Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Nutrición Hospitalaria
versión On-line ISSN 1699-5198versión impresa ISSN 0212-1611
Nutr. Hosp. vol.34 no.4 Madrid jul./ago. 2017
https://dx.doi.org/10.20960/nh.657
TRABAJO ORIGINAL / Epidemiología y dietética
Hospital malnutrition screening at admission: malnutrition increases mortality and length of stay
Cribado de la desnutrición hospitalaria en la admisión: la desnutrición aumenta la mortalidad y la duración de la estancia hospitalaria
Elisabet Leiva Badosam1, María Badia Tahull1, Nuria Virgili Casas2, Gema Elguezabal Sangrador3, Concepción Faz Méndez1, Ignacio Herrero Meseguer4, Àngels Izquierdo González5, Rafael López Urdiales2, Francisco Javier de Oca Burguete6, María Tubau Molas1, Concepció Vilarasau Farré2 and Josep Manel Llop Talaveron1; on behalf of the Clinical Nutrition Committee
Departments of 1Pharmacy, 2Endocrinology and Nutrition, 3Anestesiology, 4Critical Care, 5Otorrinolaringology and 6General and Digestive Surgery. IDIBELL-Hospital Universitari Bellvitge. L'Hospitalet de Llobregat. Barcelona, Spain
ABSTRACT
Introduction: Malnutrition is common in patients admitted to hospital and is associated with morbidity and mortality. We conducted a study to assess the prevalence of nutritional risk, risk factors associated and its consequences in a third-level hospital.
Methods: This is a prospective nutritional screening study of hospitalized patients evaluated within the first 72 hours of admission, by Malnutrition Universal Screening Tool (MUST) and Short Nutritional Assessment Questionnaire (SNAQ) screening tests. The variables recorded included demographic, anthropometric, hospitalization and clinical data.
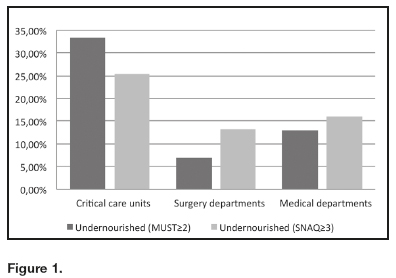
Results: Out of 409 patients, 12.7% and 15.3% were nutritionally at risk according to MUST and SNAQ, respectively, with the highest prevalence in critical care units (33.3%; 25.5%), amongst oncologic patients (17.5%; 28.4%) and those with higher Charlson comorbidity indices (CCI). Length of stay (LOS) was longer in patients at severe malnutrition risk (15.4 vs 9.9 days for MUST; 13.3 vs 9.9 days for SNAQ). Mortality was higher in those with high malnutrition risk (66.7% vs 10.9% for MUST; 50.0% vs 14.2% for SNAQ). Multivariate analysis showed that malnutrition was associated with CCI and mortality. Risk factors associated with LOS were admission as emergencies for both MUST and SNAQ tests.
Conclusions: The prevalence of malnutrition is high in patients on admission to a third-level hospital, with a higher prevalence in critical care units, amongst oncologic patients and those with a higher CCI. Malnutrition is associated with longer LOS and higher mortality. The systematic clinical use of screening tools enables to detect patients at risk of malnutrition and take appropriate action.
Key words: Malnutrition. Nutritional assessment. Nutrition surveys.
RESUMEN
Introducción: la desnutrición es común en los pacientes ingresados en el hospital y se asocia a morbi/mortalidad. El objetivo de este estudio es evaluar la prevalencia de riesgo nutricional, factores de riesgo asociados y sus consecuencias en un hospital de tercer nivel.
Métodos: estudio prospectivo de cribado nutricional de pacientes hospitalizados evaluados dentro de las primeras 72 horas de ingreso, mediante las herramientas Malnutrition Universal Screening Tool (MUST) y Short Nutritional Assessment Questionnaire (SNAQ). Las variables registradas incluyen datos demográficos, antropométricos, de hospitalización y clínicos.
