Introduction
In Brazil, a large portion of post-acute care, rehabilitation, and chronic patient care is conducted at home through Home Care (HC). Both in public healthcare and in private healthcare, HC can execute with excellence multiple interventions at its patients’ residences. These interventions include administering parenteral medication, providing enteral nutrition, applying dressings for the treatment of wounds, administering continuous oxygen therapy, conducting motor and respiratory rehabilitation therapies, and more complex procedures such as the use of negative pressure dressings, parenteral nutrition, and both invasive and non-invasive mechanical ventilation, offering superior cost-effectiveness compared to that of the hospital care(1,2,3,4).
HC consolidated itself in Brazil in the 1990s(1,2,3). Since then, it has experienced exponential growth, especially in the last decade, which has been further reinforced by the COVID-19 pandemic. According to statistics and estimates presented by the NEAD-FIPE census of Home Care 2021/2022, the private sector of HC serves 346,000 beneficiaries annually(5). It has been estimated that approximately 1 million patients are admitted to home treatment in Brazil each year when considering data from both public and private services. That way, HC is directly responsible for reducing the demand for hospital beds, relieving the overload of hospital services (with low, medium, and high care complexity), and providing safe and qualified treatment to its beneficiaries(1,2,3,(5).
Model of Operation for Home Care in Brazil
HC in Brazil’s private healthcare sector is typically divided into two modalities: Home Assistance and Home Hospitalization(1,4). The first modality, Home Assistance, is intended for patients with less complex care needs who require outpatient healthcare services such as administering parenteral medication routes up to four times a day, conducting motor and respiratory rehabilitation therapies, and applying complex dressings(1,4).
The Home Hospitalization modality is intended for patients with more complex medical and technological needs who require healthcare services such as parenteral nutrition, invasive and non-invasive mechanical ventilation, multiple lower airway aspirations, and multiple daily intravenous medication administration(1,4). Home Hospitalization includes the involvement of a nursing technician, based on the patient’s complexity of care, through continuous nursing care at the patient’s home for 12 or 24 hours. These professionals work on shift duty, which poses challenges and limitations in terms of logistics difficulties and the availability of capable human resources for a safe and quality service at home(1).
The evaluation of the best HC modality for a patient is based on the Home Care Planning Assessment Table, a tool for determining eligibility that was created by NEAD (Núcleo Nacional das Empresas de Serviços de Atenção Domiciliar/National Nucleus of Home Care Services Companies) in 2016. Since then, the tool has been widely accepted and used as a reference in the Brazilian HC market(1).
The private Brazilian HC model provides domiciliary care to patients with high complexity needs. However, in some cases, it reduced the importance of agents essential to the promotion of health and well-being, such as caregivers, family members, and even patients themselves. This assistance matrix established the nursing technician, the least specialized human resource in the chain, as the professional in charge of delivering safe and qualified continuous nursing home care.
Additionally, this system has deviated the Brazilian Home Hospitalization consumer from the HC guidelines, following the assumption that care responsibilities would be fully transferred to the nursing technician. This dependency on this professional, and a concomitant symbiosis between patient and nursing technician, has been detrimental to all players involved in HC. Furthermore, this scenario has contributed to the perpetuation of the phenomenon of judicialization of home health care in Brazil, which directly impacts the sustainability of private providers and HC’s payers.
Judicialization of home health care in Brazil derives from the lack of regulatory environment of the HC private sector by the Brazilian National Supplementary Health Agency (Agência Nacional de Saúde Suplementar - ANS). Brazilian Health Insurance Companies (HIC) and Health Care Service Plans (HCSP) are not required by ANS to cover HC services. Therefore, HC services are granted at the sole discretion of the HIC and HCSP.
When a HIC or a HCSP choose to deny home health care services access, Brazilian Home Hospitalization consumers usually appeal to judicial procedures (through individual lawsuits) based on Brazil´s Consumer Protection Code (Código de Defesa do Consumidor) content and legal jurisprudence that can guarantee their rights to home health care assistance through court decision.
What can we do differently?
Understanding the different models in effect around the world(3,6,7,8,9,10,11,12,13,14,15), and their potential application to the patient profile of Brazilian HC is a crucial starting point for this discussion. This analysis has as its objectives comprehending the existing HC models in effect around the world, understanding the patient profile being treated in Home Hospitalization by a private HC company in Brazil, and, most importantly, proposing a new, cost-effective model of domiciliary care that is based on the best available evidence We suppose this model, once tested, will be able to increase patient satisfaction and clinical outcomes for these patient profiles.
