INTRODUCTION
Cleft lip and palate are a type of congenital craniofacial dysplasia caused by a lack of union of the processes contributing to the formation of the upper lip and palate (1). Their incidence is one per 700-750 newborns and, in addition to the stigmatizing esthetic defect, they are associated to feeding and breathing problems, ear infections and hearing loss, speech pathology, and dental and developmental problems of the jaws (2,3). There are several classifications but, overall, the cleft may affect the lip, the palate, or both, and they can be unilateral or bilateral (4). Several environmental and genetic factors play a role in their etiology (5,6). The management of the cleft lip and palate requires a multidisciplinary treatment (surgical, orthopedic, orthodontic, otorhinolaryngological, phoniatric, and psychological) that must be done early in life to avoid functional alterations and allow normal infant and child development, although it may require treatment during adolescence and even later (7-9).
Patients with unilateral or bilateral complete cleft lip, as well as cleft palate, will have feeding difficulties because the cleft lip may compromise suction during lactation, and the cleft palate may cause milk to pass into the nasal cavity (10,11). Therefore, several recommendations to feed these infants should be taken into account, such as evaluating sucking capacity, teaching the appropriate position for breastfeeding, an adaptive feeding equipment (specific bottles and teats), and family education on child nutrition (12-14).
Nutritional status, growth and/or development may be affected in infants with cleft lip/palate due to feeding difficulties, their anatomy and surgical procedures, and airway and middle ear infections (15-18). Consequently, they often present growth impairment during infancy, more or less marked depending on the type of cleft, followed by subsequent compensatory catch-up growth in the first two years of life (19-21). The risk of undernutrition is even higher in developing countries where there are already poor nutritional conditions (22-24).
Growth restriction due to early life malnutrition maintained over time may decrease the potential for later growth, programming the child towards thinness, low final height, and low muscle mass (25). On the other hand, early malnutrition followed by rapid catch-up growth has been shown to program excessive fat mass accretion and a higher risk of long-term adiposity (25,26). The available studies on growth and long-term nutritional status of children with cleft lip and palate are scarce in the literature and, from two years of age, despite the fact that nutritional prognosis seems to improve (21,24,27), there is not enough evidence about the growth patterns and body composition of children with different types of CLP.
So, larger analyses are needed to assess long-term growth in these children, and the potential consequences for their body composition, either by default or by excess. This systematic review aims to identify the existing literature on the nutritional prognosis during childhood of patients undergoing surgery for cleft lip/palate, their body composition and growth patterns from two years of life, and, on the other hand, the possible effects of their early nutritional status on the long-term onset of overweight.
METHODS
DATA SOURCES AND SEARCH STRATEGY
The present systematic review was registered in the PROSPERO database and followed the systematic review methodology proposed in the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) (28) statement. A specific question was constructed according to the PICo (Population, phenomenon of Interest; Context) principle (29) (Table I). Population: children between 2 and 10 years of age, both sexes; phenomenon of interest: cleft lip and/or palate; context: growth and nutritional status (weight, height, BMI).
The studies were identified by searching in the PubMed and Scopus databases. In order to find all published studies, three command groups (according to keywords) were used. The search period was 2000-2020 and filters of English and Spanish languages were applied for all searches. First, the study population groups were combined as follows: patient OR patients OR infant OR infants OR infancy OR children OR child OR childhood OR toddler OR “early childhood” OR preschool OR pre-school OR “primary school” OR “elementary school”; the second group was related to the types of cleft: “cleft lip” OR “cleft palate” OR “cleft lip and palate” OR “cleft lip/palate” OR “cleft lip and/or palate” OR “lip and palate cleft” OR “lip and palate clefts”. Finally, the third group involved everything related to growth and nutrition and was combined as follows: growth OR body-weight OR “body weight” OR height OR length OR “body mass index” OR “body composition” OR “body fat” OR “fat mass” OR nutrition OR “nutritional status” OR anthropometry OR undernutrition OR malnutrition OR obesity OR overweight. The three terms were combined with the Boolean operator “AND”. Moreover, we added another group with the Boolean operator “NOT” to exclude from our search, which was related to facial growth: “maxillary growth” OR “maxillofacial growth” OR “craniomaxillofacial growth” OR “facial growth” OR “facial anthropometry” OR “facial anthropometric” OR “craniofacial cephalometric”. The results of the searches are summarized in Figure 1.
