My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO  Similars in Google
Similars in Google
Share
Revista Española de Enfermedades Digestivas
Print version ISSN 1130-0108
Rev. esp. enferm. dig. vol.96 n.3 Madrid Mar. 2004
| ORIGINAL PAPERS |
The opinion of patients with inflammatory bowel disease on healthcare received
F. Casellas, G. Fontanet, N. Borruel and J. R. Malagelada
Service of Digestive Diseases. Unitat d'Atenció Crohn-Colitis (UACC). Hospital Universitari Vall d'Hebron. Barcelona, Spain
ABSTRACT
Backgrounds and aim: an item to consider in analyzing a healthcare model for a population group suffering from chronic disease is necessary health-care resources, their use, and their rating by endusers. Regarding inflammatory bowel disease (IBD), healthcare resources used by patients are numerous and varied, and yet they have been never assessed.
Design: an anonymous self-rated questionnaire has been developed with 24 basic questions on overall disease, who is monitoring the patient, how are visits scheduled, need for urgent care, patient view on how control may be improved, etc. This questionnaire was sent to 393 patients who were asked to fill it out and then return it by mail.
Results: two hundred and thirty-seven patients returned a filled-out questionnaire. Most patients were followed up in a hospital, and only 8.8% were being monitored by a general practitioner or area specialist. Ninety-two percent of patients reported visits were routinely scheduled irrespective of clinical status, and 79.6% of patients reported having occasionally presented to an emergency department, because of not knowing what to do or due to having no other resources available in 25.2% of times. This entails that 38% of visits to an emergency unit may be prevented with a better understanding of disease or by means of a phone call. Thirty percent of patients reported that current healthcare is inadequate in terms of contents, form, or waiting time. In all, 97.8% of patients feel that information and knowledge on their disease would help in its control, and 69.6% consider that adequate information would allow them to initiate a proper treatment before visiting their doctor. Family care is another poorly lookedafter aspect that 74.6% of subjects believe would be of help in controlling their disease.
Conclusions: overall, the opinion of patients with IBD on healthcare received is good; however, a number of deficiencies were detected, as is the case with insufficient information, care of family members, and healthcare resources accessibility/agility.
Key words: Health care. Information resources. Inflammatory bowel disease. Ulcerative colitis. Crohn's disease.
Casellas F, Fontanet G, Borruel N, Malagelada JR. The opinion of patients with inflammatory bowel disease on health-care received. Rev Esp Enferm Dig 2004; 96: 174-184.
Recibido: 18-09-03.
Aceptado: 07-10-03.
Correspondencia: Francesc Casellas. Servei de Digestiu. Hospital uniersitari Vall d'Hebron. Pso. Vall d'Hebron, 119. 08035 Barcelona. Fax: 93 489 44 56. e-mail: fcasellas@vhebron.net
INTRODUCTION
A major goal of inflammatory bowel disease (IBD) management is to improve patient health-related quality of life (HRQoL) regardless of the type of therapy used (1). This improves well-being for both patients (2) and household members (3), and reduces sanitary expense (4). Many factors are involved in HRQoL perception; some are directly related to IBD (5), and some are not. Quality of healthcare received stands out amongst the latter in such a way that improved healthcare favors improved HRQoL (6). Therefore, the quality of healthcare received by patients with IBD should be as high as possible, and it should also fulfil the healthcare needs of the population. In this sense, healthcare programs such as the Pla de Salut de Catalunya envisage to preferentially assess user views and expectations on the efficiency and quality of services and healthcare processes (7).
Healthcare resources used by patients with IBD are numerous and varied, since they include medical visits, hospitalization, examinations, surgical procedures, medication expenses, etc. Studies performed in the United States have estimated a mean expense per patient with Crohn's disease per year of 12,417 U.S. dollars (8), with a yearly expense above one thousand million 1990 dollars in that country (9). Crohn's disease has been estimated to generate a total expense of 43.1 million 1994 dollars in Sweden (10). These data give an idea of the financial burden IBD represents for society. However, user use and rating of resources available for IBD patients are poorly understood in our country. Our goal was to establish the use and adequacy of healthcare resources for patients with IBD, and to detect other resources that may be potentially needed. To this end, a study in the form of a cross-sectional opinion poll was carried out, where an anonynous self-report survey was mailed to patients in order to know their opinion on the quality and adequacy of the medical resources they use.
