towards the Future,” the so-called Iniciativa 2020 (Initiative 2020)6, a framework of six strategic priorities and 28 key goals intended to enhance hospital pharmaceutical practice and health system performance. The first strategic priority (“Organizational Development”) was aimed at incorporating new technologies to improve the organization of pharmacy departments and the standard of care they provide, as well as to ensure patient safety and quality of care throughout the pharmacotherapeutic journey. This was also the goal behind the creation of SEFH's Techno Working Group, whose remit is to select and evaluate the technologies available for ensuring appropriate drug use and determining the extent to which drugs can improve individual and collective health7. Recently, SEFH created the so-called Fhusion Working Group to drive transformation of hospital pharmacist practice through digital technologies and the acquisition of digital skills8. Simultaneously with these initiatives, SEFH has since 2014 been working on the MAPEX project, which contemplates the development of a Strategic Outpatient Pharmaceutical Care Map (Mapa Estratégico de Atención Farmacéutica al Paciente Externo)9 aimed, among other objectives things, at promoting the incorporation of new technologies into existing healthcare models. That initiative gave rise to a new PC model called the CMO model (Capacity Motivation and Opportunity)10, which rests on three main pillars: patient stratification, motivational interview and work based on pharmacotherapeutic goals, and permanent contact with patients through new technologies.
On the other hand, European authorities as well as the Spanish central and regional governments have in the last few years expressed their support for the use of telemedicine as a way of improving standards of care. The EU's Momentum initiative11 is aimed at developing a blueprint for the implementation of telemedicine projects in Europe. The Plan de Calidad12 (Quality Assessment Plan) of the Spanish Ministry of Health advocates incorporating telemedicine to specialized medical practice to facilitate access to remote diagnostic and treatment services, avoiding unnecessary patient travel.
In view of the above, the last decade saw the development of Telepharmacy as a specific telemedicine-based PC model, which is now commonly used worldwide. Moreover, different research institutes have conducted indepth evaluations of this new form of PC from the point of view of health outcomes, patient-perceived quality and clinical efficiency13-16. SEFH has recently published its institutional position on Telepharmacy17.
The purpose of this article is to present the definition of the concept of Telepharmacy and SEFH's Position of the issue so as to provide a guideline for the introduction of Telepharmacy into hospital pharmacy services in Spain.
Definition of Telepharmacy
Telepharmacy, a term that has grown to be a widely-used both in Spain and abroad, has been associated with the fulfilment of different kinds of goals through different applications and methodologies. Different professional (in-hospital or community) pharmacist associations have adopted a specific position regarding their understanding of Telepharmacy3-5, to the extent that the concept has come to mean different meanings in different settings. Against this background, SEFH has proposed the following definition17:
“Telepharmacy is the provision of pharmaceutical care at a distance through information and communication technologies”.
Considering the definition above, Telepharmacy encompasses the following activities commonly performed in hospital pharmacy services: therapeutic validation, drafting of clinical documents, provision of PC, therapeutic follow-up of patients, adherence monitoring, drug education and information, coordination between healthcare providers of the same or different hospitals or Primary Care, and evaluation of health outcomes. Like onsite PC, Telepharmacy may or may not be accompanied by home drug delivery, whether it is a drug, an artificial enteral or parenteral nutrition or other therapies or pharmacological agents under investigation.
Telepharmacy procedures
For an optimal provision of Telepharmacy, the service must be rendered in accordance with a standardized procedure and must be part of the offering of any hospital pharmacy service. The provision of Telepharmacy services must be authorized by the Hospital Managers/Directors and/or the corresponding National or Regional Health Authorities and must meet the required quality standards and the regulations that apply to the provision of such services. At the same time, proper implementation of Telepharmacy requires the setting up of a multidisciplinary team in charge of coordinating and developing the service, with clear roles and responsibilities and permanent communication across all clinical teams involved.