INCLUSION CRITERIA
- Type of study: longitudinal cohort studies and cross-sectional observational studies about growth and nutritional status.
- Type of participants: children between 2 and 10 years of age, both sexes, with any type of cleft lip, cleft palate, or cleft lip and palate.
- Type of outcome measured: growth, body-weight, height, length, body mass index, and body composition.
SEARCH SUMMARY
Two independent researchers identified 3,787 potentially relevant articles (RG and GR). After eliminating all duplicates (804), 2,983 manuscripts were evaluated. Based on the review of titles and abstracts, 17 relevant papers were kept for final revision. From those, 4 studies did not meet the criteria for age range (23,30-32), 4 additional studies did not report outcome measures (18,24,33,34), and 3 were excluded due to the type of study (one was an intervention study (14), 1 was a review (21), and another one was a letter without relevant results (35)). Consequently, the final number of relevant articles included was 6 (Fig. 1).
QUALITY ASSESSMENT
The Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies provided by the National Heart, Lung, and Blood Institute was used to assess the quality of the included studies (36). Two reviewers independently assessed and thereafter discussed the quality of the studies (RG and GR). In case of discrepancy a third author (II) was set aside for further evaluation. This is shown in table II.
Table II. Quality assessment of the included studies using the Observational Cohortand Cross-Sectional Studies (NHBLI) tool (36)

CD: cannot determine; NA: not applicable; NR: not reported; NHBLI: National Heart, Blood and Lung Institute. a1) Was the research question or objective in this paperclearly stated? 2) Was the study population clearly specified and defined? 3) Was the participation rate of eligible persons at least 50 %? 4) Were all the subjects selected or recruited from the same or similar populations? Were inclusion and exclusion criteria for being in the study prespecified and applied uniformly to all participants? 5) Was a sample size justification, power description or variance and effect estimates provided? 6) For the analyses in this paper, were the exposure(s) of interest measured prior to the outcome(s) being measured? 7) Was the timeframe sufficient so that one could reasonably expect to see an association between exposure and outcome if it existed? 8) For exposures that can vary in amount or level. did the study examine different levels of the exposure as related to the outcome (e.g., categories of exposure or exposure measured as continuous variable)? 9) Were the exposure measures (independent variables) clearly defined, valid, reliable, and implemented consistently across all study participants? 10) Was the exposure(s) assessed more than once over time? 11) Were the outcome measures (dependent variables) clearly defined, valid, reliable, and implemented consistently across all study participants? 12) Were the outcome assessors blinded to the exposure status of participants? 13) Was loss to follow-up after baseline 20 % or less? 14) Were key potential confounding variables measured and adjusted statistically for their impact on the relationship between exposure(s) and outcome(s)?
RESULTS
DESCRIPTION OF THE INCLUDED STUDIES
Of the 2,983 potentially relevant articles, 6 were finally included (Fig. 1) and are summarized in the present review (Table III). Two were longitudinal (27,37), of which one was retrospective (37) and the other one prospective (27). The other 4 studies included were cross-sectional (38-41). The 6 selected studies included a total of 1,284 participants. The age of the participants varied from birth to 20 years, but all the studies included boys and girls from 2 to 10 years of age. Two studies included children younger than 2 years (38,39), 2 studies focused only on children from 2 to 10 years (27,41), and 2 included adolescents (40) and young adults (37).
