INTRODUCTION
Intestinal parasitic infection (PI) is a major health problem in developing countries. Globally, two billion individuals are infected with intestinal parasites; out of these, the majority of them are children. An increasing trend in intestinal PIs has been recorded in developing countries because of low socioeconomic status, low literacy rate, poor awareness among the parents regarding PI and their mode of transmission, poor quality of drinking water, inappropriate hygiene and sanitation and hot and humid tropical climate 1,2. Parasitic infection has been linked with an increased risk for nutritional anemia, protein-energy malnutrition and growth deficits in children, loss of weight in pregnancy and intrauterine growth retardation followed by low birth weight 1,3.
Globally, worm infestation is the most common health issue among children in developing countries, particularly in those living in the rural and remote areas. However, wide ranges in the prevalence of PI among children have been reported within regions or countries and between the countries. In recent studies, enormously different prevalence rates in intestinal parasites were observed in different developing countries: 60% in Rwanda (age: 5-60 months) (4), 47% in Peru (3-12 years) 5, 51.7% in Nigeria (2-5 years) 6, 26% in Venezuela (< 2 years) 7, 25-70% in Cambodia in different child age groups of children 8,9,10, 51% in India (< 24 months) 11, and 20-70% reported from various regions of Pakistan in different child age groups 12,13.
Children under five years of age present higher risk of malnutrition because of their high nutrient requirements for rapid physical and physiological growth. Multidimensional biological, environmental and behavioral factors influence childhood malnutrition 14. A number of previous studies demonstrated association between PI and different forms of malnutrition in children 4,15. Similarly, anemia, being characterized by blood hemoglobin concentration below the established cut-off level, is also a common public health problem of the developing world. The global prevalence of anemia in the preschool children is 43% 16, which contributes substantially to childhood mortality and morbidity. In Pakistan, the reported prevalence of anemia in preschoolers is between 40-70% in different areas and regions. The previous literature has shown significant association of anemia with impaired brain development and cognitive functions among children. A diverse range of risk factors including PIs likely contribute to its etiology in various age groups 1,17.
Several studies have been conducted in Pakistan to estimate the severity of the problem of PI in different age groups. Most of these studies focused on the prevalence rate of PI in the community. There is no recent information about intestinal PI and its impact on nutritional status of young children in Pakistan. The present study was designed to estimate the severity of the problem of malnutrition and anemia in association with PI among the young children and to identify the potential risk factors contributing to these health issues.
METHODS
STUDY LOCATION AND SETTINGS
This cross-sectional study was conducted in a rural area of Peshawar, the capital city of the Khyber Pakhtunkhwa province of Pakistan. The study was conducted between March 2014 and October 2016 on preschool children (6-59 months). Peshawar has a semi-arid climate, with very hot summers and mild winters. Winter in Peshawar starts in November and ends in late March, although it sometimes extends into mid-April, while the summer months are from mid-May to mid-September or early October. The mean maximum summer temperature surpasses 40 °C (104 °F) during the hottest month, and the mean minimum temperature is 25 °C (77 °F). The mean minimum temperature during the coolest month is 4 °C (39 °F), while the maximum is 18.3 °C (64.9 °F).
SAMPLE SIZE AND PROCEDURE
A sample size of 385 children was estimated considering a prevalence of worm infestation of 50% in rural and semi-urban areas, with a precision of 5% and alpha-error of 0.05. However, the sample size was increased to 450 in order to compensate the expected 15-20% non-response rate. Peshawar has three rural health centers where households and families from the surrounding rural areas (villages and remote countryside) get registration of their children for routine immunization and other health facilities. Children aged 6-59 months were identified and randomly selected from the records of the three rural health centers. Inclusion criteria were: children free from any chronic/inborn disease, and who had no acute diarrhea, constipation or dysentery. Infants > 6 months with exclusively breastfeeding were also excluded. Children's families were approached; only one child per household was included after obtaining written informed consent from the parent/caregiver. The study was approved by the university ethical review committee.
DATA COLLECTION
Pretested questionnaires, containing both closed and open ended questions, were used to collect data on socioeconomic-demographic status, child medical history including worm infection in the past and health characteristics, and household hygiene and sanitation status. Child's mothers, fathers or caregivers were thoroughly interviewed by trained graduates to gather all the required information. Standardized equipment was used to assess maternal and child nutritional, and child worm infestation statuses in well-established laboratories of the health centers.
