Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Nefrología (Madrid)
versión On-line ISSN 1989-2284versión impresa ISSN 0211-6995
Nefrología (Madr.) vol.34 no.3 Cantabria 2014
https://dx.doi.org/10.3265/Nefrologia.pre2014.Jan.12434
LETTERS TO THE EDITOR
IGM nephropathy presenting as full blown crescentic glomerulonephritis: first report in the literature
Dear Editor,
IgM nephropathy (IgMN) is a relatively newly described, and still contentious, clinicopathologic entity which presents mainly as idiopathic nephrotic syndrome (INS) in both children and adults. Although, it is widely acclaimed that this lesion was first described in 1978 by two groups led by Cohen et al.1 and Bhasin et al.,2 predominant IgM deposits in the glomeruli, in fact, were first described in renal biopsies in 1974 by Putte et al.3 in patients with persistent or recurrent hematuria. The frequency of IgMN reported in literature has varied from 2% to 18.5%.4-8 We have earlier reported a prevalence of IgMN of 18.5% in native renal biopsies in children presenting with INS in Pakistan.9 The disease is defined by its immunopathologic features: the light microscopic (LM) features being highly variable ranging from minimal change lesion to variable degrees of mesangial proliferation to focal segmental glomerulosclerosis (FSGS).4,5,9 A few studies have also noted small subcapsular crescents in cases of IgMN.4,5 However, up till now, no case of IgMN has been reported presenting with crescentic GN (CresGN). We herein report a case of an 11-year-old child presenting clinically with rapidly progressive glomerulonephritis (RPGN) and the biopsy features of CresGN.
Case report
An 11-year-old female presented with one month history of generalized body swelling, anorexia and moderate degree of hearing loss. On physical examination, her blood pressure was 150/110mmHg. No past medical history of note was elicited. Family history was unremarkable for renal disease. Abdominal ultrasound showed normal size kidneys. Urine examination revealed 1+ albumin, 15-20 white blood cells (WBCs)/HPF and 6-8 red blood cells (RBCs)/HPF. Her blood urea was 198mg/dL and serum creatinine, 4.5mg/dL. Relevant viral serology was negative. Slit-lamp examination for eye abnormalities was negative.
The percutaneous renal biopsy was done, which mostly comprised of medulla with little cortex containing six glomeruli. These showed diffuse severe degree of mesangial proliferation. In addition, three glomeruli showed extracapillary epithelial cell proliferation with the formation of cellular crescents (Figure 1). Mild arteriolosclerosis was seen. Mild degree of tubular atrophy and interstitial scarring was also noted. On immunoflourescence (IF), there was diffuse, bright (3+, on a scale of 0 to 3+) positivity of IgM in the mesangium and peripheral capillary loops, accompanied by C3 and C1q in similar location (Figure 2). IgG and IgA were negative. A diagnosis of IgMN was rendered and lupus serology and serum antineutrophil cytoplasmic antibodies (ANCAs) were advised, which returned negative.
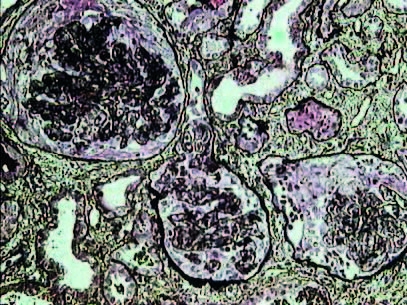
Figure 1. Medium-power view showing cellular
crescents in all the glomeruli (Silver stain, ×200).
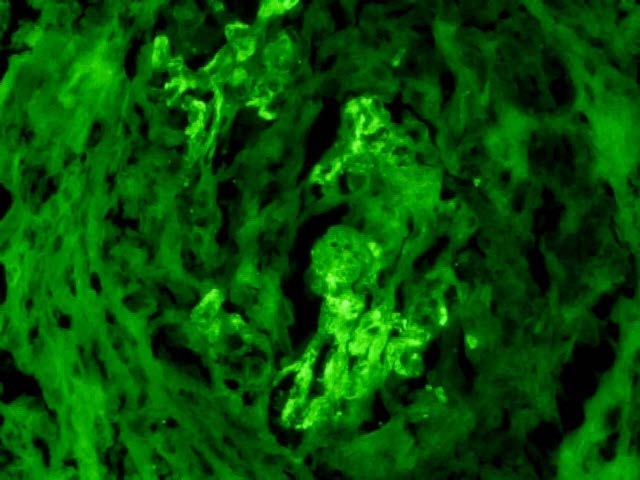
Figure 2. High-power view showing diffuse mesangial positivity of 3+ intensity of IgM in the collapsed tufts of the
glomerulus on immunoflourescence (IF) microscopy. The surrounding crescent is negative (anti-IgM on IF, ×400).