Resultados: de los 409 pacientes entrevistados, 12,7% y 15,3% presentaban riesgo nutricional según MUST y SNAQ, respectivamente, con una mayor prevalencia en la Unidad de Cuidados Intensivos (UCI) (33,3%; 25,5%), pacientes oncológicos (17,5%; 28,4%) y aquellos con mayor índice de comorbilidad de Charlson (ICC). La estancia hospitalaria fue mayor en pacientes en riesgo de desnutrición severa (15,4 vs. 9,9 días para MUST; 13,3 vs. 9,9 días para SNAQ), así como la mortalidad (66,7% vs. 10,9% para MUST; 50,0% vs. 14,2% para SNAQ). El análisis multivariante mostró una asociación entre desnutrición e ICC y mortalidad. Los factores de riesgo asociados con estancia hospitalaria fueron ingreso por urgencias para ambos tests.
Conclusiones: la prevalencia de desnutrición en pacientes al ingreso a un hospital de tercer nivel es alta, siendo mayor en las UCI, entre pacientes oncológicos y con mayor ICC. La desnutrición se asocia con mayor estancia hospitalaria y mayor mortalidad. El uso clínico sistemático de herramientas de detección puede ayudar a identificar pacientes en riesgo de desnutrición y tomar las medidas apropiadas.
Palabras clave: Desnutrición. Valoración nutricional. Cribado nutricional.
Introduction
Disease-related malnutrition is a major problem in health care settings in developed countries. Malnutrition is an independent risk factor for delayed recovery, mortality and morbidity, such as wound healing, complication rates, hospitalization, health care costs, and an early re-admission rate (1-7). Therefore, early recognition and treatment are important for both patients and health care systems. Nutritional intervention for malnourished patients is a cost-effective strategy for improving the quality of hospital care (3,4,6,7).
There are many reasons that can lead to hospital malnutrition, among them the disease itself, little knowledge of patients' nutritional status by the healthcare staff, certain diagnostic or therapeutic procedures, and the lack of standardized protocols to avoid periods of fasting and identify patients at risk of malnutrition.
Malnutrition in acute care patients has been associated with age, apathy/depression, diseases such as cancer, diabetes, cardiac or gastrointestinal conditions, inability to chew or swallow, limited mobility, sensory loss (taste, smell), treatment (ventilation, surgery, drain tubes) or drug therapy (8).
The prevalence of malnutrition in hospitals is high and ranges from 10% to 60%, depending on the definition used, the type of patient and the method of assessment (1,2,9-22). Against this background, on 11th June 2009, the European Society for Clinical Nutrition and Metabolism (ESPEN), the European Nutrition for Health Alliance (ENHA), the Medical Nutrition International Industries (MNI) and the members and partners of these organizations joined forces to fight malnutrition in Europe and signed the Prague Declaration. They concluded that malnutrition, including disease-related malnutrition, is an urgent public health problem and action needs to be taken to prevent it (23). These actions were implemented as a key priority in the 2008-2013 EU Health Strategy (24). For these reasons, this study was carried out using a multidisciplinary approach with only the usual clinical tools in order to implement feasible and easy systematic screening as part of the clinical evaluation of patients on admission to hospital.
The main objective of the study was to assess the risk of malnutrition in patients recently admitted to a third-level hospital. Secondary objectives were to estimate the associations between risk of malnutrition and comorbidities, length of stay (LOS) and mortality.
Methods
DESIGN AND SUBJECTS
This is a three-month prospective nutritional screening study of hospitalized patients evaluated at admission in a third-level hospital with 651 beds.
The following patients were included:
- Those admitted to the hospital within the previous 72 hours.
- Those > 18 years old.
- Those who gave verbal informed consent to participate in the study. For those patients who were not able to give informed consent themselves, it was asked of a relative.
Exclusion criteria were:
- Patients admitted from another hospital.
- Patients admitted for ambulatory surgery.
- Patients who refused to participate in the data collection.
When a patient was excluded, another one was selected.
