Introduction
The literature indicates that, prior to the COVID-19 pandemic, at least one third of university students suffered from depression, anxiety, stress, or another mental health disorder in the last year evaluated (Auerbach et al., 2016; Auerbach et al., 2018; Rossi et al., 2019). These mental health problems can result in low sleep quality (Milojevich & Lukowski, 2016; Zou et al., 2020), although perceived social may operate as a protective factor (Johnson-Esparza et al., 2021; Rosa et al., 2015). These factors, compounded by elements of social pressure such as modifications in university learning derived from COVID-19 (Khan et al., 2020; Shovo et al., 2021), make it necessary to track changes in prevalence rates as well as the associations between these elements.
Mental health problems in university populations are a worldwide problem, with a pre-pandemic study conducted in 21 countries reporting 20.3% of general psychopathology (Auerbach et al., 2018) and a systematic review that encompassed 40 countries finding 26.1% of depression symptoms and 24.5% of anxiety symptoms (Paula et al., 2020). Locally, recent studies conducted with large samples of university students have reported a prevalence of 46% to 50.5% of depressive symptoms, 45.5% to 54.1% of anxious symptoms, and 51% to 53.5% of stress (Barrera-Herrera & San Martín, 2021; Álamo et al., 2020). Despite the high prevalence of mental health problems reported before the COVID-19 pandemic, the available evidence indicates that, during the pandemic, depression, anxiety, and stress levels rose between 40% and 60% in this population (Díaz-Jiménez et al., 2020; Elmer et al., 2020; Huckins et al., 2020; Husky et al., 2020). Nevertheless, the impact of COVID-19 on these prevalence rates appears to be determined by factors such as financial status, the moment of the pandemic when the data were collected, and the respondents' geographical region of residence (Deng et al., 2021; Zhu et al., 2021).
Low sleep quality is also a frequent problem which, before the pandemic, was already on the rise among university students (Sivertsen et al., 2019), with researchers reporting indexes from 58% to 94% according to the Pittsburgh Sleep Quality Index (Machado-Duque et al., 2015; Ojeda-Paredes et al., 2019; Vilchez et al., 2016). The sleep quality of Chilean university students was already deficient before the pandemic, being marked by episodes of insomnia and daytime somnolence (Durán-Agüero et al., 2019; López et al., 2020). Studies have reported that, during the COVID-19 pandemic, sleep quality decreased (Saadeh, 2021; Son et al., 2020), with mental health problems representing risk factors that increased the poor subjective sleep quality of university students (Ahammed et al., 2021; Zou et al., 2020).
With respect to mental health and sleep quality issues, the available evidence indicates that perceived social support constitutes a protective factor (Johnson-Esparza et al., 2021; Rosa et al., 2015), increasing an individual's chances to successfully deal with the stressors of university settings while also boosting his/her academic performance (Johnson-Esparza et al., 2021; López et al., 2020). Perceived social support has been inversely and significantly linked to depression, anxiety, and stress levels (Kugbey et al., 2015). Good social support (social networks inside and outside the home, as well as living with other people) has also been directly linked to good sleep quality (Kent de Grey et al., 2018). Several studies indicate that social support has a moderating effect on the relationship between mental health and sleep quality, buffering or reducing the negative impact of anxiety and stress on sleep quality while also benefiting sleep, with people who have more sources of social support enjoying better sleep quality (Çivitci, 2015; Pow et al., 2017; Van Schalkwijk et al., 2015; Xiao et al., 2020).
The available evidence indicates that, during the COVID-19 pandemic, young people with better (perceived or received) social support scored higher on subjective well-being and overall psychological health instruments (Huang et al., 2021; Szkody et al., 2021). More specifically, those with better emotional support felt less depressed, while those who interacted less with their peers exhibited more anxiety (Elmer et al., 2020). Furthermore, living with parents and receiving social support from family members were protective factors against anxiety in this period (Akdeniz et al., 2020; Cao et al., 2020). Studies conducted in Chile have shown that, for university students, having problems with family, having a dysfunctional family, or quarreling with friends during the pandemic can worsen their mood (Mac-Ginty et al., 2021; Valdés et al., 2022). Likewise, belonging to a social group and perceiving positive social support is negatively associated with depressive symptoms, both in subthreshold depressive episodes and major depressive episodes (Langer et al., 2022). Doubtlessly, instrumental, informative, or emotional social support from significant others (family, friends, teachers) can help university students to deal with the challenges of this period (Saltzman et al., 2020). This includes the social support provided by social media, which can have a positive influence on young people's mental health during the COVID pandemic (Saud et al., 2020; Van Bavel et al., 2020).