Existing models
Several HC programs have been identified in literature, in congress annals, and through benchmarking, the main ones being: “Melhor em Casa”, from the Brazilian public healthcare system(3), “Hospital in the Home”, from the Queensland State’s, New South Wales(6), and Victoria’s Department of Health(7), in Australia; “Hospital at Home” from the Scotland´s National Health Service(8); “Hospitalización a Domicilio” from Spain’s Sociedad Española del Hospitalización a Domicilio(9); “Hospitalisation à Domicile” from the French Fédération Nationale des Établissements d’ Hospitalisation à Domicile(10) and models proposed by the North American market (11,12).
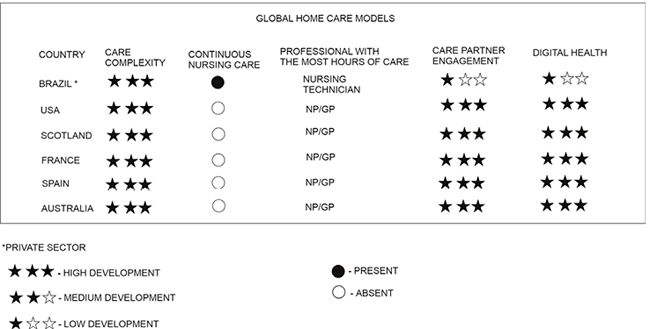
The available evidence in scientific literature specialized in Home Care, Home Healthcare, and Hospital at Home describes the benefits and value generation of European and North American HC models, led by nurse practitioners (NP) and general practitioners (GP), capable and engaged caregivers, patients empowered through self-care, social support services, and a multidisciplinary team of specialists(6,7,8,9,10,11,12,13,14,15), aided by efficient clinical management strategies based on data analysis and supported by digital health resources such as remote monitoring(16,17,18,19,20,21,22), telemedicine(23,24), electronic medical records, and integrated information and communication management systems(25). These models’ characteristics are in Figure 1.
Profile of patients receiving care in the current Home Hospitalization model
To understand the patient profile, a sample of 920 patients receiving care in the Home Hospitalization modality by Home Doctor (Brazil) was analyzed in November of 2022. Out of these patients, 355 were excluded from the clinical analysis because they were receiving HC entirely due to a judicial decision, a situation where the care isn’t defined solely by clinical recommendation, but also by legal opinion, which could potentially contaminate and affect the sample.
Of the 565 remaining patients, 486 (86% of the 565) were assessed by the multidisciplinary team at Home Doctor for a revision of its care complexity and the technological demand of its current domiciliary care. This sample was used as a convenience sample.
The main clinical criterion recognized in the assessed sample for continuous nursing care at home (during 12 or 24 hours) included the need for high-complexity respiratory care (including continuous mechanical ventilation, intermittent mechanical ventilation, and lower airway aspiration through a tracheostomy in patients with no ventilatory support), administration of intravenous medication more than 4 times per day, a history of multimorbidity and frequent hospital readmissions (2 to 3 episodes per year) and palliative care in the final stages of life. Other criteria identified was the concession of continuous nursing care at home (during 12 or 24 hours) by the HIC or the HCSP, often due to social reasons but without evidence-based criteria for Home Hospitalization recommendation.
From the assessed 486 patient sample, Home Doctor multidisciplinary team classified 137 patients (28%) that required continuous mechanical ventilation, 59 patients (12%) that required intermittent mechanical ventilation, 97 patients (20%) that required lower airway aspiration through a tracheostomy with no ventilatory support, 13 patients (3%) that required the administration of intravenous medication more than 4 times per day, 26 patients (5%) who had a history of multimorbidity and frequent hospital readmissions (2 to 3 episodes per year), 16 patients (3%) who required palliative care in the final stages of life and 138 patients (28%) who received continuous nursing care because of a concession from the Health Insurance Company or the Health Care Service Plan provider.
Patients in continuous mechanical ventilation (137) and patients who receive palliative care in the final stages of life (16) have advantages in receiving assistance from a nursing technician at home. This is particularly due to the role of these professionals who can provide immediate treatment of symptoms that require frequent and on demand medical therapy through parenteral routes. These procedures according to the Brazilian Federal Council of Nursing regulations cannot be performed by the patient family and his caregivers, even if they are well educated and have the support of qualified healthcare professionals.