Inclusion of patients on a Telepharmacy program must follow strict ethical criteria and be accordingly based on the principle of equity. For that reason, inclusion or exclusion should not be dictated by types of conditions or drugs but rather by the patients' individual clinical, pharmacotherapeutic, personal and social needs, taking into account their level of autonomy, technological skills, risk of social exclusion, socioeconomic status, family and professional dependence, and personal preference. In this respect, SEFH's so-called Modelos de Estratificación y Atención Farmacéutica (Pharmaceutical Stratification and Care Models) may be used as a reference for any decisions to be adopted18.
The electronic clinical record (EMR) should be the basic information system used to provide Telepharmacy services, both when assessing the patients' condition and for recording all the clinical and administrative data relative to the decisions, recommendations and indications of hospital pharmacists.
The evidence available shows that, at the level of PC, Telepharmacy currently encompasses the following activities: pharmacotherapeutic follow-up, patient-directed education and information-dissemination, clinical coordination, and informed home drug delivery7.
Pharmacotherapeutic follow-up
Telepharmacy is a tool that allows hospital pharmacists to conduct a remote clinical-therapeutic assessment of the patient. As such, it contributes toward the chief goal of pharmacotherapeutic follow-up, i.e. ensuring that the pharmacotherapeutic goals established for each patient are achieved. This means that, as a rule, both onsite and remote validation of the therapies administered to in-and outpatients must scrupulously follow the same PC protocols. It is advisable that pharmacotherapeutic follow-up be properly scheduled and conducted in a well-planned manner, based on a consensus between hospital pharmacist, other members of the multidisciplinary team and the patient and/or caregiver.
In addition, patients must be provided with multiple contact channels so that they can effectively communicate with their hospital pharmacist. Such channels must allow two-way communication between them so that joint decisions about any issue or complication arising during a remote consultation can be made in real time or at least as promptly as possible.
Hospital pharmacists, as members of the multidisciplinary team in charge of tending the patient, must perform the following tasks when providing Telepharmacy care (Figure 1):
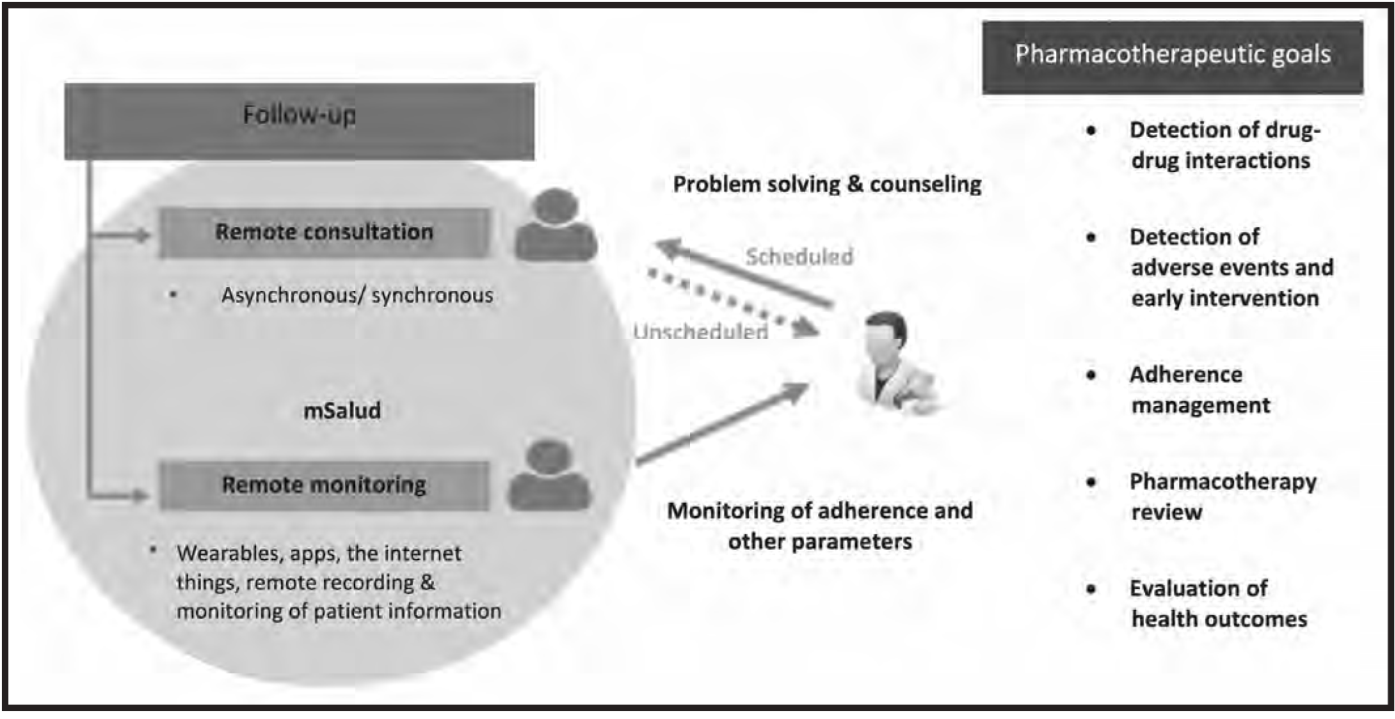
Figure 1. Proposed pharmacotherapeutic follow-up activities to be conducted through telepharmacy(18).