Given the impact of the theoretical and empirical information presented above, it is relevant to verify it using a local sample of university students. Therefore, the objectives of this study are: a) to evaluate mental health (anxiety, depression, and stress) and its impact on sleep quality in Chilean university students, cross-sectionally and longitudinally, before and during the COVID-19 pandemic; b) to determine whether perceived social support can mediate the relationship between mental health (depression, anxiety, and stress) in Chilean university students, cross-sectionally and longitudinally, before and during the COVID-19 pandemic. Furthermore, we have developed the following hypotheses: a) depression, anxiety, and stress symptoms have a direct influence on students' sleep quality, both cross-sectionally and longitudinally, thus, higher depression, anxiety, and stress levels predict sleep quality problems, with this association becoming stronger during the COVID-19 pandemic; b) perceived social support moderates the relationship between students' mental health and sleep quality, reducing the influence of depression, anxiety, and stress symptoms on sleep quality both before and during the COVID-19 pandemic.
Methodology
Design
This study presents two descriptive observational retrospective designs, one cross-sectional and another longitudinal. That is, we conducted a non-probability (convenience) sampling process over two consecutive years with monitoring purposes. One part of the sample answered the survey two years in a row (longitudinal), while other people only did so on one of the years reported in this article (cross-sectional). No interventions were conducted other than the usual ones, nor were directed manipulations implemented considering control cases (non-experimental).
Participants
In 2019, the sample comprised n = 1.619 students enrolled in undergraduate programs (62.3% women; M age: 22.05, SD: 3.01). In 2020, the sample comprised n = 1.862 students (63.6% women; M age: 22.42, SD: 3.70). The sampling frequency in each undergraduate program was 1.0% ± 1.0% (M ± SD), with a maximum of 5.4% for both years. 1.4% ± 1.0% (max.: 5.8%) for 2019 and 1.0% ± 1.0% (max.: 5.1%) for 2020, considering a total of 99 undergraduate programs included in the study. The data were collected in November of each year, which coincided with the start of a lockdown period in 2020. To be included in the study, students only needed to be enrolled in an undergraduate program offered by Universidad Austral de Chile.
Instruments
Sociodemographic Questionnaire. We constructed a sociodemographic questionnaire to collect basic data such as sex, age, semester, and socioeconomic status (by quintile). A quintile is defined as the distribution of per capita family income of the population divided into five equal parts, with quintile 1 representing the fifth of the population on the lowest income and quintile 5 that on the highest income (Ministerio de Desarrollo Social, 2016) (Table 1).
Table 1: Demographic data.

Note.Semester 0 applies to students who have passed fewer than 50% of the first semester courses of their program.
Semesters 13 and 14 apply to medical students who have completed one or more internship modules (within a 7-year program).
Patient Health Questionnaire (PHQ-9) (Spitzer et al., 1999). Evaluates the presence of depressive symptoms in the two weeks prior to administration, according to DSM-IV criteria. The scale comprises 9 Likert format items, scored as “not at all” (0), “several days” (1), “more than half the days” (2), and “nearly every day” (3), which makes it possible to determine the severity of the case and treatment follow-up. This process can yield the following outcomes: major depressive disorder, another depressive syndrome, positive depressive symptoms, and negative depressive symptoms. In this study, we employ the interpretation norms of the version validated for Chile by Baader et al. (2012), which exhibits adequate reliability and validity indexes. According to these norms, the presence of 9 depressive symptoms with scores higher than or equal to 2 plus one of the symptoms of depressive mood or anhedonia indicate the presence of major depressive syndrome. When an individual shows signs of 2, 3, or 4 depressive symptoms with scores higher than or equal to 2, and one of these symptoms is depressed mood or anhedonia, the scale indicates the presence of moderate depressive syndrome. Lastly, 1 or 2 of the depressive symptoms without any other criteria indicate the presence of mild depressive syndrome, while an overall value lower than 2 indicates the absence of depression.
