INTRODUCTION
Sarcopenia or the loss of muscle mass and function is an inevitable consequence of aging, malnutrition, chronic or terminal diseases. Patients hospitalized in intensive care units experience a dramatic loss of muscle mass, associated with an increased muscle catabolism. The net loss of muscle mass predicts the appearance of multiple organ failure 1. Among cancer patients, the loss of muscle mass and function is probably the consequence of the increased secretion of cytokines and other tumor-derived factors 2. It is also an important prognostic factor 3,4. An inadequate nutritional intake, especially of dietary protein, also contributes to the loss of muscle mass 5 and is a usual problem among patients with acute diseases or decompensated chronic conditions. Therefore, sarcopenia can also become a relevant problem in the acute care setting.
Among older people, sarcopenia assessed as a low muscle mass or function has a long term prognostic value for mortality 6 and functional impairment 7. However, there is less information concerning its prognostic value in the hospital setting. Since pneumonia acquired during hospitalization and dependence on ventilator assistance are relevant for the outcome of hospitalized patients 8, assessment of respiratory muscle function may be an important tool to determine the short term prognosis of sarcopenia. Measurement of maximal inspiratory and expiratory pressures requires an inexpensive equipment and it is not bothersome for the patient 9. In cardiac surgery, it is associated with time on mechanical ventilation 10. Therefore, it is worth exploring if these parameters could have a prognostic value in patients hospitalized in general medical and surgical wards.
Thus, the aim of this study was to explore the prognostic value of maximal inspiratory, expiratory and handgrip strength on the functional capacity and mortality of patients admitted to medical and surgical wards of a general hospital.
PATIENTS AND METHODS
Non-critical patients of both genders and over 18 years of age hospitalized in the medical and surgical wards of El Pino Hospital in Santiago de Chile were studied. Exclusion criteria were a projected hospitalization of less than five days, being pregnant, being admitted for scheduled elective surgery with an expected hospital stay of less than five days, physical conditions that prevented the measurement of grip strength and maximal respiratory pressures such as myopathies or neurological conditions, and patients with respiratory illness as cause of hospitalization. Both the Ethics Committee of the South Metropolitan Health Service and the Institute of Nutrition and Food Technology of the University of Chile approved the study. All patients gave written informed consent. All assessments were performed within the first 48 hours of hospital admission.
All demographic data, diagnoses, and treatments were obtained from the medical record of each patient. A single researcher performed all histories, physical examination, respiratory pressure and handgrip strength measurements (EC). Body weight and height were measured. Maximal respiratory pressures were measured using a DPM Collins manometer connected to a small chamber (20 mm length and 30 mm inner diameter) with a mouthpiece. A small leak in the chamber prevented the patients from using buccal muscles to generate the pressure. For maximal inspiratory pressure the patients were instructed to expire and to stop breathing at residual lung volume and try to sustain a maximal negative pressure for approximately one to two seconds. For maximal expiratory pressure, the patients were instructed to inspire and stop breathing at total lung capacity and to sustain a maximal positive pressure for one or two seconds 11. The patients were instructed how to perform the test and three measurements were done, recording the highest readings.
Maximal isometric handgrip strength was measured with a 1 kg precision 78010 Lafayette dynamometer. Measurements were performed with the patient in the sitting position, adducted shoulder, neutral forearm rotation, and with the elbow bent at 90 degrees. Three measurements were obtained in each hand and the highest reading was recorded. No dominance was considered.
Global subjective assessment of nutritional status was carried out using the protocol proposed by Detsky et al. 12, using a Spanish translation previously used by us 13. Patients were classified as A = well nourished, B = moderately malnourished or at risk for malnutrition and C = severely malnourished.
Apache II score was calculated using laboratory and clinical data of patients, also within 72 hours of admission, using the French Society for Anesthesia and Resuscitation calculator 14.
Functional status was determined on admission, and at 15 and 30 days after hospital admission using the Karnofsky performance scale 15. The procedure was performed at the patient bed if still hospitalized, or on an ambulatory basis if the patient was already discharged from hospital. After 30 days of hospitalization, a decrease in two categories in the scale, compared to the initial score, was considered as a decline in functional status. Survival during the same period was also recorded.
DATA ANALYSIS AND STATISTICAL CALCULATIONS
To obtain normal values for handgrip strength and maximal inspiratory and expiratory pressures, measurements were performed in 366 healthy subjects aged 20 to 89 years (255 females) of a similar socioeconomic status of the studied patients. The mean value for each parameter and its standard deviation were calculated for each gender in ten year intervals from 20 years of age to over 80. Measurements obtained in patients were expressed as absolute values and z-scores of age and gender normal values.
Normality of variable distribution was determined using the Shapiro-Wilk test. Variables with a normal distribution are expressed as mean ± standard deviation, otherwise as median (interquartile range). The Student's t test or the Kruskal-Wallis test were used to compare variables with normal or non-normal distributions. Proportions were compared with Chi-squared tests, with Yates correction when necessary. Logistic regression models were used to determine which parameters predicted mortality or functional decline in the studied patients. In these models, categorical variables such as gender or subjective global assessment were expanded into indicator variable sets, also called dummies. Models were designed with those variables that were significantly different in univariate analysis. Maximal inspiratory and expiratory pressures and handgrip strength were included as absolute values or z-scores in different models. All statistical calculations were done on Stata 12 for Windows (Statacorp. Texas 77845, United States).
RESULTS
During a three months period, 108 patients who met the inclusion criteria were recruited. Of these, ten were excluded due to a hospital stay of less than five days and eight due to a failure in obtaining all the clinical data necessary for the study. Therefore, 90 patients aged 58 ± 16 years (46 women) were studied. Of these, 35 had cardiovascular diseases; 25, gastrointestinal conditions; 14, infections; nine, kidney diseases; two, diabetes; and two, cancer. Baseline clinical features, respiratory and handgrip strength values of studied patients are shown in Table I. No differences in these features were observed according to the underlying diagnoses of patients.
Table I. Baseline features of studied patients (mean ± standard deviation)