Table III. Descriptive characteristics of included studies on growth and nutritional status in children aged 2-10 years born with cleft lip and/or palate
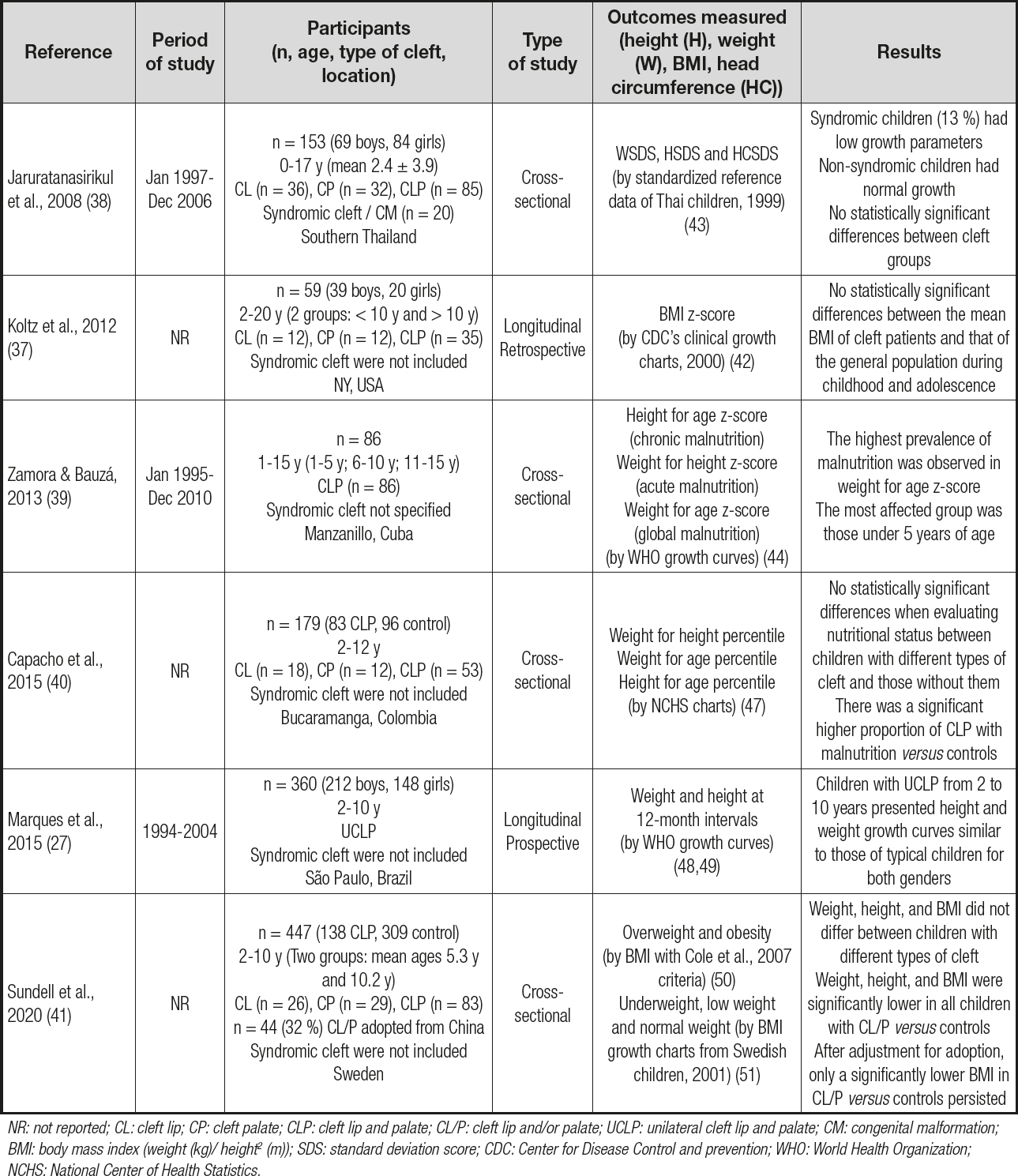
NR: not reported; CL: cleft lip; CP: cleft palate; CLP: cleft lip and palate; CL/P: cleft lip and/or palate; UCLP: unilateral cleft lip and palate; CM: congenital malformation; BMI: body mass index (weight (kg)/ height2 (m)); SDS: standard deviation score; CDC: Center for Disease Control and prevention; WHO: World Health Organization; NCHS: National Center of Health Statistics.