Abbreviated Depression Anxiety Stress Scales (DASS-21) (Lovibond & Lovibond, 1995). Questionnaire composed of three brief, Likert format scales that separately measure anxiety, depression, and stress. It comprises 21 items with four answer choices ranging from 0 (“Did not apply to me at all”) to 3 (“Applied to me very much, or most of the time”). We used the Chilean version, which was validated with Chilean university students and exhibited adequate psychometric properties. The cutoff score of the Depression scale is 6 points, that of the Anxiety scale is 5 points, and that of the Stress scale is 6 points (Antúnez & Vinet, 2012).
Pittsburgh Sleep Quality Index (PSQI) (Buysse et al., 1988). Evaluates sleep quality through 24 self-administered questions that measure 7 components (subjective quality, latency, duration, efficiency, disturbances, use of sleeping medication, and daytime dysfunction), with scores ranging from 0 to 3 points. It was validated in Chile with people over 18 years of age, exhibiting adequate psychometric properties. The following interpretation norms were used in the present study: a score lower than 5 indicates that no sleep problems exist; a score between 5 and 7 indicates that medical evaluation is required; a score between 8 and 14 indicates that medical care and treatment are needed; and a score equal to or higher than 15 indicates a severe sleep problem (Venegas, 2013).
Functional Social Support Questionnaire (DUKE-UNC-11) (Broadhead et al., 1988). Self-evaluation questionnaire composed of 11 Likert format items that assess perceived social support on two dimensions (affective support dimension and confidant support dimension). Overall scores range from 11 to 55, with 33 being the cutoff point. Lower scores are indicative of lower perceived social support. This instrument was validated in 2013 with a sample of 493 Chilean women aged between 18 and 80 years, exhibiting adequate reliability and validity indexes (Rivas-Diez, 2013). In the present study, we employed the overall perceived social support score.
Procedure
The study was approved by the Institutional Review Board for Research on Human Beings of the Faculty of Medicine of the Universidad Austral de Chile. The data were collected in November of each year using a virtual survey composed of a short self-report questionnaire that covered sociodemographic variables (sex, age, year in the program, socioeconomic quintile) and several mental health questionnaires that took the students approximately 20 minutes to complete. Before answering, the students accepted an informed consent that explained that they were participating voluntarily and anonymously. After completing the questionnaires, the participants received immediate feedback on their results, complemented with mental health recommendations, information about available health care networks, and web links for them to learn more about each topic.
Data Analysis
This study was conducted using a quantitative methodology. Data were analyzed using the Statistical Package for the Social Sciences (SPSS) 25.0 and the R Project for Statistical Computing (R Core Team, 2019). First, we calculated the prevalence values of anxiety, depression, stress, social support, and sleep problems using the cutoff criteria of each instrument. We did this for 2019 (n = 1.619) and 2020 (n =1.862), employing the full sets of observations of each instrument and assuming a random origin for the missing values. Then, using the part of the sample that answered in both years (n = 325), we contrasted the scores for each instrument in 2019 and 2020, using the Wilcoxon signed-rank test. Afterward, to gain a clearer understanding of how sleep quality fluctuated between 2019 and 2020, using the same sample, we followed up the flow of each severity level from 2019 to 2020. To do so, we constructed a transition matrix, which is graphically presented in a later section. Lastly, to establish which variables contribute to sleep quality, we employed a multiple regression model. We used the DASS-21, PHQ-9, and DUKE indicators as regressors. We used the overall PSQI score as our dependent variable. To prevent the collinearity derived from utilizing the DASS-21 depression and PHQ-9 as regressors, we performed two regressions, one with the PHQ-9 and another with the DASS-21 depression. We incorporated the DUKE scale as an independent regressor and in interaction with the other regressors to evaluate a potential moderating function. We selected the models using the backward method. Lastly, considering the contextual change between 2019 and 2020, we introduced the year as a regressor. With this variable, we mainly sought to capture changes in settings that are not directly related to the other regressors incorporated.