In order to improve the representativeness of the sample, an alpha risk of 0.05 was accepted with an accuracy of ± 0.03 units in a bilateral contrast and a malnutrition ratio estimated as 28.9%, according to previous data published (20), and a sample of 409 subjects was calculated, assuming that the population is 651 individuals. In order to have a representative sample of the different clinical departments, a list of the number of patients to be recruited from each department was provided, including all the specialties, except for pediatrics and obstetrics, which are not present at our hospital.
VARIABLES
Study variables recorded included:
- Demographic data: age, sex, country of origin.
- Anthropometric data: weight, height and body mass index (BMI), calculated from the recorded weight and height.
- Hospitalization data: reason for admission, department of admission, whether the patient had cancer or not, admission status (scheduled or emergency; medical, surgical or critical), surgical intervention during the admission, length of stay (LOS), discharge destination (home, nursing home, another healthcare center) and exitus.
- Medical history: the Charlson comorbidity index (CCI) was used to categorize comorbidities of patients
- Nutritional screening tools: the nutrition evaluation was carried out with two different validated clinical screening tools, the Malnutrition Universal Screening Tool (MUST) (25) and the Short Nutritional Assessment Questionnaire (SNAQ) (26), since they are quick, easy and have a general character of screening for all hospital wards. MUST classifies patients as: low risk of malnutrition (0 points), requiring routine clinical care; medium risk of malnutrition (1 point), requiring observation; and high risk of malnutrition (≥ 2 points), requiring treatment from the nutritional support team. SNAQ classifies patients as: no malnutrition (≤ 1 point), requiring no intervention; moderately malnourished (2 points), requiring nutritional intervention; and severely malnourished (≥ 3 points), requiring nutritional intervention and treatment.
All members of the Clinical Nutrition Committee participated in the collection of data as well as in the interviews. Answers were obtained by asking the patient or, if this was not possible, by consulting a relative or patient documentation.
Ethical approval for the present study was provided by the Clinical Research Ethics Committee (CREC). Data were collected in accordance with the ethical standards of the Ethics Committee.
STATISTICAL ANALYSIS
Data were analyzed using the statistical package SPSS version 19. p values < 0.05 were considered as significant.
For univariate and multivariate analyses, MUST and SNAQ were dichotomized considering as undernourished those with MUST ≥ 2 or SNAQ ≥ 3.
All categorical variables were reported as frequency and percentage, while the continuous variables were reported as mean ± standard deviation.
Statistical differences were tested by univariate analysis using Chi-squared tests and the Mann-Whitney test for the continuous date since they had not normally distribution.
Three multivariate models were carried out:
- Two stepwise logistic regression analyses with the outcome nutritional risk as a dependent variable, according to SNAQ or MUST, and oncologic patients and CCI as independent variables.
- Two stepwise logistic regression analyses with mortality as a dependent variable and oncologic patients, CCI, age and nutritional risk, evaluated according to SNAQ or MUST dichotomized tests, as independent variables.
- Two stepwise linear regression models with LOS as a dependent variable and oncologic patients, admission as emergencies, surgery admission and nutritional risk, evaluated according to MUST or SNAQ, as independent variables.
Results
During the study period (March to June 2013), a total of 409 patients were included; 42.8% were women, with a mean age of 61.8 ± 16.9 years, and 48.4% of the patients included were ≥ 65 years old. The majority of participants were Caucasian (96.3%).
The mean weight of the patients was 73.9 ± 17.9 kg, the mean height was 164.1 ± 9.4 cm and the BMI, 27.5 ± 5.8, kg/m2. BMI was < 18.5 kg/m2 in 7% of patients, and between 18.5 kg/cm2 and 20 kg/m2 in 3.5% of the patients.
Table I depicts admission and hospitalization-related characteristics of the participants. The mean value of the CCI was 2.9 ± 2.3. The more prevalent comorbidities were hypertension (53.3%), coronary disease (16.1%), diabetes mellitus without chronic complications (16.9%) and non-metastatic solid tumors (16.6%).