Ensure that the treatment is suitable for the patient it is intended for.
Make sure the patient understands the specifics of the treatment prescribed, examining their preconceived ideas, beliefs and attitudes regarding the prescribed pharmacotherapeutic regimen.
Review the treatment profiles and ensure that the pharmacotherapeutic goals established for each patient are met.
Establish indicators for inappropriate use, abuse, or non-adherence to the drugs prescribed.
Report to the physician treating the patient any issues resulting from poor adherence with the pharmacotherapeutic regimen so that such issues can be resolved by means of a joint strategy.
Stratify or re-stratify remotely treated patients using the available PC models, in accordance with the corresponding systems and variables.
In line with the available evidence, it is recommended that the remote interview with the patient (and/or their caregiver if the patient has consented to giving them access) be carefully scheduled and conducted in a well-planned manner, using the same approach and the same phases as in a motivational interview10.
During the remote consultation, patients will be provided with all the information they need about the treatment to be administered, including information on the following: indication; dosing regimen and length of treatment; route of administration; adverse events and recommendations to prevent them (if any); drug-drug interactions; short-, medium-and long-term pharmacotherapeutic goals to be achieved considering the patients' clinical circumstances; adherence; and the so-called patient-reported outcomes (PROs) for which questionnaires or specific tools to each clinical situation should be used.
The complexity of the remote consultation should be tailored to the patients' level of understanding and to the pharmacotherapeutic goals established. To facilitate the planning process, it is essential to determine the patient's stratification level according to the above-mentioned Modelos de estratificación y atención farmacéutica18.
Scheduled consultations
Remote consultations must be scheduled based on the same circuit as onsite ones, i.e. by managing an appointment in the hospital pharmacy's outpatient consultations register. Patients must be informed that they will be expected to show up as punctually as for onsite appointments. The protocol for administering remote consultations is the same as that for onsite ones, with every relevant detail of the interaction being documented in the patient's EMR and in the hospital's appointments registry. At each consultation, once the pharmacotherapeutic follow-up has confirmed that the patient progressing according to plan, the pharmacist must confirm the continuity of Telepharmacy for that patient and, if necessary, schedule the next informed delivery of the treatment. Figure 2 presents the recommended patient follow-up sequence, made up of scheduled consultations, onsite consultations and treatment dispensation. Every step in the sequence should comply with the standard procedure approved at hospital.
Unscheduled consultations
Remote consultations may be synchronous (via a telephone call or a videoconference) or asynchronous (via email or the internet). The tools used in each case may include options such as wearables or mobile apps, which should allow keeping a comprehensive record of the interactions as well as the remote monitoring of the information provided by the patient.
Patient-directed education and information-dissemination
Telepharmacy is a tool that makes it possible to educate patients and provide them with rigorous, reliable and up-to-date information. It can be used, among other things, as a channel to disseminate and expand information and knowledge. It also facilitates the development of e-learning, providing comprehensive fully-remote education in a manner that helps save time and optimize the use of resources.