Results
In order to determine the impact of mental health on the sleep quality of university students, we first characterized the prevalence of sleep quality problems, mental health issues, and the frequency of social support for both years. We found high prevalence rates for mental health problems, with approximately one half of the participants exhibiting mild to severe symptomatology according to the DASS-21. In this regard, we found major fluctuations between 2019 and 2020, as the prevalence of people with no depression or stress problems (DASS-21) dropped by 8%. With respect to the PHQ-9, the prevalence found was 59.5% of moderate or greater symptomatology in 2019 and 77% in 2020, with the categories moderate-severe and severe rising by 6.3 and 6.8% respectively. As for sleep quality, 16.9% of the participants reported experiencing no sleep problems in 2019, while only 12.6% did so in 2020. The participants who required not only observation, but also intervention to overcome their sleep issues, represented 73.6% in 2019 and 75.7% in 2020. Sleep problems worsened over time, with problems requiring treatment and severe problems rising by 6.2 and 1.8% respectively. With respect to support networks, in 2019, 71.2% of the respondents had one compared to only 67.7% in 2020, which constitutes a 3.4% reduction (see Table 2).
Table 2: Prevalence rates of mental health problems (DASS-21, PHQ-9) and sleep problems (PSQI), and social support frequency (DUKE).

Note.Results are shown as percentages (n) for each year and according to the levels of severity yielded by each instrument.
The table also presents changes in percentages.
Results are constructed upon the basis of cross-sectional data.
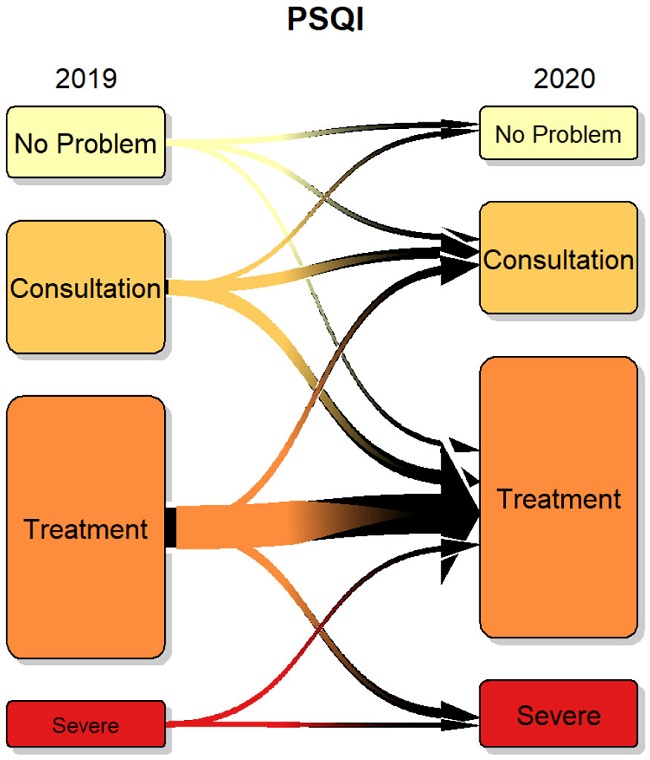
The results reported in Table 2 represent cross-sectional samples from those years; therefore, we cannot establish how severity changed, nor can we determine if the students' symptomatology worsened or if this was a consequence of the changes in the sample of respondents each year. To explore this in further detail, we employed a fraction of the sample (n = 325) that included the students who responded in both years, enabling us to perform a longitudinal analysis. Figure 1 shows the flows of sleep quality from 2019 to 2020, according to the PSQI. The figure indicates how the prevalence of people with no problems decreased, although this was due to the increase in the number of people requiring to consult a doctor or receive treatment. The severe category increased because students who needed to consult a doctor in 2019 needed treatment in 2020. Then, we evaluated whether changes in the scores of each instrument were longitudinally significant. Figure 2 shows that, even though all the scores seem to worsen, this change was only significant for sleep quality and depression (according to the PHQ-9).