The overall rate of patients at risk of malnutrition was between 12.7% and 15.3%, for MUST and SNAQ respectively. Table II and figure 1 show that critically ill patients were those with a higher risk of malnutrition, while patients admitted to surgical and medical departments had similar rates of malnutrition risk (Fig. 1). Admission status (scheduled vs emergencies) was not associated with the risk of malnutrition. Those patients with a surgical intervention during admission had lower risk of malnutrition for MUST than the non-surgical ones. Malnourished patients had more comorbidities, longer LOS (5.5 days for MUST; 3.4 days for SNAQ) and higher mortality rates.
Using multivariate analysis to determine the risk factors associated with malnutrition, we found CCI was the only associated variable when using MUST, and oncologic patients and comorbidities when using SNAQ (Table III).
Table IV shows a significant association between the malnutrition risk according to both MUST and SNAQ and mortality.
We also found malnutrition risk, both for admission as an emergency and for interventional surgery during admission, as a risk factor for longer LOS (Table V).
Discussion
PREVALENCE OF MALNUTRITION
Although the sample is representative of our population, the proportions of malnutrition prevalence found with each tool are lower compared to the last study in Catalonian hospitals published in 2012 (20) (12.7% for MUST and 15.3% for SNAQ vs 28.9% for Nutritional Risk Screening [NRS-2002]). However, there are generally wide ranges of prevalence published in European, Australian and US studies (1,3,9-22). There are many reasons for this wide range, including different medical and geographical settings, different patient populations and non-uniform criteria for the use of a screening tool for malnutrition. In the previous study developed in Catalonia, the NRS-2002, which is recommended by the European Society for Clinical Nutrition and Metabolism (ESPEN) (27), was used, while in the present study we selected MUST and SNAQ as nutritional screening tests. Both MUST and SNAQ are currently validated, practical and easy to use screening tools, and we choose both tests because there were few studies testing them, especially the SNAQ. In fact, a recent published study determines the prevalence of malnutrition in a big sample of patients hospitalized in a Dutch hospital with MUST and SNAQ (27).
The systematic review of Van Bokhorst-de van der Schueren evaluated 83 studies, including 32 different screening tools, and concluded that none of them performed consistently well on either screening/assessing patients' nutritional status or predicting nutrition related outcomes. For the adult hospital population, only MUST showed fair to good criterion or construct validity to different reference methods, while SGA, NRS-2002 and MUST all showed fair to good predictive validity to predict LOS, mortality or complications (28).
In our study, we have examined the risk factors and the consequences of hospital malnutrition in patients evaluated within 72 hours post-hospital admission, since previous studies show that early nutritional intervention improved health outcomes, morbidity, mortality, and reduced LOS in hospitalized patients (26,29,30).
Studies that evaluate malnutrition on admission show variable rates of malnutrition. A study of 750 patients from three hospitals in Denmark showed that 22% of the patients were nutritionally at-risk on admission, as assessed by the NRS-2002 (11). In a study of 15 randomly selected departments in Danish hospitals, out of 590 patients, 39.9% were nutritionally at risk, with the highest prevalence in departments of gastro-surgery (57%) (14). In 2008, a multinational study comprising 12 countries in Europe and the Middle East evaluated malnutrition risk according to NRS-2002. Of the 5.051 study patients, 32.6% were defined as "at-risk". However, the percentage at risk ranged from 13% to 100%, representing the heterogeneity of patient populations from different countries and departments (18). In contrast, another study in 34 Turkish hospitals of 29,139 patients found 15% of them at nutritional risk on admission. Nutritional risk was highest (52%) in Intensive Care Unit patients and lowest (3.9%) in otorhinolaryngology patients (9). A recent study conducted in 13 Dutch hospitals reported that 13.7% (n = 419.086) and 14.9% (n = 144.977) of the patients were defined as being undernourished according to SNAQ and MUST (22). These results are similar to ours.
