Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Nutrición Hospitalaria
versión On-line ISSN 1699-5198versión impresa ISSN 0212-1611
Nutr. Hosp. vol.34 no.6 Madrid nov./dic. 2017
https://dx.doi.org/10.20960/nh.1028
Resistin in morbidly obese patients before and after gastric bypass surgery
Resistina en obesos mórbidos antes y después de un bypass gástrico
Elena Parreño Caparrós1, Fátima Illán Gómez2, Manuel Gonzálvez Ortega3, Isabel Orea Soler2, Matías Pérez Paredes3, M.ª Luisa Lozano Almela4, Elena Arjonilla Sampedro2 and Marisol Alcaráz Tafalla2
1Department of Endocrinology and Nutrition. Hospital de la Vega Lorenzo Guirao. Cieza, Murcia. Spain.
2Department of Endocrinology and Nutrition. Hospital Universitario Morales Meseguer. Murcia, Spain.
3Department of Cardiology. Hospital Universitario Morales Meseguer. Murcia, Spain.
4Department of Hematology. Regional Blood Donation Center. Murcia, Spain
Funding: This study was financed by the Fundación para la Formación e Investigación Sanitarias de la Región de Murcia (FFIS) (FFIS project/EMER09/10).
ABSTRACT
Background and objectives: Resistin was originally suggested to be a potential mediator of obesity-related insulin resistance in rodents. However, in humans, the role of resistin in obesity and insulin resistance has not yet been demonstrated. The present study investigates whether there are differences in resistin levels between patients with morbid obesity and lean subjects, and analyzes changes in resistin levels after significant weight loss secondary to bariatric surgery.
Methods: Sixty-eight patients with morbid obesity (body mass index [BMI] ≥ 40 kg/m2) and 31 lean subjects (BMI < 25 kg/m2) were selected. The study variables were: weight, height, BMI, waist-hip ratio (WHR), fat mass, family history of cardiovascular disease (CVD), type 2 diabetes mellitus (DM), hypertension, dyslipidemia, smoking, glucose, glycated hemoglobin (HbA1c), insulin, high-sensitivity C-reactive protein (hsCRP), interleukin-6 (IL-6), adiponectin and resistin. Homoeostasis model assessment (HOMA) and quantitative insulin sensitivity check index (QUICKI) were calculated. The obese patients underwent gastric bypass surgery, and the above mentioned variables were reassessed after 12 months and major weight loss.
Results: There were no significant differences in resistin levels between morbidly obese patients and healthy subjects of normal weight, or between obese patients before and after weight loss. Resistin levels in morbidly obese patients were not correlated to adiposity anthropometric measures, insulin, glucose, HOMA, QUICKI, hsCRP, IL-6 or adiponectin. In the morbid obesity group, after one year of weight loss, the only study parameter correlated to resistin levels was IL-6.
Conclusion: Our results do not support a relationship among resistin levels, obesity and insulin resistance in humans.
Key words: Resistin. Obesity. Gastric bypass. Insulin resistance.
RESUMEN
Introducción y objetivos: inicialmente se sugirió que la resistina era un mediador potencial de la resistencia a la insulina relacionada con la obesidad en roedores. Sin embargo, en seres humanos, el papel de la resistina en la obesidad y la resistencia a la insulina aún no se ha demostrado. El presente estudio investiga si existen diferencias en los niveles de resistina entre pacientes con obesidad mórbida y sujetos con normopeso, y analiza los cambios en los niveles de resistina después de la pérdida significativa de peso debida a cirugía bariátrica.
Métodos: se seleccionaron 68 pacientes con obesidad mórbida (IMC ≥ 40 kg/m2) y 31 sujetos normopeso (IMC < 25 kg/m2). Las variables del estudio fueron peso, talla, IMC, relación cintura-cadera (WHR), masa grasa, antecedentes familiares de enfermedad cardiovascular, diabetes mellitus tipo 2 (DM), hipertensión arterial, dislipidemia, tabaquismo, glucosa, hemoglobina glicosilada (HbA1c), insulina, proteína C reactiva de alta sensibilidad (hsCRP), interleucina-6 (IL-6), adiponectina y resistina. Se calcularon la evaluación del modelo de homeostasis (HOMA) y el índice cuantitativo de control de sensibilidad a la insulina (QUICKI). Los pacientes obesos se sometieron a un bypass gástrico, y las variables mencionadas fueron reevaluadas después de 12 meses y una pérdida de peso importante.