The 333 remaining patients (68,5% of the assessed sample of 486) will be considered eligible for admission to a new standard of Home Hospitalization, named: Hospital at Home (HaH).
Proposal of a new hospital at home model
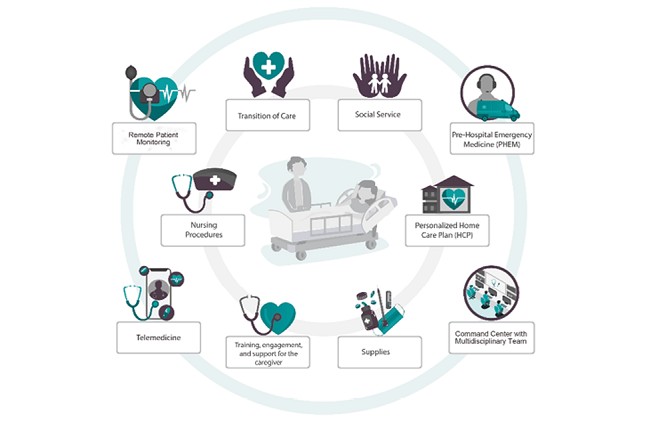
The proposed Hospital at Home (HaH) model is based on increasing the frequency of home visits by key professionals of the HC Multidisciplinary Team (HCMT); increasing the visits from doctors and nurses, who are better qualified to provide excellent care; treatment from specialized doctors as needed; engaging the care partner (the patient, caregiver, and family members), with a decrease in social dependency on nursing technicians, by providing social and technical support to the caregiver. The program is supported by digital health being the most relevant type of resource, of which include a Command Center staffed by a Multidisciplinary Team who provide active monitoring and are clinically proactive with the patients, using remote monitoring tools (Chatbot, Voicebot, and Devices), implementing robust telemedicine, using electronic medical records, and an integrated clinical management system with real-time information. In addition to the above, a rapid response team complements the model, being capable of providing agile treatment at home in case of clinical complications.
The new HaH model is based on 10 pillars (figure 2), which are:
Implementation package for transition of care, consisting of frequent medical and nursing visits during the first week of HC, besides nutritional and physiotherapy services, and a social assistant during this first week
Development of a personalized Home Care Plan (HCP) after the first week of implementation, created by the entire multidisciplinary team involved in the project, with established goals for each individual patient
Execution of specialized nursing procedures on demand up to 4 times per day
Training, engagement, and support for the caregiver(s) to promote the health and well-being of the care partner unit (patient, family members, and caregivers), provided by trained professionals and based on a specific manual with execution and productivity control tools
Active participation of social service through the specialized customer service aimed at reinforcing the role of the caregiver and their responsibilities, emphasizing the technical eligibility of care and the limitations of the services, seeking support networks to assist the caregiving unit in the process of change, and providing guidance on accessing the patient’s social rights
Remote monitoring of vital signs and invasive mechanical ventilation through specialized devices
A Command Center composed of a Multidisciplinary Team that provides remote monitoring, telehealth, and elective or emergency dispatches of HC professionals as needed
Telemedicine
Allocation of necessary resources for healthcare and patient well-being (materials, diets, equipment, and medication according to evidence-based guidelines)
Rapid response team comprising qualified nurses and Pre-Hospital Emergency Medicine (PHEM) through the Emergency Department.
Benefits and challenges of the hospital at home model
The HAH program commits itself to a safe and high-quality transition of care from the hospital to the patient’s residence. It is focused on maximizing the most qualified resources of the HCMT, with support from digital health resources and a rapid response team for domiciliary emergency services, particularly during the first week after home admission, where there are higher medical complications related to healthcare assistance. In this way, it aims to protect patients from the elevated risk of clinical complications and promote greater safety and trust for the patient and their families, with the potential to reduce 30-day hospital readmission rates.
The methodical training of caregivers, which prioritizes them as the mainstay of HC and encourages the patient to prosper as an agent of self-care, combined with the provision of a social support axis by the reception center, will progressively shift the current Brazilian reliance on the nursing technician as an indispensable social element in HC services to a culture grounded on the empowerment of the care partner unit as an advocate for regaining independence, functionality, and well-being of the patient.