RISK FACTORS ASSOCIATED WITH MALNUTRITION
Admission and surgery
In our study, critical patients were those at a higher risk of malnutrition. Korfali G et al., in their study conducted in Turkish hospitals, also found the highest prevalence of nutritional risk in the ICU (52%) (9). Agarwal et al. found similar malnutrition risk at admission among surgical (43%) and medical (51%) patients in a population of 3,122 evaluated patients (16). However, a previous finding in Spanish hospitals showed a higher prevalence of malnutrition risk in medical treatment units of hospitals (39%), compared to surgical units (16%) (20). It should be noted that these published malnutrition risk rates are higher than ours, except for those published by Pirlich et al., where patients admitted to surgical wards had a rather low risk of malnutrition at 13.6% (13). Different instruments used for the classification of malnutrition as well as different disease spectra most likely explain these discrepancies. In fact, Naber et al. found that, depending on the tool used for diagnosis, between 40% and 62% of the patients studied were classified as malnourished (21).
When considering the relationship between the type of hospital admission and the risk of malnutrition, we have found no difference between the patients admitted through the emergency route and those admitted for scheduled treatment. Our results also differ from previous studies that showed an increased risk of malnutrition when patients were admitted via the emergency route (16,20,31). These differences are probably due to the fact that we are in the setting of a third level hospital where most of the patients admitted have severe pathologies.
In our study, patients experiencing a surgical intervention during admission had a rather lower risk of malnutrition than non-surgical ones. In contrast, other publications have described a much higher rate of malnutrition (14,32). These results are biased by the comorbidity of the included patients; the patients in whom surgery was performed during admission had lower comorbidities (CCI = 2.47) than the non-surgical ones (CCI = 3.44).
Morbidity
Malnutrition is, in general, a consequence of several risk factors, of which the disease per se is one of the most important, where increased energy and protein requirements, increased losses together with inflammation may play a central role. In fact, the interaction of disease and nutrition is bilateral: while disease may cause secondary malnutrition, malnutrition may adversely influence the underlying disease. So, this makes it difficult to conclude that malnutrition alone leads to the patient's worse outcome (33). However, there are many studies that report the association of morbidity with malnutrition (1,3,13,15). Our findings support this association. Malnourished patients had significantly higher values of CCI than those who were well nourished, using both the univariate and multivariate analysis. In fact, in the logistic model, CCI was the only variable associated with both screening tests, reporting an increased risk of mortality for moderate to severe risk of malnutrition patients compared to those of low risk.
Oncologic patients
In some cancers, the proteolysis inducing factor (PIF) and lipid mobilizing factor (LMF) have been shown to play a major role in the pathogenesis of the cachexia syndrome (1). Besides, drug-related side effects such as chemotherapy, morphine derivates or sedatives can cause anorexia or affect the ingestion of food. In fact, oncology patients are 1.7 times more likely to be malnourished than other hospitalized patients (34). A recent study conducted in 2,248 cancer patients from 20 Chinese hospitals found 19.7% of patients were undernourished at baseline. Patients with gastrointestinal malignancies had higher rates of undernutrition than other patients (35).
Our results partially support these studies, since oncologic patients had significantly higher risk of malnutrition than the non-oncologic ones only for SNAQ. However, our malnutrition risk at baseline in oncologic patients is higher than that published by Pan H et al., probably due to the different screening test used and the high variability of evaluated patients (35). In our multivariate model, oncologic patients had 2.117-fold risk of being malnourished than non-oncologic ones, according to SNAQ.
The prevalence of malnutrition screening was different depending on the test used. Although these two screening instruments have been proven to have a sufficient diagnostic accuracy and are both valid, they categorize differently: while SNAQ scores weight loss, appetite, and use of enteral nutrition, MUST scores BMI, weight loss, and acute disease effect on intake. Oncology hospital patients often use enteral nutrition and have a decreased appetite. Since both risk factors for malnutrition are included in the SNAQ but not in the MUST, the SNAQ is more sensitive for detecting malnutrition in this patient population. Furthermore, the screening took place at admission, and particularly in this patient group, much attention is given to an optimal preoperative nutritional status. Hence, no nutritional intake for five days, a criterion of the MUST, would be a rare exception, so the MUST score is less likely to increase.