Telepharmacy creates a space for discussion and analysis within the domain of health. It improves communication with patients and helps better understand their needs regarding their health and the treatments they may need. It also allows real time measurement of health outcomes thanks to the use of technological tools to process patient-reported health data. As a result, specific follow-up and monitoring strategies can be designed for each patient (Figure 3).

Figure 3. Patient-directed education and information dissemination activities and coordination with the telepharmacy clinical team(18).
Clinical coordination
Telepharmacy is considered an efficient and secure tool allowing hospital pharmacists to coordinate their work with the rest of the multidisciplinary team treating a patient (Figure 3).
Telepharmacy allows the creation of a patient-directed information system, which must then be integrated into the hospitals' own information systems. The information input procedures to be employed must be agreed on by the different clinical teams involved.
During every pharmacy intervention or consultation, onsite or otherwise, hospital pharmacists must enter the relevant information into the patient's EMR so as to enable a multidisciplinary evaluation of therapeutic strategies and the implementation of follow-up plans in the different clinical settings.
Informed home drug delivery
Although Telepharmacy allows for informed home drug delivery to take place in a secure manner, it is essential to carefully plan and organize the delivery circuit in accordance with the possibilities, infrastructure and material means available to each hospital. To facilitate proper coordination and optimization of Telepharmacy procedures, single clinical acts must be favored, ensuring that onsite hospital pharmacy appointments coincide with other appointments in the same hospital. In addition, the scheduling of appointments as well as a register of remote consultations with the hospital pharmacy will be required.
A pre-delivery validation procedure must be established before drugs reach the patients' home. A remote consultation with a specialist hospital pharmacist will be required at the time the drug is delivered in order for the pharmacist to perform an individualized pharmacotherapeutic follow-up of the patient and enter the data into their EMR. It is essential to ensure the confidentiality, security and traceability of the whole process (dispatch, custody, preservation, delivery and reception).
If at all possible, drugs will be dispensed in their original package to allow proper traceability. Furthermore, in order to provide for a single clinical act and/or adjust the doses dispensed and maximize efficiency, drugs may be dispensed in repackaged format or in a labeled blister pack, provided that all official recommendations are followed and that the dose, batch and expiry dates are properly identified.
Resources
It is essential that the relevant government bodies make available the human and material resources required for a proper implementation of Telepharmacy services.
Human resources
All the healthcare providers involved in Telepharmacy (pharmacists, physicians, nurses, etc.) and the patients benefiting from the service should be appropriately educated regarding the use of Telepharmacy tools so as to ensure that the service provided is of the expected standard. In this respect, an education program should be established that provides for technological capacity building and deals with aspects related to effective service provision, procedures, quality and safety standards and communication strategies5.
All healthcare providers involved should also learn to appropriately educate patients in how to make the most of Telepharmacy. The first few training sessions should be held on the hospital pharmacy premises but, after that, more in-depth reinforcement sessions could be held either onsite (consultations, workshops, forums) or remotely (web 2.0). Expert patients could participate in the education of newly signed-up patients; patient associations also play an important educational role through the multiple activities they organize.
A helpdesk should be established to provide users with technical support and assist them along their educational journey clarifying any doubts they may have. It should also help them with functional maintenance of the technologies used, ensuring that the service is provided appropriately. Any agreement entered with Telepharmacy service providers should adhere to the policies, procedures and work standards established. Finally, once a Telepharmacy program has been implemented, it is essential that is should be appropriately honed over time. That is why it is necessary to implement a capacity-enhancement plan that ensures that Telepharmacy services can efficiently cope with the stipulated demand to the required quality and safety standards. A risk assessment program must also be established, accompanied by a contingency plan that ensures that any difficulty arising while the service is being provided can be swiftly addressed.