Concerning the population of the study, only 2 studies included just one type of cleft: UCLP in one of them (27) and CLP in the other one (39). All other studies included the three main groups of clefts: CL, CP, and CLP. Nevertheless, only 3 of them compared the outcomes depending on the type of cleft (38,40,41). Syndromic children were excluded in 4 of the studies (27,37,40,41), were specifically included and analyzed in 1 of them (38), and their presence was not clarified in the sample description of the other one (39).
Regarding the origin of the population of the studies, samples came from all over the world: Southern Thailand (38); NY, USA (37); Manzanillo, Cuba (39); Bucaramanga, Colombia (40); São Paulo, Brazil (27), and Sweden (41). The latter (41) also included adopted children from China (32 % in the group of children with CL/P), and the results were analyzed taken this into account. In each study patients belonged to the same sociodemographic level except in one, in which the results were investigated according to this condition (40).
Two studies (27,38) used the weight and height as measures, 2 studies (37,41) included BMI as outcome measure, and the other 2 studies (39,40) calculated indexes of nutritional status from height for age, weight for height, and weight for age. All the results obtained in each of the studies were normalized with growth charts from reference healthy counterparts, or z-scores were calculated. The population references used in each study are detailed in table III.
QUALITY ASSESSMENT
The obtained grade of quality assessment for each study is included in table II. Grades for the selected studies ranged from 75 % to 100 %. Most of the included studies in the present review were of good quality. In all studies two criteria were NA (‘not applicable') because the exposure (cleft condition) only had to be assessed once (criterion 10) and the outcome assessors did not have to be blinded in these kind of studies (criterion 12).
HEIGHT, WEIGHT AND BMI IN CLEFT CHILDREN AS COMPARED WITH THEIR COUNTERPARTS
The two longitudinal studies reviewed in this article did not show statistically significant differences in mean BMI z-scores (37) or height and weight growth curves (27) between cleft patients and the reference population. Koltz et al. (37), in a small sample (N = 59) with a wide age range (from 2 to 20 years, stratified in two groups: younger and older than 10 years, without detailing how many patients in each group), failed to find differences in mean BMI z-scores between cleft patients and CDC growth charts (42). Marques et al. (27) developed the only longitudinal growth study for boys and girls between 2 and 10 years of age in a large sample with the same type of cleft: UCLP. They constructed their own height and weight charts, and concluded that children with UCLP from 2 to 10 years of age presented growth patterns similar to those of their counterparts for both genders.
Jaruratanasirikul et al. (38), in a cross-sectional study, did not find any statistically significant differences either, by calculating in this case SDS for weight, height and head circumference using Thai population references (43). However, mean age at the time of the study was 2.4 ± 3.9 years, with 65 % of patients younger than 1 year; so, the results of this study cannot provide good answers about the population we wished to evaluate.
On the contrary, the other 3 studies found some differences between cleft children and their counterparts (39-41). Two studies (39,40) investigated the prevalence of malnutrition by the normalized measures of height for age (chronic malnutrition), weight for height (acute malnutrition), and weight for age (global malnutrition) (44); and the other one (41) compared mean weight, height, and BMI between cleft children and controls. Zamora & Bauzá (39) divided their study population into 3 age groups (1-5, 6-10, and 11-15 years). The most affected group was that under 5 years, with a prevalence of malnutrition of 11.8 % (weight for age z-score < -2 DE as criterion), 5.9 % (weight for age z-score < -3 DE as criterion), and 11.8 % (weight for height z-score < -2 DE as criterion). However, they also included children younger than 2 years, the sample size was small (n = 86), and they did not specify whether syndromic children had been included. Capacho et al. (40), in a group of CL/P children aged 6.7 years, detected more undernourished children (acute and chronic malnourishment) in the group with cleft as compared with those without cleft lip/palate (24.1 % vs 12.5 %; respectively, p = 0.043). At last, Sundell et al (41), in a sample of Swedish children from 2 to 10 years of age, divided into two groups (median 5.3 and 10.2 years), concluded that weight, height, and BMI were significantly lower in children with cleft lip/palate versus controls in both age groups, but after adjusting for adoption only the significantly lower BMI in CL/P versus controls persisted. In fact, when comparing underweight and low-weight prevalence by BMI classification between groups, this was higher both at 5 years and at 10 years in CL/P children than in controls.
