INTRODUCTION
Becoming a mother is a wish or a dream that every woman in the world possesses universally and implicitly. But this dream of motherhood is not always pleasant for all, as some may experience few nightmares through their journey. Ectopic pregnancy (EP) is one of them, and it can be fatal. When a fertilized ovum is implanted outside the usual uterine cavity, it is called an ectopic pregnancy [1]. Worldwide the ectopic pregnancy accounts for 1-2% of all pregnancies, and it is a thoughtful cause of maternal morbidity and mortality [1, 2]. Ectopic pregnancy risk factors are closely linked to conditions that alter the normal function of fallopian tubal transport. It is thought that the more damage to the fallopian tube, the greater the chance of an ectopic pregnancy occurring. There are many risk factors for ectopic pregnancy, including Prior ectopic pregnancy, h/o infections in the reproductive system, multiple sexual partners, miscarriage, induced conception period, current intrauterine contraceptive device (IUCD) use, prior caesarian section (CS), and cigarette smoking at the time of conception are all factors to consider [3]. Other factors are prior tubal surgery, tubal sterilization, and history of abortions [4], maternal age, and parity, pelvic and abdominal surgeries [5]. Despite these facts and knowledge, there is a lot to be learned about these factors. For example, these factors' exact role and strength have not been definitively determined in our area. Moreover, extrapolation of results from studies conducted before but at other regions is difficult, owing to the variation in incidence and risk factors associated with EP among different populations studied. This study will help us to prepare a list of risk factors associated with ectopic pregnancy in our state. It will help implement a risk-reduction counselling program before conception, which will help us screen high-risk patients and further reduce and manage EP.
MATERIALS AND METHODS
The present study was conducted over a period of two years in the Department of Obstetrics and Gynecology, Lal Ded Hospital, an associated hospital of Government Medical College, Srinagar, from September, 2016 to August, 2017 and in the Department of Obstetrics and Gynecology, Sri Maharaja Gulab Singh Hospital, Government Medical College Jammu from August, 2018 to July 2019. Cases included all patients with ectopic pregnancy admitted in labor. A total of 192 cases were taken, out of which 8 cases refused to participate in the study, so 184 subjects were included. Age-matched women with a typical intrauterine pregnancy of the same gestational age reported to the Outpatient Departments of both hospitals served as controls.
The inclusion criteria were: 1) histologically proven diagnosed cases of ectopic pregnancy; 2) both newly diagnosed and chronic ectopic pregnancy cases were taken; c) the findings were history-based and available previous records. In addition, the exclusion criteria were: 1) the cases which were not histologically proven were not taken in the study; 2) those patients who left the study or had not reported with the histopathology report were excluded from the study.
All subjects (both cases and controls) were interviewed, records were checked, and complete history pertaining to the following were recorded:-Infertility, any pelvic inflammatory disease (PID), abortions: spontaneous or induced, previous ectopic pregnancy, intrauterine contraceptive device usage, oral contraceptive pills usage, induced conception cycle, tubal sterilization or other tubal surgery, prior CS, cigarette smoking at the time of conception, tuberculosis (TB) in the past (also, TB-PCR of histopathology sample is positive) and endometriosis. In addition, detailed clinical examination was done in dorsal position after the evacuation of the bladder, including general physical examination, systemic examination, per abdomen, per speculum, and per vaginal examination.
Following investigations were done as per the proforma designed for the study:- Blood for Hemoglobin (Hb), Bleeding time (BT), Clotting time (CT), Urine routine examination, ABO/Rh blood typing, X-ray chest (Posteroanterior view), electrocardiogram (ECG), blood urea, creatinine, Na+, K+, and sugar, urine for -human chorionic gonadotrophin (using a commercially available kit) and ultrasonography abdomen and pelvic organs. Histopathological examination was done in cases where laparoscopy or laparotomy was done.
STATISTICAL ANALYSIS
MS Excel and SPSS Version 21.0 were used to conduct the data analysis. Age was described using mean and standard deviation. For two classes, the means were compared using the student's t-test. The proportions were compared using either the chi-square or Fisher's exact test. Odds ratios with 95% confidence interval were calculated. To estimate the risk factors for ectopic pregnancies, logistic regression analysis was applied.
RESULTS
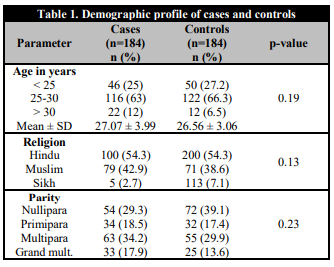
As is evident from Table 1, maximum females were in the age group of 25 to 30 years, but both the groups were almost similar in characteristics on age, parity, and religion.