METHODS
Patients
A survey was mailed to 393 patients diagnosed with ulcerative colitis or Crohn's disease who had enrolled in Unitat d'Atenció Crohn-Colitis (UACC), irrespective of main complaint and follow-up center. All patients who returned a correctly filled-out questionnaire have been included.
Method
The survey was mailed to the homes of all participants. Enclosed was a self-addressed stamped envelope for the returning of the filled-in questionnaire to UACC. The survey was anonymous and made up of 24 basic questions on patient social and demographic data, overall disease, controll-ing staff, how visits were scheduled, need for urgent care, rating of healthcare received, view on how control may be improved, suggestions for improved healthcare, etc.
Statistical analysis
When results obtained failed to pass the Kolmogorov-Smirnov normality test, the results of quantitative variables were expressed as median and 25-75 percentiles. Differences between median values were estimated by using the Mann-Whitney test. Differences between proportions were established by using Fisher's test. P values below 0.05 were accepted as significant.
RESULTS
Patients
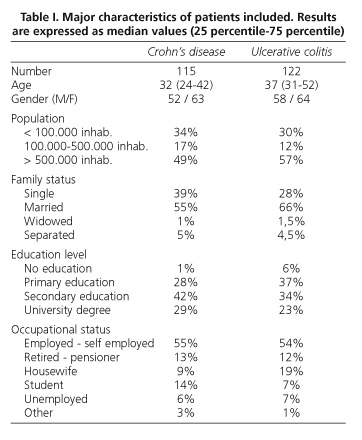
Of 393 patients surveyed, 237 (60.3%) returned a correctly filled-out questionnaire; 115 of these were patients with Crohn's disease and 122 were patients with ulcerative colitis. Major characteristics of patients included are listed in tables I and II. Age was similar in both Crohn's disease and ulcerative colitis groups of patients, and a slight predominance of females was seen in both groups. As expected, most patients in both groups lived in a big city. Family status was also similar for both group of patients, with married patients predominating followed by single patients. Also, education level was similar for both groups of patients. Most had primary or secondary education, and approximately 25% of patients had a university degree. Most patients in both groups were occupationally active, either for third parties or through self-employment. Six percent of patients with Crohn's disease and 7% of patients with ulcerative colitis were unemployed, but the number of cases in which this was due to their disease remains unknown.
Healthcare received
Ninety-four percent of patients with Crohn's disease and 89% of patients with ulcerative colitis were medically followed by a hospital gastroenterologist, whereas only 3 and 8% were followed by a primary care center gastroenterologist, respectively, and 3% in both groups reported being followed by their general practitioner. The high number of patients controlled in a hospital is likely a bias due to the fact that patient recruitment took place in a tertiary referral hospital.
For both Crohn's disease (93.1%) and ulcerative colitis (90.9%) patients, most visits were scheduled in the previous one regardless of disease activity. Only 6.1% of patients with Crohn's disease and 8.2% of patients with ulcerative colitis were appointed when symptoms arose.
The need for urgent visits is a difficulty commonly experienced by patients with IBD, as they require treatment updates when flare-ups or complications arise. Even though most visits are routinely scheduled on the previous appointment, the fact that treatment changes occur with minor delays in 75% of cases is conspicuous, and may be due to phone consultations by the patients, urgent visit rescheduling or self-medication (Table III). When asked "how many days usually elapse from the time you start to feel worse to the time your doctor prescribes you a therapy?", patients surprisingly report a median of merely 1 (0-3.5) day for Crohn's disease and 1 (0-5) day for ulcerative colitis.
