CASE REPORT
A 41-year-old female, with a personal background for type I obesity and total thyroidectomy due to goiter, in substitutive hormonal treatment with Eutirox. No personal history of peripheral vascular disease was known. As her gyneco-obstetric background, three gestations: one spontaneous abortion and two eutocic deliveries; the first 10 years ago, and the last one approximately one month ago, with a controlled and normal pregnancy, that required manual extraction of the placenta due to retention of the same.
Attends the emergency room due to scanty vaginal bleeding at 14 days postpartum. Physical examination shows an arterial tension of 154/69 mmHg, heart rate of 91 BPM, and temperature of 36°C. External genitalia appear normal. A speculoscopy shows a normal vagina and cervix, with blood clots in the vagina without active bleeding. The cervix is permeable and doesn’t present with pain in response to movement or bimanual palpation. The uterus is contracted, with no abdominal pain.
An ultrasound reveals an anteverted uterus, regular and augmented in size. The cavity is distended and occupied by a heterogeneous image 84 mm in size, with several anechoic zones through its depth, which, via a Doppler, are matched to tortuous blood vessels that not respect the endometrium-myometrium interface, practically throughout the whole uterus. Thinning myometrial wall (4-3 mm), and no free fluid.
It’s decided that no curettage be done due to myometrial thinning, and perforation and active bleeding risks.
Blood tests are carried out, among which stands out a 9.4 g/dl haemoglobin, positive BetaHCG, and normal biochemistry and coagulation. The PCR for SARS-COV-2 comes back positive.
The patient is informed about her therapeutic options, and a hysterectomy is decided upon. During surgery, it was observed that the uterus was enlarged with a mass occupying the right horn without trespassing the serosa, and multiple surface blood vessels at the level of the right horn. The piece is sent to the Pathology Service (figure 1).
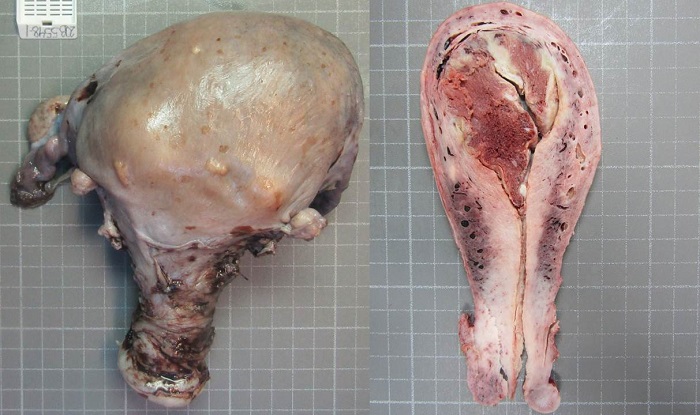
Figure 1. Gross image of uterine specimen. The bisected uterus reveals retained placental fragments within the endometrial cavity.
Macroscopically, an enlarged uterus is observed, 17 cm in size through the largest axis, which displays an unscathed external surface; upon opening, an endometrial cavity occupied by a reddish irregular mass measuring 8x6 cm is observed. Also, vascular structures are observed through the myometrial depth, with dilated vessels and a presence of haematic material within. In the histological study, the mass described in the endometrial cavity corresponds to chorionic villi of mature aspect (some of them necrotized), without proliferation of the syncytiotrophoblast. An absence of decidua was observed in points with implantation of the villi directly on the myometrium (figure 2). The anathomo-pathological diagnosis was Placenta Accreta.
DISCUSSION
Placentary accretism is a relatively rare pathology, in which the placenta implants abnormally, with villi in direct relation with the myometrium, without the presence of decidua in between, which results in the placenta adhering to the uterus and thus extraction difficulty, with risks of postpartum haemorrhage and uterine rupture, ending, on occasion, in hysterectomy. Maternal death can occur1.
In spite of the fact that the exact aetiology of the pathology isn’t known, it has been associated to antecedents of abortions, C-sections, advanced maternal age, a history of multiple pregnancies, previous curettages and structural uterine defects, which would lead to damage to the basal decidua and to an abnormal implantation of the placenta2.
There are different degrees of abnormal placental implantation; placenta accreta (A) is limited to the surface myometrium, showing myometrial fibers within the basal plate; placenta increta (I), where the chorionic villi extend to the depth of the myometrium; and in placenta percreta (P), to the uterine serosa (figure 3)3.
The incidence of postpartum hysterectomy due to placenta accreta is believed to oscillate between 0.2-1.5 per 1,000 births, and related mortality is between 2% and 7%2.
As of today, there is no effective prophylactic, and pre-natal diagnostic tests are done via ultrasound and MRI. In 45% of cases, high serum levels of alpha-fetoprotein have been observed3.
In terms of the effect of the COVID-19 infection on the placenta of pregnant women, emerging publications exist, some without relevant findings, and others where it is described, above all, maternal vascular malperfusion alterations associated to altered maternal blood vessels with decidual arteriopathy, villous infarction and inter-villious thrombi4,5.
A study about manifestations during pregnancy in patients with COVID-19 report two cases of placenta accreta6. Additionally, in another study, microscopical placentary accretism was observed, as well as myometrial fibers joined to the maternal placentary face, but not with a significant increase as compared to control cases5.
These alterations are seen when the infection occurs just before pregnancy or during early pregnancy because is the moment when the virus is able to disturb the endometrial immune response that could produce altered decidualization, placentation and trophoblast invasion, that could lead into placenta accreta spectrum or even preeclampsia.
After consulting the scientific literature, to our knowledge, there is no increased risk of significant placental histopathologic changes if the diagnosis of COVID-19 is in the third trimester, which is the case of our patient, but further studies are required to understand the possible effects of the virus in the placenta in this term.