Material resources. Technology
Material resources, particularly those of a technological nature, are also essential for a successful implementation of Telepharmacy. Apart from providing the groundwork for appropriate PC, such tools must be integrated into the healthcare information and the telemedicine tools already in place in the relevant hospital or regional health system. The security and integrity of patient information and a fail-safe access to information systems must be guaranteed at all times.
Below is a list of the essential technological requirements for an optimal provision of Telepharmacy services5,19:
Healthcare institutions and technology assessment agencies should agree on a standardized methodology for evaluating Telepharmacy or telemedicine tools, guaranteeing their usefulness, quality and attunement to patients' needs.
The (minimum) technological requirements for the development and implementation of Telepharmacy tools should be clearly defined.
The technological tools and components best aligned with the delivery of Telepharmacy services (remote access, data transmission, communications, hardware and software) should be appropriately identified.
A plan should be designed to regularly evaluate the technological solutions available in the market and determine whether they may help achieve the clinical goals established.
Given the plethora of technological tools that may be applied to Telepharmacy, it is essential to design evaluation systems that ensure the quality and usefulness of the tools selected.
Technological tools should be integrated into existing healthcare information and remote medical care systems both at the level of individual hospitals and of the health system as a whole, ensuring interoperability between the different tools implemented.
It is indispensable to involve the management as well as other (information systems, technical, legal, etc.) professionals whose contribution may be necessary to guarantee that any technology used for Telepharmacy complies with the procedures, policies and recommendations required (requirements vary depending on whether Telepharmacy is applied at a national or a regional level).
Working together with the hospital manager/director, a series of goals to be achieved should be established, and a plan should be designed to evaluate and monitor Telepharmacy services.
Strategies should be implemented to mitigate potential risks arising from damaged equipment, inconsistencies in the delivery of care, errors in the protective and/or anti-virus software, hacker attacks, etc.).
Every Telepharmacy system must guarantee data security and confidentiality as well as the protection of all user data.
Legal framework
National regulation
A cursory analysis of the current legislation on Telepharmacy20 might suggest that specialist pharmacist care provided remotely through ICTs or when administering drugs typically administered in the hospital setting at the patient's home is outlawed by the Spanish legal system. Nonetheless, judgement 152/2003 of the Court of Spain21 ruled that the fact that the law requires pharmacists to be present for the performance of their professional duties does not mean that they should personally deliver patients their medications as the task may be entrusted to other personnel. It also stated that dispensation should be carried out as a single act, although the first delivery can be made at the pharmacy and subsequent ones at the patient's home as long as the pharmacist-patient relationship is not compromised. Finally, this Tribunal established that dispensing chronic patients their medications through the mail or by courier is part of the ordinary activity of a pharmacy and does not constitute an infringement of the pharmacist's obligation to protect the patients' health as long as the medications are dispensed in compliance with the doctor's prescription.
Regional regulation
At the regional level, regulation of Telepharmacy is limited to a small number of references to the possibility of dispensing medications at the patient's home in the context of community pharmacy practice22-24. Some Spanish regions however expressly provide for in-house dispensing of drugs typically administered in the hospital setting25-27.
Other legal/regulatory aspects
In addition to the above-mentioned regulations, and taking into account the absence of any legal impediment, hospital pharmacy services should meet a few other legal requirements prior to implementing a Telepharmacy service, such as:
Providing evidence that all the regulations related to clinical documentation and patient autonomy are complied with in the terms set by the national28 and regional legislation.
Implementing all legally stipulated technical, legal29-31 and organizational measures aimed at protecting data privacy when enforcing standardized working procedures, outsourcing external services or developing or acquiring technological patient monitoring tools.
Scrupulously complying with public procurement laws32 (this only concerns hospitals subject to such legislation).