A structured questionnaire was used to collect data on socioeconomic-demographic status and health characteristics of the children. The questionnaire included information on household monthly income (in Pakistani rupees), family type (joint or nuclear) and size, home infrastructure (muddy or concrete), and parental characteristics (such as age and formal education). Family size was defined as the total number of individuals, including the child parents, grandparents, parity, and other relatives sharing the same kitchen. Questions on child characteristics included recent medical history (such as any digestive or respiratory problems), current use of medicine, regular medication for worm infestation and pica habit. Questions were asked in the local language and all the information was recorded on the questionnaire.
A pretested questionnaire was used to assess awareness level and perception of mothers about PI, mode of parasites transmission, safety and precautionary measures to control worms, child caring and nutrition, and home hygiene and sanitation. The questionnaire had specific close-ended questions for each section. Mothers' responses were indicated on a three point scale, ranging from "totally wrong", "partially true", and "correct". A total score for each section was calculated and a grand score value for each respondent was obtained by adding the scores of each section. Mothers above the median of grand score were considered as having "sufficient awareness of overall child health" as compared to those below the median.
Children with both visible and invisible worms were identified by trained graduates using the recommended procedure under the supervision of project investigators. For stool collection, mothers/caretakers were properly guided regarding sample collection in dry, clean leak proof containers labelled with the name and identification number of the child. Physical examination of the stool samples was done by noticing stool color, consistency, presence or absence of mucus and blood and the visibility of worms. Type of worms present in the stool was confirmed and recorded.
Recommended laboratory techniques were used to diagnose invisible worms 18. Invisible worms in fresh stool samples were diagnosed using the "direct wet mount method", in which microscope slides were made from fecal specimen (about 2 mg), 1-2 drops of saline solution and a drop of Lugol's iodine for examination under low (x10) and high power (x40). The addition of a drop of Lugol's iodine stains the cysts, making them easier to identify. Saline iodine wet mount identified parasites, protozoan trophozoites and cyst, helminth ova and larvae. All stool samples were then processed by formalin-ether sedimentation concentration and examined similarly under 10x and 40x magnifications to identify the protozoan cysts. Pictures and atlases provided by authentic and well-established sources were used to identify parasites.
Nutritional statuses of mothers and their children were assessed. Mothers of the selected children were assessed for nutritional status by taking body weight and height without shoes and in lightweight clothing to the nearest 0.1 kg and 0.1 cm, respectively. Mothers' body mass indexes (BMI) were calculated using their weight and height measurements. Children nutritional and anemia statuses were evaluated by measuring their body weight, length/height and blood hemoglobin level. Weight was taken to the nearest 0.1 kg by using pediatrics scale for less than two-year-old children and electronic digital scale for younger children (3-5 years). Length board/recombinant length scale was used for measuring the length of infants and height scale was used for younger children to the nearest 0.1 cm. All of the anthropometric measurements were taken using recommended procedures of the World Health Organization (WHO) and standardized equipment.
The children anthropometric measurements were compared with the WHO 2006 growth standards to identify malnourished children. Standard deviation or Z-scores for "weight-for-age' (WAZ), "length/height-for-age" (L/HAZ) and "weight-for- length/height" (WAL/HZ) of the children were generated using the WHO recommended Anthro software. Children with standard deviation score < -2 for WAZ, L/HAZ and WAL/HZ were identified as underweight, stunted and wasted, respectively. However, children who had all of the WAZ, L/HAZ and WAL/HZ values below -2 were grouped together and collectively declared as undernourished.
HemoCue(r) was used to measure the hemoglobin concentration of children by taking 2-3 drops of blood in disposable strips used in the HemoCue(r) micro-cuvette 19. First, the instrument was calibrated for the accuracy of hemoglobin level. A control cuvette was applied to the instrument holder to verify the stability of the HemoCue(r). The accuracy of the instrument was checked repeatedly with the control cuvette after the analysis of 10-12 blood samples. To measure Hb levels, the middle/ring finger of the child was cleaned at the side of the fingertip by alcohol swab, and then punctured with the lancet. First, 2-3 drops were wiped away; the next large drop of blood was transferred to a micro-cuvette and placed in the HemoCue(r) for the results. The results appeared in approximately 15-60 seconds in g/dl and recorded. Anemia was defined as a hemoglobin < 12 g/dl.