She was given three pulses of methylprednisolone and was started on oral steroids in the standard dosage. Her serum creatinine stabilized at 2.3mg/dL and she was discharged with advice to follow-up in the OPD. Unfortunately, she was soon last to follow-up.
Discussion
To our knowledge, this is the first case of IgMN in literature presenting with full-blown CresGN. The latter is a morphologic expression of severe glomerular injury resulting in rupture of glomerular basement membranes (GBMs) and leakage of fibrin and monocytes into the Bowman's capsule. This causes reactive proliferation of the visceral and parietal epithelial cells along with influx of macrophages, resulting in crescent formation. CresGN is further classified into three etiologic categories on the basis of IF microscopy: anti-GBM disease, immune complex-mediated, and pauci-immune. Our case belongs to the second category on the basis of IF study.
The morphological changes observed on LM in our case were rather deviant from the vast majority of cases of IgMN, which show either minor changes or mild mesangial proliferation.4-10 Moderate to severe degree of mesangial proliferation is rare in the reported literature.8,9 Some authors have also noted small cellular crescents in a number of biopsy specimens in IgMN.4,5 In contrast, our case showed prominent cellular crescent formation in half of the glomeruli, thus, fulfilling the criteria for the diagnosis of CresGN. Full blown CresGN has not been previously reported in IgMN in the literature.
This case illustrates the point that the spectrum of morphological changes in IgMN is wider than hitherto described in the literature. In this regard, it resembles closely IgAN, another well characterized immune complex-mediated disease, not only clinically but also morphologically, which shows the entire range of morphologic changes from minor glomerular changes to CresGN to chronic sclerosing GN.
The etiology and pathogenesis of IgMN are still unresolved. Some authors have suggested immune complex-mediated, classical pathway of complement activation leading to mesangial injury and reaction, evinced by the co-localization of C1q and C4 along with IgM in the glomerular mesangium.4,5 Others have found C1q only infrequently.8 Source of the triggering antigen is also debated.5
In summary, the present case expands the spectrum of morphologic presentation of IgMN and proves that this disease can rarely present as rapidly progressive renal failure.
Conflict of interest
The authors declare that there is no conflict of interest associated with this manuscript.
Javed Kazi, Muhammed Mubarak
Histopathology. Sindh Institute of Urology and Transplantation (SIUT).
Karachi, Sindh (Pakistan)
References
1. Cohen AH, Border WA, Glassock RJ. Nephrotic syndrome with glomerular mesangial IgM deposits. Lab Invest 1978;38:610-9. [ Links ]
2. Bhasin HK, Abeulo JG, Nayak R, Esparza AR. Mesangial proliferative glomerulonephritis. Lab Invest 1978;39:21-9. [ Links ]
3. Van de Putte LBA, DeLaRiviere GB, Van Breda Vriesman PJC. Recurrent or persistent hematuria, sign of mesangial immune-complex deposition. N Engl J Med 1974;290:1165-70. [ Links ]
4. Lawler W, Williams G, Tarpey P, Mallick NP. IgM associated primary diffuse mesangial proliferative glomerulonephritis. J Clin Pathol 1980;33:1029-38. [ Links ]
5. Hsu HC, Chen WY, Lin GJ, Chen L, Kao SL, Huang CC, et al. Clinical and immunopathologic study of mesangial IgM nephropathy: Report of 41 cases. Histopathology 1984;8:435-46. [ Links ]
6. Chan YH, Wong KM, Choi KS, Chak WL, Cheung CY. Clinical manifestation and progression of IgM mesangial nephropathy: a single center perspective. Hong Kong JNephrol 2000;2:23-6. [ Links ]
7. Kopolovic J, Shvil Y, Pomeranz A, Ron N, Rubinger D, Oren R. IgM nephropathy: morphological study related to clinical findings. Am J Nephrol 1987;7:275-80. [ Links ]
8. Myllymaki J, Saha H, Mustonen J, Helin H, Pasternack A. IgM nephropathy: clinical picture and long term prognosis. Am J Kidney Dis 2003;41:343-50. [ Links ]
9. Mubarak M, Kazi JI, Malik S, Lanewala A, Hashmi S. Clinicopathologic characteristics and steroid response of IgM nephropathy in children presenting with idiopathic nephrotic syndrome. APMIS 2011;119:180-6. [ Links ]
10. Al-Eisa A, Carner JE, Lirenman DS, Magil AB. Childhood IgM nephropathy: comparison with minimal change disease. Nephron 1996;72:37-43. [ Links ]
![]() Correspondence:
Correspondence:
Muhammed Mubarak,
Histopathology,
Sindh Institute of Urology and Transplantation (SIUT),
Dewan Faruque Medical Complex,
74200, Karachi,
Sindh, Pakistan
E-mail: drmubaraksiut@yahoo.com
E-mail: drmubaraksiut@gmail.com