Although none of the studies specifically assessed overweight and obesity in cleft children, the results did not show an increase in growth parameters in these children when compared to their counterparts. In one of the studies (41), categorized by BMI criteria (Table III), it was seen that the prevalence of overweight and obesity was not higher in cleft patients.
HEIGHT, WEIGHT AND BMI COMPARISONS BETWEEN GROUPS OF CLEFT PATIENTS
When the patients were divided into the three types of cleft (CL, CP and CLP), 3 studies did not find statistically significant differences between cleft groups (38,40,41). However, in one of these studies (38), the growth parameters in children with CP and CLP were apparently lower than in those with CL, but specific analyses between the different groups were not carried out, and statistical significance was not reported. The other 3 studies did not evaluate this aspect owing to their small sample size, as authors stated (37), or because only one type of cleft was included in the study (27,39).
SYNDROMIC CHILDREN
Only one study analyzed syndromic children with CL/P and compared them with nonsyndromic patients with cleft lip/palate (38). They concluded that children with syndromic cleft (13 % of the sample) had a poorer growth with statistically lower weight, height, and head circumference SDS. All other studies excluded syndromic children with CL/P (27,37,40,41), or it was not specifically reported whether this condition had been included (39).
SOCIODEMOGRAPHIC FACTORS, ORIGIN OR ADOPTION
An important aspect that must be pointed out is the socioeconomic and demographic conditions of the families in which children are born with this type of craniofacial anomaly, since this factor may influence the nutritional status of the child. Capacho et al (40), evaluated these sociodemographic variables, such as socioeconomic status and family income, and then selected children with similar conditions to avoid the influence of socioeconomic status on nutritional comparisons.
Sundell et al (41) included adopted children in their study (n = 44; 32 % in the group of children with CL/P), all of them from China. They concluded that children with CL/P who had been adopted from China were significantly lighter and shorter when compared to the rest of children with CL/P. This fact may be related both to ethnic differences and social and health care conditions in those internationally adopted children from regions and institutions where undernutrition and delayed growth are very common.
DISCUSSION
This systematic review aims to identify the existing literature on the nutritional prognosis of patients born with cleft lip and/or palate during childhood, the peculiarities of their body composition, and their growth patterns from two years of life on. Orofacial malformations may be severe enough to have a negative effect on growth and development, and in the specific case of cleft lip and/or palate, this effect might be also related to the high frequency of comorbidities in these patients (2). Besides, it is well recognized that CLP is a common component of numerous malformation syndromes (10,11), so this fact will also have to be taken into account.
This review identified 2 longitudinal (27,37) and 4 cross-sectional studies (38-41) with reliable data about the outcomes of interest. The selected studies showed widely varied results—3 of them found some growth differences between cleft children and their counterparts (39-41), but the other 3 did not find any (27,37,38). Taking into account the number of studies and the amount of patients included, we might say that the entire sample considered as a whole would be enough to answer our questions. However, among these 6 studies we found different types of design, including very heterogeneous samples, with different sizes and wide age ranges varying from 0 to 20 years. Furthermore, different groups of cleft lesions were selected for each study, patients came from a variety of origins, and authors assessed diverse outcome measures. All of the above prevented us from obtaining solid, reliable, homogeneous results. Moreover, in these studies only anthropometric parameters were used to assess nutritional status, and body composition or adiposity assessments were not reported in any of them. These study characteristics are the main limitations of this systematic review. Despite the Quality Assessment Tool report that all the studies included were of good quality (Table II), when the studies are analyzed together (Table III) that is not enough to draw summary conclusions.