STATISTICAL ANALYSIS
Data were entered and analyzed using the statistical package SPSS version 20 (SPSS, Inc., Chicago, IL, USA). Data was first checked for entry errors and distribution using appropriate descriptive tests such as frequency, mean, mode, and Kolmogorov-Smirnov. The 95% confidence intervals (95% CI) of percentages were calculated based on the standard error. Logistic regression tests were used to investigate the association of potential social, demographic, health and nutritional variables with the status of PI among children; independent predictors of PI were identified and their associations with the outcome variable were reported as adjusted odds ratio (OR) with 95% CI. The differences were considered to be statistically significant at p < 0.05.
RESULTS
Required information for the current analysis was available on 437 (97%) mother-child pairs, including data on socioeconomic-demographic status, nutritional indicators, worm infestation among children, and hygiene and sanitation status at household levels. General characteristics of the study participants are summarized in Table 1. The mean age of the mothers and children was 27 ± 3.7 year and 24 ± 10 months, respectively; 48% (n = 210) of the study children were female. Average family size of the respondents was 6 ± 1.6, with a mean monthly income (thousands) of PKR 18 ± 5.5. The mean monthly income of the families was closed to the 3rd quintile of the national monthly household income of Pakistani rural population 20. Most of the children were living in joint family systems, muddy homes with open sewage system, and had illiterate or low-educated parents. However, 58% (n = 253) of mothers had some knowledge of overall child health, i.e., awareness on PI, mode of parasites transmission, safety and precautionary measures to control worms, child caring and nutrition, and home hygiene and sanitation.
Table I. General characteristics of the study subjects (n = 437)
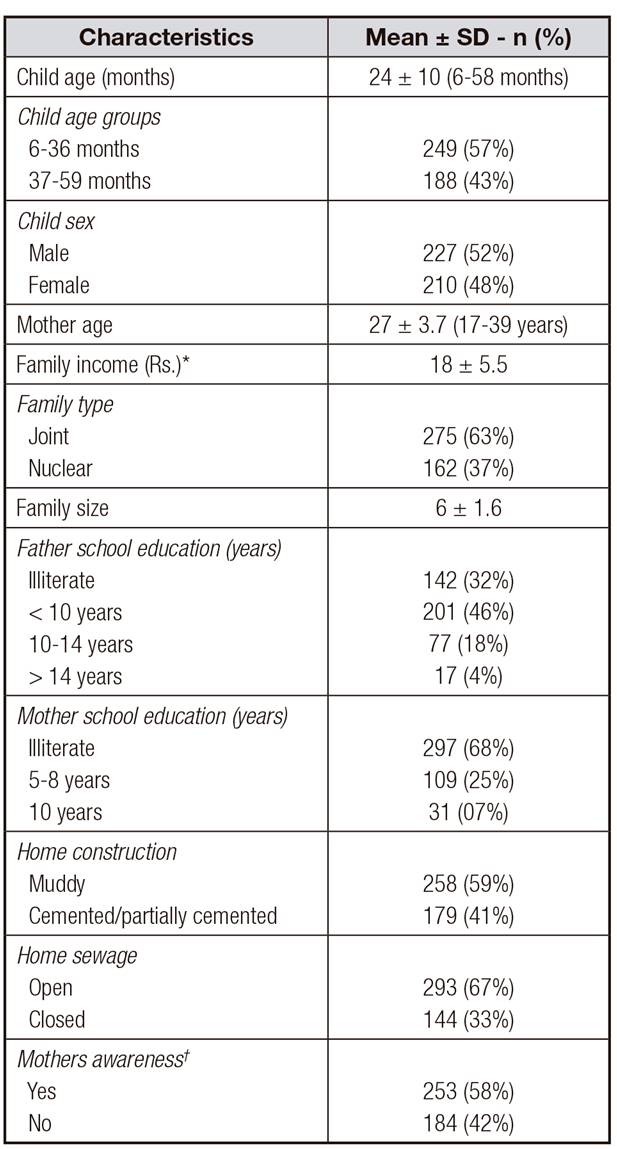
*In thousands (Pakistani rupees [PKR], 1 USD = 105 PKR).