A significant number of patients with IBD has to visit a hospital's emergency department sometime. In fact, 85% of patients with Crohn's disease and 75% of patients with ulcerative colitis had at least once been to an emergency department (p = NS between these two groups of patients). Reasons alleged by patients for their presenting to emergency care are listed in table IV. Patients were asked whether in their own view their visits to emergency departments could have been prevented. Most patients (62% of those with Crohn's disease and 61% of those with ulcerative colitis) considered that their visits to emergency departments could not have been avoided. However, 20% of patients in the Crohn's disease group and 21% of those in the ulcerative colitis group reported that their visit to an emergency department could have been prevented, should they have had more information and greater self-monitoring skills. In this same sense, 18% of patients with Crohn's disease or ulcerative colitis considered they might have skipped their visit to an emergency department if they had had a telephone clinic available.
Results obtained for the question "Do you think current healthcare is adequate to control your disease?" are listed in table V. It must be pointed out that most patients in both groups reported that the current healthcare system was adequately meeting their needs. Anyway, a valuable number of patients considered that delays in medical care were excessive, and a smaller number of patients deemed healthcare type inadequate (Table V).
An aspect that was to be established was whether patients considered that care to their immediate environment, e. g. their family members, was necessary for the control of their disease. Fifty-two patients (46%) in the Crohn's disease group and 43 patients (36%) in the ulcerative colitis group answered that care to their family environment was highly necessary to help control their disease. Only 20 patients in the Crohn's disease group (17%) and 36 patients in the ulcerative colitis group (30%) considered that care to their family environment was of no help in controlling their disease. The difference in the proportion of patients who did not consider family care a need was statistically significant between the Crohn's disease and the ulcerative colitis groups (p < 0.05).
Information on IBD
Patients were asked whether they considered information and knowledge on their disease as a relevant item for the control of their health. Results are listed in table VI, which shows that virtually all patients considered having adequate information significant. These data are in contrast with the fact that nearly one half of patients considered they had adequate information but still many doubts, and that 13% of those in the Crohn's disease group and 16% of patients in the ulcerative colitis group considered they had not adequate information (Table VI). Patients were asked whether they considered that they could initiate treatment before getting in touch with their doctor in case of having adequate information, in order to start medication as soon as possible for flare-up symptoms, and most patients in both groups gave an affirmative response (Table VI).
Aspects on which patients considered themselves poorly informed were analyzed, and only 7 patients (6%) in the Crohn's disease group and 8 patients (6%) in the ulcerative colitis group highlighted none of the available choices, suggesting that there was no area of interest on which they deemed more information necessary regarding their disease. However, most patients considered that more information was needed in more than just one area of interest, which they ticked accordingly (Table VII).
Suggestions to improve healthcare
In the questionnaire that was mailed to the patients a blank space was provided for their jotting down suggestions that in their view might contribute to healthcare improvement. Suggestions may be summarized as follows: provision of more information, faster scheduling of visits and examinations, improved accessibility to services, design of psychological help programs, availability of diets and dieticians, setup of integrated care units, more thoroughly informed physicians, support for medical research on the disease, and sensitization of society to IBD.
DISCUSSION
Identifying the healthcare-related needs and views of patients with chronic disease may help rationalize resources and improve care. This is the reason why a survey was mailed to 393 patients with imflammatory bowel disease. Patients were recruited from the records of Unitat d'Atenció Crohn-Colitis in a attempt to obtain patient characteristics with as much variation as possible. Thus, both patients with Crohn's disease and ulcerative colitis, males and females, etc., were included. Time elapsed since diagnosis was 5 years, more than one half of patients needed hospitalization sometime, and 46.1% of patients with Crohn's disease and 13.2% of patients with ulcerative colitis even required a surgical procedure. This reflects disease severity and the fact that patients have ultimately experienced all sorts of healthcare resources. However, against the representativeness of the chosen sample stands the fact that most patients were followed by specialized physicians in third-level hospitals. This suggests a possible bias in sample selection, and the sample would then include fewer patients with less agressive disease who were exclusively followed in primary care centers.