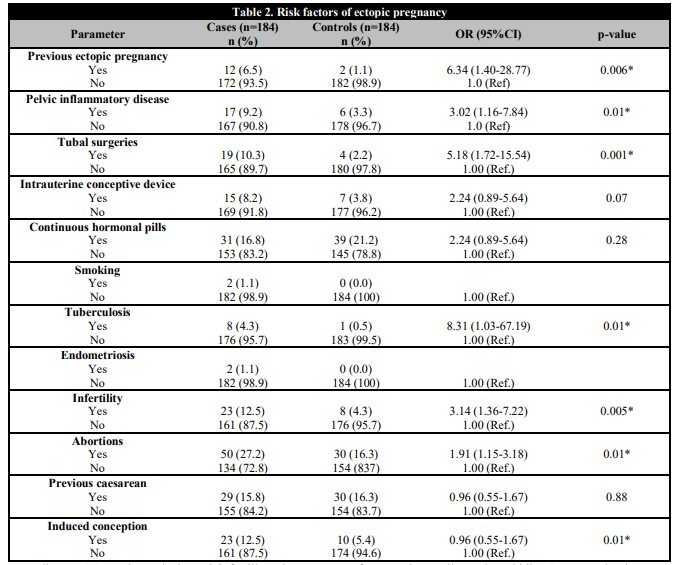
As depicted in Table 2, Patients with previous ectopic pregnancy have 6.34 times increased risk of a repeat ectopic pregnancy (odds ratio 6.34, confidence interval 1.40-28.77), and this association was highly significant (p = 0.006). The risk of having an ectopic pregnancy is 3.02 times increased (odds ratio 3.10; 95% confidence interval, 1.16-7.84) if patient once had PID and is statistically significant (p = 0.01) It is also seen that 17 (10.3%) patients with ectopic pregnancy had a history of tubal ligation or some other tubal surgery done in the past compared to 3 (2.2%) patients among controls. This finding is statistically highly significant (p = 0.001).
In addition, more patients with IUCD insertion had an ectopic pregnancy and more controls were on continuous hormonal pills (OCPs), but the results were found to be statistically not significant (p = 0.07; p = 0.26) respectively.
Attending to TB, endometriosis and infertility, there are 8.31 times increased risk of ectopic pregnancy in patients with tuberculosis (odds ratio 8.31; confidence interval 1.03-67.19), .and this is statistically significant.
Whereas only two patients with endometriosis had ectopic pregnancy, and none of the patients in the control group had increased odds ratio. But with infertility as risk factor, there is 3.14 times increase risk of ectopic pregnancy, which is statistically significant.
Finally, abortions and induced conception pose a significant risk factor for ectopic pregnancy, whereas previous cesarean sections were not found to increase the risk factor for ectopic pregnancy.
DISCUSSION
Ectopic pregnancy is a common obstetrical emergency in early pregnancy worldwide that remains a significant cause of maternal mortality and morbidity. In our study, the mean age ± Standard Deviation) of the ectopic pregnancy group was 27.07 ± 3.99 years, and that of controls was 26.56 ± 3.06 years. Based on our results, the average maternal age was higher for women with EP than controls, which was similar to other studies [6, 7]. “Some previous studies found that the risk of EP increases with advancing maternal age, but the existing evidence on how advanced maternal age has an effect on EP risk remains unclear.”
Our study found, 80.99% of females were multigravidae. In our study, we specifically noted that younger multigravidae were particularly affected. However, this distribution has not been compared in other similar studies [8]. The higher incidence in multigravidae could be explained due to the previous infection or trauma.
The results of our study showed that the history of previous ectopic pregnancy was a significant risk factor for the subsequent development of an ectopic pregnancy, which was also clear from a meta-analysis [9] and studies in Germany and India [9, 10, 11]. These results confirm the fact that recurrent ectopic pregnancies likely reflect perseverance in tubal pathology and tubal dysfunction [12].
