Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista Española de Enfermedades Digestivas
versão impressa ISSN 1130-0108
Rev. esp. enferm. dig. vol.109 no.5 Madrid Mai. 2017
PICTURES IN DIGESTIVE PATHOLOGY
Choledochocele as an atypical cause of relapsing acute pancreatitis: diagnosis and endoscopic treatment
Coledococele como causa atípica de pancreatitis aguda de repetición: diagnóstico y tratamiento endoscópico
Cristina Saldaña-Dueñas, Juan José Vila-Costa and Ignacio Fernández-Urién
Department of Digestive Diseases. Complejo Hospitalario de Navarra. Pamplona, Spain
Case report
We present the case of a 56 year old patient with a regular follow-up due to relapsing acute biliary pancreatitis events (microlithiasis). After the cholecystectomy he suffered a new episode of pancreatitis, so an endoscopic ultrasonography study (EUS) was performed.
The EUS showed a large cystic duct remnant without any content inside, as well as the pancreas, Wirsung and biliary duct with no abnormalities.
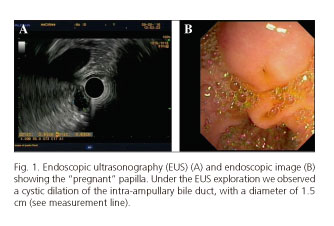
We observed a cystic dilatation of the intra-ampullary bile duct, of 1.5 cm in diameter with hyperechogenic content inside (Fig. 1). In light of a suspected type A choledochocele (Sarris and Tsang classification) an endoscopic retrograde cholangiopancreatography (ERCP) was performed (1).
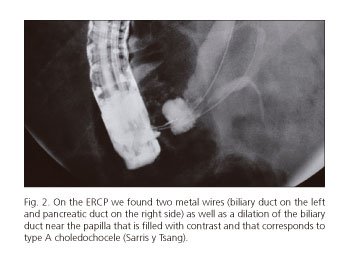
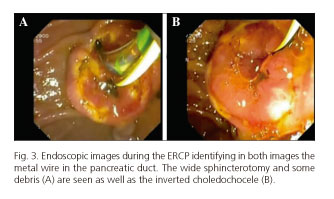
The ERCP identified a "pregnant" papilla (Fig. 1), and after the bile duct cannulation the cholangiography confirmed the EUS findings (Fig. 2). After performing the sphincterotomy, some pinpoint debris appeared (biliary sludge) (Fig. 3). The pancreatic duct was then cannulated and a prophylactic plastic stent was placed. We took biopsies of the inverted choledochocele.
The histology samples had both biliary mucosa and columnar epithelium (duodenal), fibrosis and inflammatory infiltration that confirmed the suspicion of choledochocele. No dysplasia was identified.
After the procedure the patient evolved favorably and was discharged from hospital without gastrointestinal symptoms.
Discussion
The choledochocele is a cystic dilatation of the intraduodenal portion of the bile duct and corresponds to the type III biliary cysts in Todani's classification (2,3). The Sarris and Tsang classification of choledochoceles can differentiate the cyst types on the basis of their morphology and also provides different treatment approaches (1-3). They have wide presentations, from asymptomatic to abdominal pain, cholangitis and relapsing pancreatitis.
There is a low risk of malignancy (< 2.5%) (1-3). The diagnosis is made by imaging techniques (cholangio-MR, EUS) and the treatment is based on surgical or endoscopic resection or endoscopic sphincterotomy (2).
References
1. Sarris GE, Tsang D. Choledochocele: Case report, literature review, and a proposed classification. Surgery 1989;105(3):408-14. [ Links ]
2. Culetto A, Miranda-García P, Tellechea JI, et al. Endoscopic treatment of a choledochocele. Endoscopy 2016;48. DOI: 10.1055/s-0042-114428. [ Links ]
3. Uribarrena Amezaga R, Fuentes Olmo J, Raventós Irigoyen N, et al. Coledococele complicado con carcinoma de páncreas en un paciente de edad avanzada. Diagnóstico y tratamiento endoscópico. Rev Esp Enferm Dig 2010;102(5):344-6. [ Links ]











 texto em
texto em