Most patients routinely schedule their visits during the previous one. This system of fixed periodical visits may be disadvantageous in that it may not meet patient needs when an emergency arises because of a flare-up, complications, etc. Notwithstanding, two thirds of surveyed patients reported no delays in medication changes as a result of phone consultations with their doctors, fast rescheduling or simply self-medication. This result is possibly biased, since phone consultations may be easier for patients included as a result of their keeping in touch with UACC, which facilitates and promotes this type of care. Anyway, there is currently a trend to replace fixed schedules with phone "as-needed" schedules, which is preferred by patients even though an agile healthcare system able to adapt itself to urgent needs is required (11,12).
When a health-related difficulty arises that cannot be solved in offices and surgeries, patients present to hospital emergency rooms. This is not uncommon, since 85% of patients with Crohn's disease and 75% of patients with ulcerative colitis reported having presented to a hospital emergency room on occasion. Notions suggested by patients to presumably prevent it stand out simply as much as their extensive use of emergency care. Thus, about 20% of patients reported that they might not present to an emergency room if provided with more information, better self-control capabilities, or a telephone clinics service. This view supports the current trend to set up interactive monographic units such as UACC, in which phone consultations permit ongoing care that is tailored to each patient, with a reduced number of visits in person (13).
Overall, most patients reported being satisfied with the kind of healthcare they receive. However, aspects such as delays in appointments or care to the patient's closest environment, including the patient's family, should be improved. In this respect, inflammatory bowel disease has an impact beyond the patient him- or herself, and also involves household family members, which has an influence on family dynamics and affects relatives' quality of life (3).
Patients attach a lot of importance to being well informed, and a significant number amongst them consider their information inadequate. Multiple media to deliver information to patients and their families exist, which range from in-the-flesh deliveries to deliveries by phone, the internet, handouts, leaflets, video, magazines, books, associations, etc. Informing patients is important, at least because patients who perceive their information is poor report poorer quality of life (14), and acquiring know-ledge on their disease is related to a better emotional adjustment to living with inflammatory bowel disease (15). Anyhow, information must be carefully delivered to patients, since recent observations suggest that handing out information leaflets to outpatients may slightly impair quality of life for a few days (16). However, when asked about the usefulness of receiving information leaflets, all patients considered them useful, even though information makes one third of patients more anxious (17). Anyway, the anxiety induced in patients with Crohn's disease by their accessing information through leaflet reading de-creases in the long run (18). Most probably, the best system to convey information to patients is by verbal means in a person-to-person encounter, and this information may then be completed or deepened by using other modalities. Which may be more effective is as yet not well esta-blished. When compared, the effectiveness of knowledge acquisition on colonoscopy and cancer risk in patients with ulcerative colitis is the same for leaflets and leaflets plus videos (19). Nevertheless, knowledge (information) communication should be supplemented by appropriate information use (education) in order to acquire healthy living habits (health promotion).
An increasingly important information source is the internet. A recent survey of 173 patients from Asociación Catalana de Enfermos de Crohn y Colitis (ACCU) revealed that 84% of patients would be interested in visiting a web page on inflammatory bowel disease, and that 44% of patients searched the internet for topics related to their disease (20). Such evidence suggests that patients with inflammatory bowel disease are prone to acquiring information and willing to resort to cutting-edge resources to do so.
To conclude, patients with inflammatory bowel disease view healthcare received in an overall satisfactory manner. However, deficiencies such as inadequate information, lack of family care, and poor accessibility to available healthcare resources were detected. The setting up of interactive monographic units and novel telematic technologies will make up an essential resource for the improvement of care to patients with inflammatory bowel disease.