†Awareness of PIs, mode of parasites transmission, safety and precautionary measures to control worms, child caring and nutrition, and home hygiene and sanitation
Table 2 shows results on the respondents' health and nutritional status. A total of 120 (27.5%) fecal samples were positive for various worms, including both visible (round worm, tape worm, pin worm and thread worms) and invisible worms (giardia, coccidia, whip worm and hook worm). A child being positive for single or multiple worm infestation was declared as "infected" and compared with the rest of children for different characteristics. Average WAZ, WL/HZ and L/HAZ of the children was -1.5 ± 1.2, -1.4 ± 1.5 and -1.7 ± 1.4, respectively. Of the total, 205 (47%), 109 (25%) and 140 (32%) children were stunted, wasted and underweight, respectively. Overall, 83 (19%) of the children had z-scores below -2 for all the three indicators of malnutrition and were grouped as "undernourished". Based on the recommended cut-off value for blood Hb, 267 (61%) children were found as anemic. The mean BMI of mothers was 21.08 ± 3.7 (range: 14.87-33.19); the minimum and maximum BMI values showed the presence of both underweight and overweight mothers in the study sample.
Table II. Health and nutritional status of the children

*Infections with single or multiple parasites.
†Children had WAZ, L/HAZ and WAL/HZ values < -2.
Prevalence of malnutrition (undernutrition, underweight, wasting and stunting) and anemia among children by PIs status was evaluated (Fig. 1). There were no statistical differences among the groups in the prevalence of "underweight" and "stunting" (p > 0.05). Most of the wasted (59% versus 41%) and anemic (66% versus 34%) children were worm infested; these differences in the percentages were statistically different (p < 0.05). Overall, 61% of the undernourished children were infected (p < 0.05).

Figure 1. Malnutrition and anemia in children by parasitic infection status. Note: percent values in bold are statistically different between the groups (p < 0.05). *Children had WAZ, L/HAZ and WAL/H < -2.
Figure 2 displays findings on risk factors and their corresponding adjusted OR (95% CI) for PIs in children. Among parental characteristics, mothers' BMI (adjusted OR: 0.56, 95% CI: 0.07-0.98) and awareness (adjusted OR: 3.00, 95% CI: 2.45-3.60) and fathers' formal education (adjusted OR: 2.43, 95% CI: 1.09-3.10) had independent association with PIs. Similarly, among child characteristics examined, pica habit (adjusted OR: 2.23, 95% CI: 1.89-3.03) and age (adjusted OR: 2.32, 95% CI: 1.70-3.21) were associated with PIs. Children living in the houses with open sewage system were 1.76 time more at risk for worm infestation as compared to those living with closed sewage system (adjusted OR: 1.76, 95% CI: 1.06-2.61). Among sociodemographic characteristics, only family size had association with PIs (adjusted OR: 2.02, 95% CI: 1.61-2.71).
DISCUSSION
Epidemiological studies on the prevalence of acute and chronic health problems and predisposing risk factors are essential to design appropriate intervention strategies, particularly for the vulnerable population of young children. The current study was aimed to assess the status of malnutrition and anemia in association with PI among the young children and to identify the potential risk factors for PI in the study area. Parasitic infection has been reported among the major contributing factors for child malnutrition and anemia in the developing world, leading to growth retardation and other adverse health consequences. Findings of the current study revealed the prevalence of malnutrition and anemia in association with worm infestation in a significant number of the study children. Other risk factors associated with anemia and malnutrition were age, family size, family income, mothers' BMI and awareness level, fathers' education and child recent medical history.