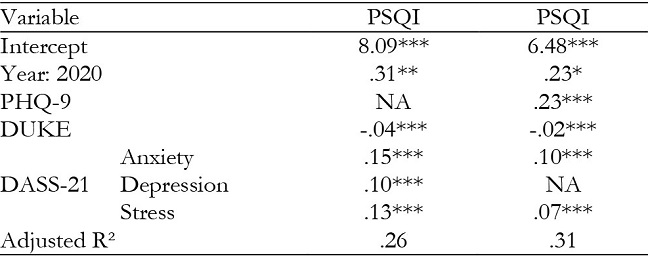
Lastly, we evaluated the possible moderating role of social support in the relationship between mental health and sleep quality; however, we found no significant moderating effects between perceived social support (DUKE) and the rest of the variables. We also evaluated whether mental health variables could predict sleep quality scores. Table 3 shows that all regressors were significant. With respect to depression, the PHQ-9 model explained more variance than the DASS-21 model. All regressors, except for social support, contributed to the worsening of sleep quality. In both models, the year 2020 involved an increase in sleep problems, contributing .31 or .23 PSQI points depending on the model used.
Discussion
The first objective of this study was to evaluate, both cross-sectionally and longitudinally, the impact of mental health on the sleep quality of Chilean university students before and during the COVID-19 pandemic. Our cross-sectional results regarding the prevalence of mental health symptoms, both before and during the COVID-19 pandemic, are in line with a number of studies conducted in university settings that have found worrying rates of anxiety, depression, stress, and sleep disorders (Auerbach et al., 2018; Rossi et al., 2019; Paula et al., 2020). This high prevalence among university students has been ascribed to the complexity of the transition and adaptation stage that these young people are undergoing, which makes them more vulnerable to stress (Barrera & Vinet, 2017; Brook & Willoughby, 2015). Even though this increase in their symptoms may not be caused by higher education in itself, it is often suggested that the daily stressors associated with university life are a significant contributing factor (Beiter et al., 2015; Duffy et al., 2020). The normative stressors mentioned above are compounded by the need to tackle the COVID-19 pandemic which, for university students, involved adapting to a new on-line education model. This new approach is marked by connectivity issues for those living in rural areas, being away from family in difficult times, postponing graduation ceremonies and student exchange trips, and losing part-time jobs due to the closure of many companies and stores, among other problems (Khan et al., 2020). Furthermore, long-term lockdown or social distancing measures may intensify mental health problems (Brooks et al., 2020). Specifically, university students affected by quarantine or lockdown measures have reported stronger feelings of loneliness, depression, and other mental health problems compared to those not affected by such measures (Gritsenko et al., 2021).
Likewise, our longitudinal findings indicate that, between 2019 and 2020, students' perceived support network and the percentage of people with no depression or stress symptoms went down. In addition, we observed an increase in the percentage of students with moderate and severe depressive symptoms in 2020, together with a worsening of sleep problems, as the number of cases requiring treatment rose. These results are consistent with those of international studies with samples of university students during the COVID-19 period, which indicate a worrisome increase in disorders such as depression, anxiety, and stress, as well as suicidal ideation, emotional exhaustion, feelings of fear, irritability, and sleep quality deterioration (Gritsenko et al., 2021; Islam et al., 2020; Odriozola-González et al., 2020).
Our second objective was to evaluate, both cross-sectionally and longitudinally, whether perceived social support can influence the relationship between the mental health and the sleep quality of Chilean university students before and during the COVID-19 pandemic. In this regard, a reduction in perceived social support is an unsurprising outcome, as some studies indicate that the social support provided by classmates or peers covers a large share of young people's psychological needs, even surpassing the impact of family due to their degree of interaction and the similarity of their experiences (Basson & Rothmann, 2018; Bernardon et al., 2011). Although social media may have greatly influenced young people's perception that they received more social support from friends and family during the lockdown period (Saud et al., 2020; Van Bavel et al., 2020), the available evidence suggests that social media as a substitute of physical social relationships may have caused them to feel less happy due to the relevance of non-verbal aspects and physical proximity during communication (Cauberghe et al., 2021). Therefore, if peer support -usually a protective factor that reduces the psychological impact of stressful or unexpected events- decreases, lockdown measures may have a stronger impact on this perception of lessened social support (Xu et al., 2020).