Resultados: no hubo diferencias significativas en los niveles de resistina entre pacientes obesos mórbidos y sujetos sanos de peso normal, ni entre pacientes obesos antes y después de la pérdida de peso. Los niveles de resistina en pacientes obesos mórbidos no se correlacionaron con medidas antropométricas de adiposidad, insulina, glucosa, HOMA, QUICKI, hsCRP, IL-6 o adiponectina. En el grupo de obesos mórbidos, al año de la pérdida de peso experimentada, el único parámetro del estudio correlacionado con los niveles de resistina fue la IL-6.
Conclusión: nuestros resultados no apoyan una relación entre los niveles de resistina, la obesidad y la resistencia a la insulina en los seres humanos.
Palabras clave: Resistina. Obesidad. Bypass gástrico. Resistencia insulínica.
INTRODUCTION
Resistin was first described in 2001 in rodents. The first investigations suggested that this molecule, which is mainly produced in adipocytes, contributes to insulin resistance in obese rodents (1). In humans, the information available on the relationship among resistin, obesity and insulin resistance is subject to controversy (2). In humans the molecule is not produced mainly in adipocytes but in inflammatory cells such as monocytes and macrophages (3). In this regard, adipose tissue contains abundant macrophages, and these may constitute an important source of resistin in obese subjects (4).
Bariatric surgery is effective in reducing adipose tissue in morbidly obese patients. This significant weight loss in turn is followed by improvement of the inflammatory state (5), and this change could be correlated to the resistin levels.
The present study was carried out to determine whether there are differences in resistin levels between patients with morbid obesity and lean subjects, and to analyze the possible relationship between resistin and insulin resistance in morbidly obese subjects before and after important weight loss secondary to bariatric surgery.
SUBJECTS AND METHODS
A non-randomized, longitudinal, prospective observational study was carried out in the Hospital Universitario Morales Meseguer (Murcia, Spain).
We estimated a sample size of 68 subjects, accepting an alpha risk of 0.05 (α < 0.05) and a beta risk of 20% (β < 20%), assuming a standard deviation (SD) of 7 and a loss to follow-up rate of 2%. We selected 68 consecutive patients with morbid obesity (body mass index [BMI] ≥ 40 mg/kg2) seen in the Endocrinology and Nutrition outpatient clinic. In turn, a control group of 31 healthy lean subjects (BMI < 25 kg/m2) was established. The inclusion criteria for the morbidly obese patients were: BMI ≥ 40 kg/m2, age 18-60 years, failure of hygiene-dietetic measures for weight loss, and failure of medical treatment for obesity. The inclusion criteria for the controls were: BMI 18.5-24.9 kg/m2 and age 18-60 years. The exclusion criteria in both groups were: presence of inflammatory diseases or of infectious, neoplastic or cardiovascular disorders prior to inclusion in the study.
After signing of the informed consent document, all the subjects underwent a general physical examination and venous blood tests. The following variables were recorded: sex, age, weight (kg), height (cm), waist circumference (cm), hip perimeter (cm), fat mass (%), body mass index (kg/m2), WHR (waist-hip ratio [cm]), family history of cardiovascular disease (CVD), type 2 diabetes mellitus (DM), hypertension, dyslipidemia, smoking, glucose (mg/dl), glycated hemoglobin (HbA1c [%]), insulin (mIU/l), homoeostasis model assessment (HOMA: fasting insulin [mIU/l] x fasting glucose [mmol/l]/22.5), quantitative insulin sensitivity check index (QUICKI: 1/log insulin [mIU/l] + log glucose [mg/dl]), high-sensitivity C-reactive protein (hsCRP [mg/l]), interleukin-6 (IL-6 [pg/ml]), adiponectin (µg/ml) and resistin (ng/ml). The blood samples were collected after a fasting period of 12 hours, centrifuged at 3,500 rpm for 15 minutes, and stored at 4 °C. The glucose, HbA1c and insulin levels were determined immediately. The serum samples for the determination of hsCRP, IL-6, adiponectin and resistin were frozen at -80 °C for posterior analysis. Two readings were made of each sample (coefficient of variation [CV] < 6%) except for resistin, and the results were reported as the mean of the two measurements. Glucose concentrations were determined by enzyme methods (Advia 2500 auto-analyzer). The insulin concentration was determined by chemiluminescence (Advia Centaur). An automated high performance liquid chromatograph was used for determining HbA1c, while hsCRP was determined by enzyme-linked immunosorbent assay (ELISA; DRG Diagnostics, Marburg, Germany). Interleukin-6, adiponectin and resistin were also determined by ELISA (Quantikine R&D System, Minneapolis, USA). HOMA and QUICKI were calculated using the above described formulas.
Following the initial evaluation, the 68 patients with morbid obesity were referred to the Department of General Surgery (Hospital Universitario Morales Meseguer) for Roux-en-Y gastric bypass based on the technique described by Capella. Twelve months after surgery and following important weight loss, a total of 68 patients were reassessed.