Our data found associations of malnutrition (based on anthropometric measurements) with PI; infected children were more likely to be wasted in comparison to the rest. There are discrepancies in the available literature on the association between the anthropometric indices and PI as some studies had positive results 21,22 whereas others reported no relationship 12,23,24. Our findings demonstrated an association between the prevalence of malnutrition and worm infestation among the study children. The overall prevalence of anemia in the current study was 61%, which is closed to the 2011 national prevalence report for the country for children under five years of age 25. Our study confirmed the association between worm infestation and the risk of anemia in the subjects as well. Children infected with intestinal parasites were more anemic than those who were not infected, which shows a similar association as the one previously reported in different developing countries 26,27. Parasitic infections are closely related to anemia and malnutrition. Most of the parasites, such as hookworm infections, cause mucosal damage resulting in endogenous losses of iron and other trace micronutrients. Parasitic infections resulting in bleeding (e.g., hookworm infection) are known to be predictors for iron deficiency anemia 28,29. Results of the current study suggest that infected children might have parasites-related comorbidities such as anorexia, nausea and vomiting, reductions in digestion and absorption, increased metabolic requirements, and enhanced nutrient losses that could lead to adverse health consequences 30,31-32.
Previous studies from different developing countries have identified various socio-demographic and environmental factors associated with PI among children. The findings from multivariate logistic regression analyses in the current study showed a considerably higher risk of worm infestation among children having various characteristics, including mothers' low BMI, open sewage system or poor sanitation at home, pica habit, child age, family size, fathers' illiteracy and mothers' poor awareness level. The association between mothers' nutritional status as manifested by BMI and PI could be explained by the fact that malnourished and unhealthy mothers might not be able to properly maintain the household hygiene status and look after their children. Previous literature supported the relationship between maternal and child health and nutrition statues 33,34-35. Most mothers in the current study were not educated formally, but showed somehow awareness of PI and related health knowledge. A negative association between maternal awareness level and the odds of PI in the children was evident. Mothers' awareness level played a significant role in lowering the likelihood of PI among children. Awareness, particularly about the mode of parasitic transmission, could enable the mothers or caregivers to modify the child's life style and living environment. Paternal formal education was significantly associated with the absence of PI among children. Education levels, particularly regarding decision-making partners such as fathers in the study area, might have a direct impact on children's health because it increases the ability to acquire and process information. Overall education helps parents to make better health investments for themselves and their children and may result in better parenting in general 36.
Visible sewage and poor sanitation, child pica, and exposure to soil-transmitted parasites have been frequently reported among the leading causes for PIs among children. Child age had a significant effect, probably because we studied such a wide age range (6-59 months). On average, for a unit increase in child age, the odds of having worm infestation increases by a factor of 2.32 (Fig. 2). As the children get older, exposure to soil-transmitted parasites becomes higher than that of their younger counterparts because of the increase in indoor and outdoor physical activities. The current study was conducted in rural slums where most of the constructions are either muddy or semi-cemented and most houses have open sanitation and sewage systems. This increases the risk of parasite transmission in preschool children. Hands and fingers of children might be easily contaminated with soil that contains cyst and eggs of parasitic organism, leading to intestinal PI. Parasitic infection had been shown to be initiated in early childhood in different previous research 32,37,38.