CONSEQUENCES OF MALNUTRITION
Lenght of stay
The negative impact of malnutrition on patient's outcome is well demonstrated. Many studies have found that LOS is significantly longer in malnourished patients, with an increase of 40-70% in malnourished patients (1,3,13). According to these studies, in our cohort the LOS of malnourished screened patients was 5.5 days longer than for well nourished patients when evaluated by MUST.
While Pirlich et al. used number of prescriptions per day as a surrogate marker for disease severity (13), other authors found malnutrition as an independent risk factor for longer LOS, not controlled by disease severity (3,5). Since we do not have collected the disease severity we cannot support these results. However, as indicated in table V, malnutrition and being admitted as emergencies are risk factors of an increased LOS. In fact, it has been demonstrated that providing strong nutritional care can reduce LOS. In a recent retrospective analysis of Premier Healthcare Alliance data that included more than one million adult inpatient cases, representing approximately 20% of all inpatient admissions in the United States, oral nutritional supplementation reduced LOS by an average of 2.3 days or 21% and the average cost saving was 21.6% compared with routine care (36).
Mortality
Malnutrition has been shown to increase mortality not only in chronic disease, but also in acute settings (1). According to the Australasian Nutrition Care Day Survey (ANCDS) in 56 Australian and New Zealand acute care hospitals, of 3,122 patients, 32% were malnourished and 23% consumed ≤ 25% of the offered food. The odds of 90-day in-hospital mortality were twice greater for malnourished patients and those consuming ≤ 25% of the offered food (16).
In our sample, in the multivariate model we found a strong association between mortality and malnutrition risk for both screening tools used. Patients at severe/moderate risk of malnutrition had an OR of 6.965 and 5.279 of mortality than those at low risk, according to MUST and SNAQ, respectively.
LIMITATIONS OF THE STUDY
The difficulty in interviewing patients with communication problems for various reasons, but who were probably at a higher risk of malnutrition, could have contributed to their exclusion, resulting in a certain selection bias.
We only have provided in-hospital mortality data and those that may have occurred in early post-discharge in a different setting were not recorded, hence mortality rate may have been underreported.
Besides, the selection of an objective screening tool leading to an easy comparison with other studies remains as a pending issue in the field of nutritional screening.
Conclusions
In conclusion, prevalence of third-level hospital malnutrition at admission is around 20% using MUST and SNAQ. Malignant diseases, major comorbidity and critical states were found to be the main contributors to disease-related malnutrition. So, in these populations the evaluation of nutritional status must be accurate in order to optimize their clinical outcome. For this reason, hospital protocol should include early nutritional assessment as part of every medical examination at admission.
References
1. Norman K, Pichard C, Lochs H, Pirlich M. Prognostic impact of disease-related malnutrition. Clin Nutr 2008;27(1):5-15. [ Links ]
2. Naber TH, Schermer T, De Bree A, Nusteling K, Eggink L, Kruimel JW, et al. Prevalence of malnutrition in nonsurgical hospitalized patients and its association with disease complications. Am J Clin Nutr 1997;66(5):1232-9. [ Links ]