Exceptional regulation during the emergency states
As a result of the COVID-19 crisis, the Spanish Ministry of Health introduced exceptional regulations33 stipulating that regional authorities with jurisdiction over pharmaceutical matters may exceptionally establish exceptional measures to ensure that medications normally administered in the hospital setting can be dispensed elsewhere. As regards drugs undergoing clinical trials, the Ministry authorized regional pharmaceutical authorities to exceptionally provide for patients participating in a clinical trial to receive their medications at home. In these cases, regional parmaceutical authorities may require the sponsors of a clinical trial to make the necessary logistic arrangements under the supervision of the corresponding hospital pharmacy service and the trial's principal investigator. Further to this regulation, all autonomous regions adopted the relevant decisions to immediately implement the measures required to guarantee delivery of medications at the patients' doorstep. They also took steps to authorize the implementation of remote procedures to ensure continued delivery of PC care with the highest levels of effectiveness and safety, promoting adherence.
Research. Innovation. Indicators
Although Telepharmacy has been adopted fairly widely in the last few years, the results obtained following its application have not been evaluated with sufficient rigor. Most of the analyses published are fundamentally descriptive, placing the focus mainly on the structure of the Telepharmacy programs in use, the services delivered, and the processes used to implement them. Few studies have been undertaken to evaluate the results obtained following the delivery of Telepharmacy services, with only a minority of them being randomized and controlled. Moreover, there are very few rigorous studies that compare the health outcomes achieved with the use of Telepharmacy with those obtained when using traditional onsite PC34.
The majority of published studies analyzing the impact of Telepharmacy on health outcomes measure a patient's satisfaction with the care received; the impact of Telepharmacy on patient safety as a function of their pharmacotherapeutic regimen; and the impact of Telepharmacy either on the clinical outcomes obtained in a series of therapeutic areas (asthma, diabetes…), or on therapeutic adherence. Generally speaking, published studies show that both patients and other healthcare providers (physicians, nurses) are satisfied with the performance of Telepharmacy. Improvements have also been reported in the realm of safety and clinical outcomes. Further research is needed nonetheless to confirm these findings34.
Promotion of research and the measurement of the impact of Telepharmacy with agreed-on indicators should be a priority for any pharmacy department implementing a Telepharmacy strategy as this is the only way to guarantee that the service is being delivered appropriately and to the right quality standard. Indicators should allow a joint evaluation of clinical efficiency (impact on the patient's health), technological efficiency and return on investment.
In this respect, measurement of PROs is essential as they are an invaluable source of information on patients' health, quality of life, functional status and social factors. This information ensures a more efficient attunement of Telepharmacy interventions to the patients' needs. It also contributes to an early detection of unrecognized problems, a better monitoring of treatment response and more effective communication between patients and healthcare providers35,36.
For the reasons above and to permit a correct implementation of Telepharmacy in a way that improvements in user satisfaction and clinical monitoring are ensured, it is essential to develop a balanced scorecard to follow-up on the way Telepharmacy is delivered and the results obtained following the implementation of Telepharmacy programs. Below is a list of indicators that could make up the above-mentioned scorecard, which will naturally have to be adapted to the needs and characteristics of each specific Telepharmacy project37.
Patient/caregiver and healthcare provider satisfaction:
Overall satisfaction of healthcare providers, patients/caregivers.
Ease of use for healthcare providers, patients/caregivers.
Usefulness of the information for patients/caregivers.
Impact on the lives of patients/caregivers.
Performance of telepharmacy:
Number of patients and proportion of patients on Telepharmacy vs. total patients.
Number of Telepharmacy consultations vs. total consultations.
Degree of compliance with the Telepharmacy program.
Time to inclusion into the program.
Number of dropouts and reason for dropping out.
Number of incidents and type of incidents registered.
Clinical goals and health outcomes:
Impact of the project in terms of specific pharmacotherapeutic goals.
Impact on PROs.
Cost analysis:
Analysis of costs borne by the patient, the hospital pharmacy and the healthcare system.
Finally, it would be advisable to create a communication channel with SEFH's working groups so as to share information on any Telepharmacy initiatives that may be in the offing. Such a channel would act as a kind of observatory devoted to the identification of initiatives promoted by hospital pharmacies. The observatory could become a Spain-wide point of reference that would help hospital pharmacies establish common criteria, avoid duplicities, and design and implement Telepharmacy research and innovation projects more effectively.