Moreover, it will reduce the caregiver’s burden by promoting his well-being through his care skills development allied with strong corporate support (technical, psychological, and social) network provided by the multidisciplinary team, social service, and specialized customer service. Also, it will minimize the waste of nursing hours lacking technical relevance. It is plausible that, in the long run, this cultural change will contribute to the reduction HC judicialization rates providing due to social aspects of care.
The personalized HCP is an ally to the processes mentioned above and reinforces the centrality of domiciliary care to the patient by fulfilling their desire of receiving care in a welcoming and dignified environment, their own home. It enables better governance of the patient reported outcomes and experience measures and supports cost-effective healthcare management.
The specialized Command Center, in conjunction with the Rapid Response Team, will enhance patients’ experience and improve their satisfaction, especially by strengthening their trust and connection with the HCMT. It can increase the efficiency of multidisciplinary coordination in domiciliary care and promote equitable access to HC. It will also facilitate prediction and early intervention of clinical complications, thus possibly reducing the current hospital readmission rates (after the first 48 hours in Home Care) in the Brazilian private HC sector as showed in Figure 3.
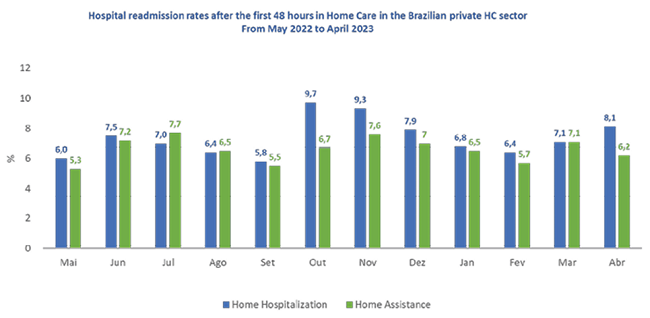
Figure 3. Hospital readmission rates after the first 48 hours in Home Care in the Brazilian private HC sector from May 2022 to April 2023 (SOURCE: NEAD/ IndicAD(26)).
Among the main challenges for the success of HaH is the existence of contractual barriers and funding sources that follow the current Brazilian standard for Home Hospitalization services, which lack the alignment of financial incentives and proportional payment to the incremental costs of HC companies, necessary for the promotion of innovations capable of improving the quality and safety of care.
Brazilian HC clients are often accommodated in a culture of transferring care and fear of judicialization - both forces that can result in social concessions of continuous nursing care, either from payers or legal rulings in response to pleas from patients and their family members - that could be an obstacle to the effective implementation of the care partner as the mainstay of HC, the patient as an agent of self-care, and the cutback of wasted continuous nursing care.
Another obstacle will be aligning the available technological infrastructure in the patient’s home to meet their remote monitoring and telemedicine needs while preserving equitable access. The precision, safety, and real-time access of data sent by remote monitoring devices, coupled with the incorporation of this data into digital health tools such as electronic medical records and enterprise resource planning systems, along with the incrementally rising high cost of innovation, could limit the scalability of information technologies applied to HC.
Conclusion
The Brazilian demographic and epidemiological transition will increase the use of HC services, particularly the Home Hospitalization model. Brazil has an unstable economic and political landscape that contributes to the high inflation of HC costs, forcing the sector to search for formulas that guarantee its sustainability. The current Brazilian Home Hospitalization service model is outdated and too fragile to meet the challenges ahead.
European, North American, and Australian models have proven effective for the delivery of HC at different levels of care complexity. Their use of technology enables connections between patients and healthcare professionals, preventing clinical events and stimulating early interventions, resulting in better patient reported outcomes and patient reported experience for its clients.
The Brazilian HC consumer demands a positive experience resulting from qualified, safe, and humane care in their homes. HC payer sources require lower costs aligned with evidence-based guidelines. Private sector HC companies seek operational efficiency and value creation for their clients to ensure their continuity. The Hospital at Home model presents itself as the transformative model of Brazilian HC, as it reshapes the pillars of HC, being capable of improving coordination and management of HC patients’ pathways, ensuring evidence-based interventions supported by data management and efficient resource control.
The HaH model could provide key tools for the Brazilian HC private sector. It could set up the groundwork for value-based Home Care and contribute to the sustainability of HC market in Brazil.