REFERENCES
1. Casellas F, López Vivancos J, Badia X, Vilaseca J, Malagelada JR. Impact of surgery for Crohn's disease on health-related quality of life. Am J Gastroenterol 2000; 95: 177-82. [ Links ]
2. Hörnquist JO. Quality of life: concept and assessment. Scand J Soc Med 1989; 18: 68-79. [ Links ]
3. Vergara M, Casellas F, Badia X, Malagelada JR. Assessing the quality of life of household members of patients with inflammatory bowel disease: development and validation of a specific questionnaire. Am J Gastroenterol 2002; 97: 1429-37. [ Links ]
4. De Boer A, Sprangers M, Bartelsman J, de Haes H. Predictors of health care utilization in patients with inflammatory bowel disease: a longitudinal study. Eur J Gastroenterol Hepatol 1998; 10: 783-9. [ Links ]
5. Casellas F, López-Vivancos J, Casado A, Malagelada JR. Factors affecting health related quality of life of patients with inflammatory bowel disease. Qual Life Res 2002; 11: 775-81. [ Links ]
6. Van der Eijk I, Stockbrügger R, Russel M. Influence of quality of care on quality of life in inflammatory bowel disease: literature review and studies planned. Eur J Int Medicine 2000; 11: 228-34. [ Links ]
7. Satisfacció dels usuaris dels serveis i participació dels ciutadans. En: Pla de Salut de Catalunya, 1999-2001. Generalitat de Catalunya, Departament de Sanitat i Seguretat Social. Primera edició, 1999. p. 171. [ Links ]
8. Feagan BG, Vreeland MG, Larson LR, Bala MV. Anual cost of care for Crohn's disease: a payor perspective. Am J Gastroenterol 2000; 95: 1955-60. [ Links ]
9. Hay JW, Hay AR. Inflammatory bowel disease: cost-of-illness. J Clin Gastroenterol 1992; 14: 309-17. [ Links ]
10. Ekbom A, Blomqvist P. Costs to society in Crohn's disease. Res Clin Forums 1997; 20: 33-9. [ Links ]
11. Williams JG, Cheung WY, Russell IT, Cohen DR, Longo M, Lervy B. Open access follow up for inflammatory bowel disease: pragmatic randomised trial and cost effectiveness study. Br Med J 2000; 320: 544-8. [ Links ]
12. Robinson A, Thompson DG, Wilkin D, Roberts C. Guided self-management and patient-directed follow-up of ulcerative colitis: a randomised trial. Lancet 2001; 358: 976-81. [ Links ]
13. Miller L, Caton S, Lynch D. Telephone clinic improves quality of follow-up care for chronic bowel disease. Nurs Times 2002; 98: 36-8. [ Links ]
14. Moser G, Tillinger W, Sachs G. Disease-related worries and concerns: a study on out-patients with inflammatory bowel disease. Eur J Gastroenterol Hepatol 1995; 7: 853-8. [ Links ]
15. Olbrisch ME, Ziegler SW. Psychological adjustement to inflammatory bowel disease: informational control and private self-conciousness. J Chronic Dis 1982; 35: 573-80. [ Links ]
16. Borgaonkar MR, Townson G, Donnelly M, Irvine J. Providing disease-related information worsens health-related quality of life in inflammatory bowel disease. Inflam Bowel Dis 2002; 8: 264-9. [ Links ]
17. Connroy SP, Mayberry JF. patient information booklets for asian patients with ulcerative colitis. Public Health 2001; 115: 418-20. [ Links ]
18. Smart H, Mayberry J, Calcraft B, Morris JS, Rhodes J. Effect of information booklet on patients' anxiety levels and consultation rates in Crohn's disease. Public Health 1986; 100: 184-6. [ Links ]
19. Eaden J, Abrams k, Shears J, Mayberry J. Randomized controlled trial comparing the efficacy of a video and information leaflet versus information leaflet alone on patient knowledge about surveillance and cancer risk in ulcerative colitis. Inflam Bowel Dis 2002; 8: 407-12. [ Links ]
20. Panés J, Lacy AM, Sans M, Soriano A, Piqué JM. Elevado índice de consultas por internet de los pacientes catalanes con enfermedad inflamatoria intestinal. Gastroenterol Hepatol 2001; 25: 306-9. [ Links ]











 text in
text in