3. Correia MI, Waitzberg DL. The impact of malnutrition on morbidity, mortality, length of hospital stay and costs evaluated through a multivariate model analysis. Clin Nutr 2003;22(3):235-9. [ Links ]
4. Pérez de la Cruz A, Lobo Támer G, Orduña Espinosa R, Mellado Pastor C, Aguayo de Hoyos E, Ruiz López MD. Malnutrition in hospitalized patients: Prevalence and economic impact. Med Clin (Barc) 2004;123(6):201-6. [ Links ]
5. Agarwal E, Ferguson M, Banks M, Batterham M, Bauer J, Capra S, et al. Nutrition care practises in hospital wards: Results from the Nutrition Care Day Survey 2010. Clin Nutr 2012;31(6):995-1001. [ Links ]
6. Amaral TF, Matos LC, Tavares MM, Subtil A, Martins R, Nazaré M, et al. The economic impact of disease-related malnutrition at hospital admission. Clin Nutr 2007;26(6):778-84. [ Links ]
7. Löser C. Malnutrition in hospital: The clinical and economic implications. Dtsch Arztebl Int 2010;107(51-52):911-7. [ Links ]
8. Kubrack C, Jensen L. Malnutrition in acute care patients. Int J Nurs Stud 2007;44:1036-54. [ Links ]
9. Korfalii G, Gündogdu H, Aydintg S, Bahar M, Besler T, Moral AR, et al. Nutritional risk of hospitalized patients in Turkey. Clin Nutr 2009;28:533-7. [ Links ]
10. Edington J, Boorman J, Durrant ER, Perkins A, Giffin CV, James R, et al. The Malnutrition Prevalence Group. Prevalence of malnutrition on admission to four hospitals in England. Clin Nutr 2000;19:191-5. [ Links ]
11. Kondrup J, Johansen N, Plum LM, Bak L, Larsen IH, Martinsen A, et al. Incidence of nutritional risk and causes of inadequate nutritional care in hospitals. Clin Nutr 2002;21(6):461-8. [ Links ]
12. Meijers JM, Schols JM, Van Bokhorst-de van der Shueren MA, Dassen T, Janseen MA, Halfens RJ. Malnutrition prevalence in The Netherlands: Results of the annual Dutch national prevalence measurement of care problems. Br J Nutr 2009;101(3):417-23. [ Links ]
13. Pirlich M, Schütz T, Norman K, Gastell S, Lübke HJ, Bischoff SC, et al. The German hospital malnutrition study. Clin Nutr 2006;25(4):563-72. [ Links ]
14. Rasmussen HH, Kondrup J, Staun M, Ladefoged K, Kristensen H, Wengler A. Prevalence of patients at nutritional risk in Danish hospitals. Clin Nutr 2004;23(5):1009-15. [ Links ]
15. Tannen A, Lohrmann C. Malnutrition in Austrian hospital patients. Prevalence, risk factors, nursing interventions, and quality indicators: A descriptive multicentre study. J Adv Nurs 2013;69(8):1840-9. [ Links ]
16. Agarwal E, Ferguson M, Banks M, Batterham M, Bauer J, Capra S, et al. Malnutrition and poor food intake are associated with prolonged hospital stay, frequent readmissions, and greater in-hospital mortality: Results from the Nutrition Care Day Survey 2010. Clin Nutr 2013;32(5):737-45. [ Links ]
17. Álvarez-Hernández J, Planas Vila M, León-Sanz M, García de Lorenzo A, Celaya-Pérez S, García-Lorda P, et al.; PREDyCES researchers. Prevalence and costs of malnutrition in hospitalized patients: The PREDyCES Study. Nutr Hosp 2012;27(4):1049-59. [ Links ]
18. Sorensen J, Kondrup J, Prokopowicz J, Schiesser M, Krähenbühl L, Meier R, et al. EuroOOPS study group. EuroOOPS: An international, multicentre study to implement nutritional risk screening and evaluate clinical outcome. Clin Nutr 2008;27(3):340-9. [ Links ]
19. McWhirter JP, Pennington CR. Incidence and recognition of malnutrition in hospital. BMJ 1994;308(6934):945-8. [ Links ]
20. Burgos R, Sarto B, Elío I, Planas M, Forga M, Cantón A, et al.; on behalf of the Group for the Study of Malnutrition in Hospitals in Catalonia. Prevalence of malnutrition and its etiological factors in hospitals. Nutr Hosp 2012;27(2):469-76. [ Links ]
21. Naber TH, Schermer T, De Bree A, Nusteling K, Eggink L, Kruimel JW, et al. Prevalence of malnutrition in nonsurgical hospitalized patients and its association with disease complications. Am J Clin Nutr 1997;66(5):1232-9. [ Links ]