Surprisingly, we found that social support did not have a moderating or predictive effect regarding sleep quality, even though the literature indicates that the severity of sleep disorders is significantly associated with low social support levels (Kent de Grey et al., 2018; Kim & Suh, 2019). Our results also differ from studies that indicate that social support does moderate the interaction between these variables (Pow et al., 2017; Van Schalkwijk et al., 2015). This may be a consequence of the differences between the samples used, as previous research employed men whose average ages were 42.1 and 14.6 years respectively (Pow et al., 2017; Van Schalkwijk et al., 2015) and the respondents in our study were mostly women 22 years old on average, suggesting that the moderating effect could operate differently in such a population. Furthermore, in contrast to these prior studies, the second sample used in our study was collected at the start of a lockdown period in the city, implemented in response to the COVID-19 pandemic; therefore, the number of risk factors and stressors during this period may have weakened the protective impact of social support.
In consequence, our findings only support the first hypothesis presented, indicating that higher levels of depression, anxiety, and stress predict sleep quality problems, with this influence being heightened by the COVID-19 pandemic. This finding is consistent with research conducted before the COVID-19 lockdowns (Kim & Suh, 2019; Vílchez et al., 2016) and afterward (Wright et al., 2020), since deficient sleep patterns are identified as predisposing factors for depression and other mental health problems, mainly among younger people (Itani et al., 2017).
The present study has a number of strengths, such as the large sample used in both years (2019 and 2020) and the substantial number of cases examined longitudinally. However, it also has some limitations, mostly derived from the use of convenience sampling, which limits the representativeness and generalizability of the results. Likewise, the questionnaires were administered on-line, preventing respondents from asking questions to clarify any potential doubts. Furthermore, the respondents have the largest stake in their own mental health, which may have introduced bias. In addition, many students may have been forced to interrupt their mental health treatments during the COVID-19 pandemic because the health care system was overloaded, they feared becoming infected at health care centers, or they had to return to their cities of origin and lost contact with their treating clinicians, among other reasons. This variable was not evaluated, although such factors may have increased the severity of the respondents' mood disorders while also affecting their sleep quality.
Conclusions
The overall results of the present study show that the effects of the year 2020 on Chilean university students were complex, exceeding the family, economic, and academic impact spheres. The results associated with the first objective of this study -to evaluate, both cross-sectionally and longitudinally, mental health and its impact on sleep quality before and during the COVID-19 pandemic- yielded worrying rates of anxiety, depression, stress, and sleep disorders among university students, both before and during the pandemic, which is consistent with research conducted in other countries (Auerbach et al., 2018; Rossi et al., 2019; Paula et al., 2020). Longitudinal follow-up revealed that severity increased mainly for depression and sleep quality, two aspects that require universities to adopt long-term psychological support measures aimed at students, since it has been documented that non-normative stressful events can have a lasting impact on mental health problems and quality of life (Ahammed et al., 2021). The results associated with the second objective do not indicate that social support has a moderating or predictive effect on sleep quality. Nevertheless, it would be interesting to determine under which circumstances social support might play a protective or moderating role and which particular aspects of our sample may have caused our results to differ from those reported by other authors. It is also worth noting that sleep quality appears to be directly affected by young people's mental health problems and that it tends to be underestimated. We expect this study to highlight the importance of sleep quality for mental health, as the literature indicates that sleep hygiene interventions can have beneficial effects such as depression reduction in student populations (Dinis & Bragança, 2018). Examining sleep quality from a preventive point of view can have positive consequences for mental health, posing major practical challenges and delineating a field of study that offers new lines of research.











 text in
text in