*Probability for differences between men and women.
Table II. Baseline features of patients who survived or died during the observation period expressed as mean ± standard deviation or median (interquartile range)

*Probability for differences between groups. †A: well nourished; B: moderately malnourished; C: severely malnourished. ‡Number of patients per category.
During the 30 days observation period, six patients died and nine had a decline in Karnofsky performance scale. Baseline features of patients who survived or died during the observation period are shown in Table II. Deceased patients had a worst baseline subjective global assessment, lower maximal expiratory pressure and handgrip strength. The differences were significant when the later parameters were expressed as absolute values or z-scores. Baseline features of patients who did no experience a functional decline, those whose functional status declined or died or those whose functional status declined but survived are shown in Table III. Patients who experienced a functional decline or died were older and had a lower maximal expirtory pressure, either expressed as absolute value or as z-score and a lower absolute value of handgrip strength. Among those who experienced a functional decline but survived, no significant differences in any parameter, were observed.
Table III. Baseline features of patients according to their functional decline during the observation period expressed as mean ± standard deviation or median (interquartile range)
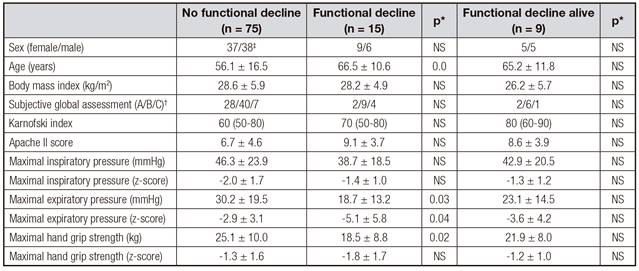
*Probability for differences with patients without functional decline. †A: well nourished; B: moderately malnourished; C: severely malnourished. ‡Number of patients per category.
Logistic regression models for mortality and functional decline are shown in Table IV. The only significant predictor of 30 days mortality or functional decline and mortality was maximal expiratory pressure, expressed as a z-score. Again, in the models in which functional decline excluding deceased patients was used as the dependent variable, none of the tested parameters had a significant predictive capacity.
Table IV. Logistic regression models for mortality or functional decline including only those variables that were significant on univariate analysis

*Probability. †Subjective global assessment of nutritional status; A: well nourished, B: moderately malnourished and C: severely malnourished. ‡Odds ratio (95% confidence intervals).
DISCUSSION
The main result of this observational study is that maximal expiratory pressure upon admission was an independent and significant predictor of mortality and functional decline in this group of hospitalized patients.
The prediction of mortality, incidence of complications and functional impairment is of utmost importance among hospitalized patients. The Acute Physiology and Chronic Health Evaluation II (APACHE II) 16 score was developed to predict mortality among intensive care patients, and it is still a reliable instrument 17. This score is calculated from disease related items and organ function. Nutritional status assessment should predict the incidence of complications. Among the nutritional scores with high predictive value, we chose the subjective global assessment, which is easy to apply and has a low interrater variability 18. Functional impairment prior or during hospital stay is especially relevant in older people, since it predicts outcomes in terms of independence and is also associated with a higher rate of readmission 19 and mortality 20. The importance of maintaining mobility and functionality during hospital stay is underscored by trials showing that mobility enhancing programs improve outcomes in terms of independence after discharge 21.
Since mobility and functionality are important prognostic factors during hospital stay, assessment of muscle performance should be a valuable tool to assess clinical outcome. The long term prognostic value of hand grip strength and other functional measures is undisputable 22. In the hospital setting we showed that this measurement predicts functional impairment during hospital stay 23,24. Maximal inspiratory and expiratory pressures measure thoracic muscle strength, without interferences from airflow limitations 25. These muscles are important to maintain an adequate respiratory capacity, thus influencing oxygen and artificial ventilation requirements, but should also serve as global indicators of muscle mass and function. The finding of this study showing that maximal expiratory pressure predicts mortality and functional impairment in hospitalized patients is novel. The logistic regression models show that this measurement outweighs handgrip strength and subjective global assessment as prognostic indicators. However, a study with a larger number of patients should be performed to determine the additive significance in prognosis that a combination of these assessments could have.
As shown in the results, maximal expiratory pressure is a significant predictive tool only when it is expressed as a z-score of normative values in healthy age and gender matched individuals. Since muscle strength measurements are so dependent on age and gender, informing them as absolute values can be misleading 26. Moreover, normal values cannot be extrapolated from one region to another. Those obtained in North American populations are different to those of Latin American subjects 27. Therefore, obtaining local standards in subjects of the same country and socioeconomic status becomes relevant. For the present study, handgrip and respiratory muscle strength were measured in a significant number of healthy people; therefore, our z-score calculation can be considered as reliable.
The main weakness of this study is the low number of patients studied and that they all were admitted to the same hospital. The ideal would be to perform the study in several hospitals to observe if results were maintained. This is a pending task that should be carried out in the future. However, we detected that maximal expiratory pressure has a significant predictive value for death and functional impairment, even with the low number of observations, which increase the validity of the observation. The strengths of the study are that all the observations and measurements were carried out by the same researcher (EC), that in very few patients we were not able to obtain all the required clinical data and having a significant number of measurements in healthy people to be able to calculate accurate z scores.
In conclusion, maximal expiratory pressure deserves future studies to determine its real value as a prognostic parameter, along with hand grip strength, in hospitalized patients.