A well-designed study of growth patterns requires a large longitudinal design. The two longitudinal studies (27,37), which are supposed to be more informative, did not show significant differences between cleft patients and their respective counterparts using adequate reference standards (CDC clinical growth charts (37) and WHO growth curves (27)). Nevertheless, on the one hand, Koltz et al. (37) studied a small sample (N = 59), insufficient both to guarantee results and to stratify them in different groups of clefts. On the other hand, Marques et al. (27), in order to have an homogeneous population in a large longitudinal prospective study (N = 360), included only children with the same type of cleft (UCLP) in a well-matched age range (2-10 years) for our aims. In the same sample, the authors previously analyzed infant growth from birth to 2 years of age (20), reporting an early impairment of length and weight, followed by compensatory catch-up growth at the end of the first year of life, and normalizing nutritional status at 2 years as compared to their peers.
The four cross-sectional studies varied in their conclusions. Jaruratanasirikul et al. (38) did not find any significant differences when comparing sample SDS for weight, height and head circumference with Thai population references (43). However, the median age of their sample was less than 1 year, which is quite far from the one intended to be analyzed in our review. On the other hand, in this study, growth parameters in children with CP and CLP were apparently lower than in those with CL, but this fact was not statistically analyzed. Some studies have already reported that growth problems are more frequent in children with CLP and isolated CP than in children with isolated CL (16,18,45,46). The other 3 cross-sectional studies found some differences between cleft lip/palate children and their counterparts (39-41). Zamora & Bauzá (39) analysed a small sample of Cuban children (N = 86) in which the most affected group was that under 5 years of age, which corresponds to the general concept (as explained in the introduction) that the highest prevalence of malnutrition is seen during infancy and early childhood. Capacho et al. (40) identified more undernourished children in the group with cleft lip/palate, although the selected population belonged to low and medium socioeconomic strata in Colombia, so this factor could have influenced the observed results. Sundell et al. (41), after adjusting for adoption, only observed a significantly lower BMI in CL/P versus controls. One third of the participating children with CL/P in this study were internationally adopted from China. International adoptees have increased the prevalence of children with CL/P in Sweden, and most of them have primary lip surgery performed before arrival in Sweden (41). Institutionalized cleft children waiting for adoption in their countries and having surgery have an increased risk of early undernutrition.
The available literature has shown that growth restriction due to early undernutrition maintained over time can affect nutritional status and subsequent growth potential, programming the child towards thinness, lower final height, and lower muscle mass (25). Moreover, the rapid catch-up period observed when nutritional intake is reestablished has been shown to program excessive growth and a higher risk of long-term adiposity (25,26). So, it would be reasonable to hypothesize that children with impaired early growth may maintain such lack of growth later in life. However, after examining the results from this review, we cannot confirm whether cleft children have a worse nutritional and growth prognosis than their counterparts, or the metabolic programming hypothesis towards excess adiposity. In the current landscape of children healthcare, due to the increasing prevalence of overweight and obesity, a better understanding of the nutritional status of CL/P patients over different age periods should be a priority.
After this systematic review, we cannot confirm that cleft children aged 2-10 years, excluding those with syndromes or coming from vulnerable populations (such as developing countries, low socioeconomic status, or international adoption), have different growth patterns or a worse nutritional status as compared to their counterparts. We cannot affirm whether any anthropometric differences exist between the different groups of cleft children (CL, CP and CLP). Nevertheless, syndromic patients and those internationally adopted from unfavorable nutritional environments have lower growth parameters and a higher risk of undernutrition. The prevalence of overweight and obesity does not seem to be higher in cleft patients during childhood, but the hypothesis of long-term metabolic programming towards excess weight due to early life periods of malnutrition has to be explored. Further, larger studies are needed to confirm the long-term consequences of cleft lip and/or palate malformations on the nutritional status and body composition of children with cleft lip/palate.
