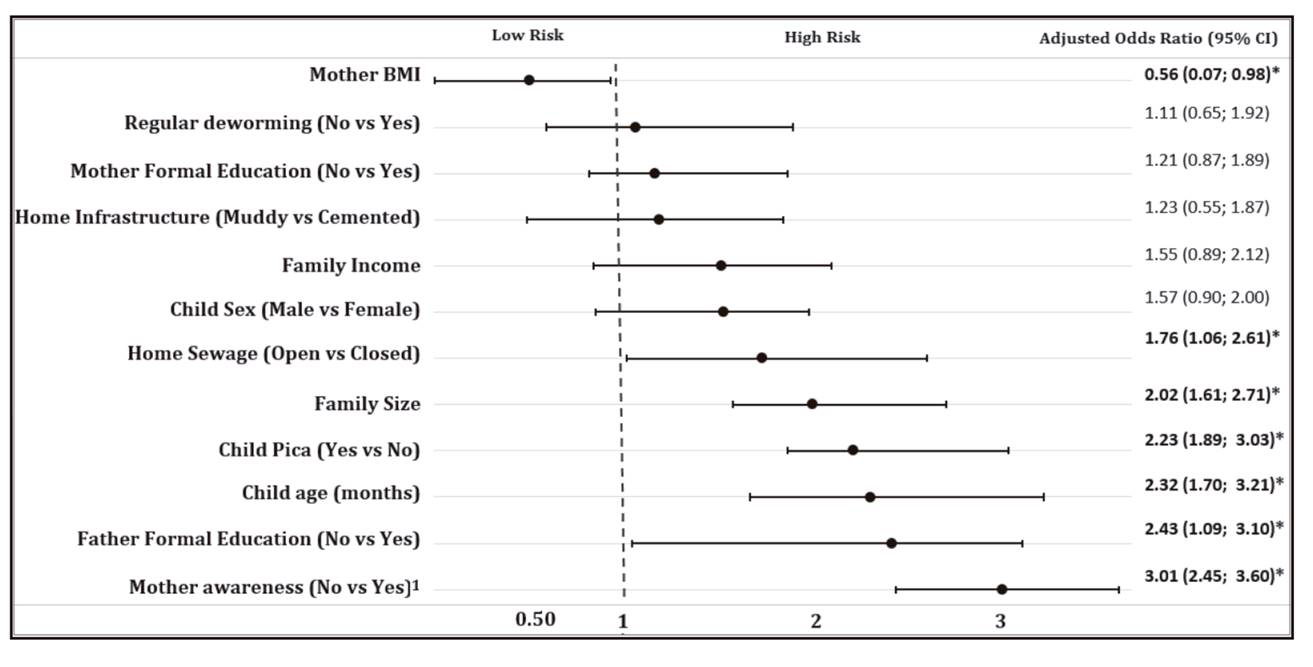
Figure 2. Maternal and child health, and sociodemographic associates of worm infestation. 1Awareness of PIs, mode of parasites transmission, safety and precautionary measures to control worms, child caring and nutrition, and home hygiene and sanitation. *p < 0.05.
The present study showed that the likelihood of PI in children increased with the increase in family size. Previous studies conducted in different developing countries showed a similar trend 39.
The possible explanation for this association might be that overcrowding and larger family sizes can easily lead to major problems, such as poor sanitation and personal hygiene, which promote the likelihood of parasitic transmission and increase the susceptibility of family members to PIs.
Our study has certain limitations. This study was of cross-sectional study in nature; therefore, our results only reflect one point in time in the study area which has a hot humid summer season between March and October. It was assumed that prevalence of PIs might be higher in this season as children are more exposed to dust, mud and consumption of unwashed fresh foods such as fruits. This exposure is much higher in children living in the rural slums of developing countries where most of the constructions are not cemented. The second limitation is the unavailability of dietary information for current analysis to explore its association with the subjects' nutritional and hemoglobin status. However, this limitation was offset by adding the variable of family income in the analysis, which predicts the level of household food security. Third, the findings presented here are representative of the selected rural areas of the north western region and cannot be generalized for all of the country.
This study has certain strengths. The sample size was pretty large to represent the study area. Among the participants, gender distribution was fair, with 48 percent of females and 52 percent of males. As per the knowledge of the investigators, this is the first study in the north-west region of Pakistan focusing on preschool children of rural slum areas to investigate the association of anemia and malnutrition with PI. A major strength of the study is the high response rate (97%). Similarly, as planned, the stool sample testing was conducted within 2-3 hours of collection. This was possible as the facilities of worm infestation determination were available in the laboratories of local hospitals. Based on previous literature, potential confounders were identified and detailed data were collected to adjust their effects.
CONCLUSIONS
Our results showed that almost one third of the children had infestation of different parasites which were associated with poor health outcomes among children. Overall malnutrition and anemia were highly prevalent in children in association with PI. Parasitic infection was found to be an independent risk factor for malnutrition and anemia among preschoolers. Among the different possible risk factors evaluated in the current study, mother nutrition status as assessed by BMI, open home sewage, larger family size, child pica habit, child increasing age and mothers' poor awareness of overall child health were strongly associated with intestinal PI.
Mothers health and awareness level play a significant role in the control of worm infestation among young children. Similarly, household hygiene and sanitation has a direct impact on overall child health. Therefore, all relevant stakeholders should be involved to design and implement mini developmental projects for the promotion of maternal nutrition status and awareness level, personal and environmental hygiene, household sanitation, control of PI, and drinking water quality improvement.