22. Kruizenga H, Van Keeken S, Weijs P, Bastiaanse L, Beijer S, Huisman-de Waal G, et al. Undernutrition screening survey in 564,063 patients: Patients with a positive undernutrition screening score stay in hospital 1.4 d longer. Am J Clin Nutr 2016;103(4):1026-32. [ Links ]
23. The Prague Declaration: Stop disease-related malnutrition. Accessed on Sept 4th 2013. Available at: http://www.european-nutrition.org/index.php/topics/praguedeclaration. [ Links ]
24. Commission of the European Communities. Together for health: A strategic approach for the EU 2008-2013, 2010. Accessed on Sept 4th 2013. Available at: http://www.european-nutrition.org/index.php/topics/together_for_health_strategy_2008_2013. [ Links ]
25. Malnutrition Advisory Group (MAG) of the British Association for Parenteral and Enteral Nutrition. The "MUST" explanatory booklet. A guide to the "Malnutrition Universal Screening Tool" for adults. Edited on behalf of MAG by Todorovic V, Russell C, Stratton R, Ward J and Elia M. November 2003. [ Links ]
26. Kruizenga HM, Seidell JC, De Vet HC, Wierdsma NJ, Van Bokhorst-de van der Schueren MA. Development and validation of a hospital screening tool for malnutrition: The short nutritional assessment questionnaire (SNAQ). Clin Nutr 2005;24(1):75-82. [ Links ]
27. Kondrup J, Allison SP, Elia M, Vellas B, Plauth M. ESPEN Guidelines for Nutrition Screening 2002. Clin Nutr 2003;22(4):415-21. [ Links ]
28. Van Bokhorst-de van der Schueren MA, Guaitoli PR, Jansma EP, De Vet HC. Nutrition screening tools: Does one size fit all? A systematic review of screening tools for the hospital setting. Clin Nutr 2014;33(1):39-58. [ Links ]
29. Tappenden KA, Quatrara B, Parkhurst ML, Malone AM, Fanjiang G, Ziegler TR. Critical role of nutrition in improvising quality of care: An interdisciplinary call to action to address adult hospital malnutrition. Medsurg Nursing 2013;22:147-65. [ Links ]
30. Somanchi M, Tao X, Mullin G.E. The facilitated early enteral and dietary management effectiveness trial in hospitalized patients with malnutrition. JPEN 2011;35(2):209-16. [ Links ]
31. Planas M, Audivert S, Pérez-Portabella C, Burgos R, Puiggrós C, Casanelles JM, et al. Nutritional status among adult patients admitted to a university-affiliated hospital in Spain at the time of genoma. Clin Nutr 2004;23(5):1016-24. [ Links ]
32. Bruun LI, Bodaeus I, Bergstad I, Nygaard K. Prevalence of malnutrition in surgical patients: Evaluation of nutritional support and documentation. Clin Nutr 1999;18:141-7. [ Links ]
33. Jeejeebhoy KN. Nutritional assessment. Nutrition 2000;16:585-9. [ Links ]
34. Boltong AG, Loeliger JM, Steer BL. Using a public hospital funding model to strengthen a case for improved nutritional care in a cancer setting. Aut Health Rev 2013;37(3):286-90. [ Links ]
35. Pan H, Cai S, Ji J Jiang Z, Liang H, Lin F, Liu X. The impact of nutritional status, nutritional risk, and nutritional treatment on clinical outcome of 2248 hospitalized cancer patients: A multi-center, prospective cohort study in Chinese teaching hospitals. Nutr Cancer 2013;65(1):62-70. [ Links ]
36. Philipson T, Thornton Sinder J, Lakdawalla D, Stryckman B, Goldman D. Impact of oral nutritional supplementation on hospital outcomes. Am J Managed Care 2013;19(2):121-8. [ Links ]
![]() Correspondence:
Correspondence:
Elisabet Leiva Badosa.
Department of Pharmacy.
IDIBELL-Hospital Universitari Bellvitge.
C/ Feixa Llarga, s/n.
08907 L'Hospitalet de Llobregat, Barcelona. Spain.
e-mail: eleiva@bellvitgehospital.cat
Received: 13/10/2016
Accepted: 15/01/2017