Ethical considerations
Telepharmacy should complement traditional PC, promoting humanization of healthcare and supporting outpatients throughout their care journey with full regard to the relevant ethical and legal requirements. For that reason, Telepharmacy must be grounded in the search for excellence contained in the Spanish Code of Pharmaceutical Ethics (CEEF) and the four pillars of bioethics38, with pharmacists playing the key role in ensuring its proper delivery.
The principle of non-malfeasance, often cited as primum non nocere, implies that hospital pharmacists must offer the pharmacotherapeutic care that best suits the needs of each patient and encourage them to join a Telepharmacy program on the basis of criteria agreed on by a multidisciplinary team or an ad hoc committee39.
Telepharmacy bolsters the bioethical principle of personal autonomy (CEEF principle 4) and uses ICTs to provide patients with rigorous, reliable and up-to-date information (CEEF principle 6), allowing them to participate in the adoption of decisions that by their very nature will have an impact on their health.
When practicing Telepharmacy, hospital pharmacists should ensure due protection of patients with impaired autonomy and respect cultural and personal differences between patients (CEEF principle 8). That is why Telepharmacy must rest on stratification models that prioritize patients who are likely to obtain the greatest benefits from remote PC. Practitioners must ensure patients understand the nature of Telepharmacy and provide them with such oral and written information as may be necessary for them to understand the implications of using Telepharmacy services. Against this background, patients must be willing to participate, give their consent and make a commitment to join a Telepharmacy program, signing the corresponding informed consent form, which should include the information the patient was given both orally and in written form, refer to the patient's co-responsibility in the use of medications, and explain that patients can revoke their consent at any time. Privacy and confidentiality of patient data must be guaranteed at all times, using appropriate protection software and secure access controls. Patient-pharmacist privilege should also be guaranteed (CEEF principle 9). As regards the principle of fairness, universal access to Telepharmacy must be ensured.
Transparency and equity should be embedded in every decision, prioritizing patients according to the severity of their condition and their prognosis, both in business as usual scenarios and in emergency situations such as that arising from the COVID-19 pandemic40.
Telepharmacy is also associated with the bioethical principle of beneficence, which requires pharmacists to maximize patient wellbeing (CEEF principle 1) by means of pharmacotherapeutic follow-up (through remote consultation and remote monitoring) and remote informed dispensing and delivery of drugs. Individualized PC activities must be implemented whenever necessary. Special attention must be paid to patients at risk of exclusion where digital unpreparedness or a vulnerable socioeconomic situation may make remote consultation and remote monitoring unfeasible. In this respect, Telepharmacy promotes beneficence through interactions with patients from geographically remote areas or those with travel limitations because of disease, dependence or a difficult occupational or economic situation. The limitations to Telepharmacy are in any case always derived from the need to abide by the non-malfeasance and fairness principles.
SEFH's Position Statement on Telepharmacy
SEFH considers Telepharmacy a necessary complementary tool to provide specialized pharmaceutical care centered on clinical monitoring, patient education, dissemination of rigorous and reliable information, coordination of the work of healthcare providers from different areas to ensure continuity of the clinical process and a multidisciplinary approach, and informed dispensing and home drug delivery to ensure their availability when needed. All these activities should be geared toward the ultimate goal of clinical care, i.e. improving health outcomes and maximizing patient safety.
SEFH believes that the delivery of Telepharmacy is fully warranted provided that it is set within a clearly defined PC model that rests on quality and safety-driven criteria. Telepharmacy should also comply with the existing laws and regulations concerning health and pharmaceutical care, abide by the ethical principles inherent in healthcare, and follow the humanization-of-care strategy and the code of conduct advocated by the pharmacist profession.
SEFH calls on healthcare authorities, lawmakers, professional healthcare organizations, hospital pharmacy administrators and patient associations to introduce such initiatives as may be required to promote an efficient, secure and humanized use of Telepharmacy both by patients and healthcare providers, and to foster the conduction of research projects into the ways Telepharmacy can influence health outcomes.











 texto en
texto en 