“Similar to other studies [5, 9, 10, 11, 12] we found that, among all the possible risk factors of EP, the strongest evidence is for an association between previous EP and sequent EP. According to our results, the risk of EP was almost 6 times higher for women who had prior EP compared to controls (OR = 6.34, 95% CI = 1.40-28.77). A study on risk factors for ectopic pregnancy in women with symptomatic first-trimester pregnancies indicated that the risk of facing a repeat EP increases intensely with the number of prior EP (OR = 2.98 for one prior EP and OR = 16.04 for 2 or more) [12]. Other research studies also estimated the risk of facing a repeat EP to be between 2.4 and 25.0 [5]. These results confirm the fact that recurrent ectopic pregnancies likely reflect perseverance in tubal pathology and tubal dysfunction [12]”.
“Pelvic infection is one of the most common, serious infections in non-pregnant women or reproductive age. Pelvic infections are usually the result of infection ascending from the endocervix causing endometritis, salpingitis, parametritis, oophoritis, tubo-ovarian abscess and/or pelvic peritonitis. PID is reported to occur in 1% of the 15-25 year age group of young adults around the world and affects around 24-32% of women in India. In developed countries, the annual incidence is estimated to be 10–13 per 1000 women, with 20 per 1000 women being in the age group of 20–24 years. Neisseria gonorrhea and Chlamydia trachomatis have been identified as the causative agents [1, 3, 4, 9, 10, 11]. The results of our study found a strong independent association between prior PID and EP occurrence. The risk of having an ectopic pregnancy is 3.02 times increased if the patient once had PID (p = 0.01). These findings are similar to other studies done in France and Nigeria [13, 14, 15]. Adult females have the highest incidence of Neisseria gonorrhea and Chlamydia trachomatis among any sexually active age group. This population also has an elevated risk of subsequent sexually transmitted infections (STIs) after initial PID, thus putting them at increased risk of associated reproductive health sequelae such as infertility, ectopic pregnancy and chronic abdominal pain.”
“It has been reported that previous tubal surgery is a major risk factor for EP with an estimated OR of 4.7 (2.4-9.5) according to a meta-analysis [9]. Similarly, we found a significant relationship between previous tubal surgery and EP. We could not ascertain whether the increased risk is arising from a surgical procedure or from the underlying problem.”
According to a meta-analysis, they found a 2.5–23-fold increased risk of ectopic pregnancy associated with a history of infertility [9]. Another similar large case-control population study found that the risk of ectopic pregnancy increased with the duration of infertility [13]. The findings of the present study on induced conception cycle are consistent with previous studies [16, 17]. A study on controlled ovarian hyperstimulation as a risk factor for ectopic pregnancy found that Ovulation induction alone was associated with an increased risk of ectopic pregnancy (adjusted odds ratio = 3.98; 95% confidence interval 1.10-14.30). “An association between history of infertility and risk of EP detected in our study may be due to a significant role of hyperstimulation, with high estrogen levels.”
In contrast, Oelsner et al. found that the cause of ectopic pregnancy treated with gonadotrophins lies in the patient, likely due to underlying tubal disease and not in the drug [18]. Large and comprehensive studies are needed. The results of the present study on contraceptive methods are similar to those previously reported.
In the present study, we found an association between abortion and ectopic pregnancy. However, conflicting results have been reported. “Some studies suggest that induced abortion may be a risk factor for ectopic pregnancy [19], whereas many studies in contradictions showed no significant association between induced abortion and ectopic pregnancy [20, 21]. With regard to the available evidence, the cause of this relationship is most likely due to infection, hormonal imbalance, or immunologic factors [11].” Analysis among women with no previous history of ectopic pregnancy showed after controlling main risk factors, prior induced abortion was associated with an increased risk of ectopic pregnancy, which is quite comparable to other studies [22, 23, 24, 25].
The strength of our study was that, it was carried out across the two main referral hospitals for gynecologic and obstetric emergencies. The cases and controls were from the same source of population, which makes this comparison valid. There were few limitations in our study. The first limitation of the study was that the history of pelvic infection was by interview only. Because pelvic infections are asymptomatic in a large proportion of women, interview data may be an insensitive means of determining the occurrence of prior infection. A second limitation of this study was that its sample size was limited.
CONCLUSIONS
Since the incidence of ectopic pregnancy is likely to be considered as an essential role for future fertility, we designed this study to identify the risk factors of ectopic pregnancy in a sample of north Indian women. In the present study, we found that the main risk factors for incidence of ectopic pregnancy are prior ectopic pregnancy, prior tubal ligation, and prior pelvic/abdominal surgery. In addition, ectopic pregnancy was positively related to the previous history of ectopic pregnancy, abortion, cesarean section, and infertility. These findings can be helpful for early diagnosis of ectopic pregnancy to pursue proper medical therapy instead of unnecessarily surgical treatment.