The quantitative variables were expressed as the mean ± SD. The distribution of the variables was assessed using the Kolmogorov-Smirnov test, though the central limit theorem was assumed. The Student's t-test was used for the comparison of quantitative variables means, while correlations between qualitative variables were assessed by means of the Pearson correlation coefficient (r). All comparisons were two-sided, and statistical significance was considered for p < 0.05. The SPSS version 20 statistical package for Mac was used throughout.
RESULTS
Resistin levels in morbidly obese patients versus lean subjects
Of the 68 patients with morbid obesity finally included in the study, 22 were males (32.4%) and 46 were females (67.6%), with a mean age of 39.57 ± 10.15 years and a BMI of 48.27 ± 7.15 kg/m2; 40.8% had a family history of CVD, 19.1% had DM, 27.9% had hypertension, 25% had dyslipidemia, and 35.3% were smokers. The control group in turn consisted of ten males (32.3%) and 21 females (67.7%), with a mean age of 39.48 ± 8.69 years and a BMI of 22.31 ± 1.96 kg/m2. There were statistically significant differences in BMI, WHR, fat mass, glucose, HbA1c, insulin, HOMA, QUICKI, hsCRP, IL-6 and adiponectin between the morbidly obese patients and the controls. There were no significant differences in the mean resistin levels between the morbidly obese patients and the controls with normal body weight. The mean plasma resistin concentration in the obese patients was 9.42 ± 3.81 ng/ml, versus 9.38 ± 4.24 ng/ml in the control group. The difference between the two groups (0.04 ng/ml; 95% CI: -1.64 to 1.74) was not statistically significant (Table I).
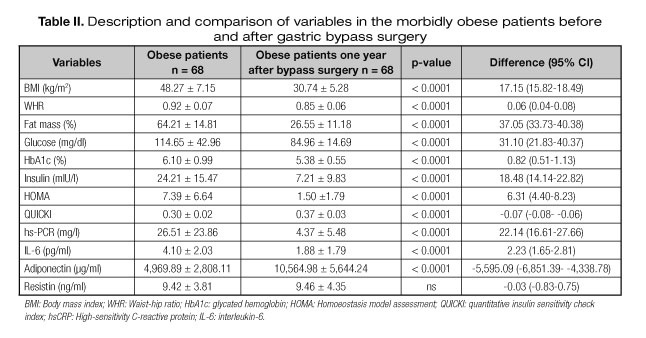
Resistin levels in morbidly obese patients before and after bariatric surgery
One year after gastric bypass surgery with important weight loss, significant reductions were recorded in the anthropometric and adiposity parameters (BMI, WHR, fat mass), as well as in glucose, HbA1c, insulin and HOMA, with a significant increase in QUICKI. Both hsCRP and IL-6 decreased significantly one year after surgery, while the adiponectin levels were seen to increase significantly. The resistin levels showed no significant changes following the experienced weight loss.
There were no significant differences in plasma resistin levels among the morbidly obese patients before and after important weight loss: the mean basal resistin concentration was 9.42 ± 3.81 ng/ml, versus 9.46 ± 4.35 ng/ml one year after bariatric surgery. The observed difference (-0.03 ng/ml; 95% CI: -0.83 to 0.75) was not statistically significant (Table II).
Relationship between resistin and the rest of the variables in morbidly obese patients at baseline and one year after surgery
The resistin levels showed no correlation with the anthropometric or adiposity variables studied either before or after surgery. A weak positive correlation was observed between resistin and HbA1c in the obese patients at baseline (r = 0.271; p = 0.043), though this correlation was lost after weight loss. We found no relationship between resistin and insulin or between resistin and glucose and the HOMA and QUICKI insulin resistance indices, at either baseline or one year after bariatric surgery. Likewise, no correlation was found between resistin and hsCRP, or between resistin and IL-6, in the obese subjects. However, after weight loss, the resistin concentrations were found to be positively correlated to IL-6 (r = 0.291; p = 0.017). Adiponectin was not seen to be correlated to resistin at any time (Table III).
Resistin levels in obese diabetic and non-diabetic patients
Of the 68 patients, 19.1% were obese diabetic and 80.9% were obese non-diabetic patients. The mean plasma resistin concentration was higher in obese diabetic patients than in the rest (10.73 ± 4.24 ng/ml versus 9.18 ± 3.67 ng/ml), although this difference of 1.55 ng/ml (95% CI: 0.78-3.88) was not statistically significant. The resistin levels showed no correlation with the different variables in the group of obese diabetic patients either before or after surgery.
Resistin levels in obese patients with ≥ 2 CVD risk factors
In regard to obese patients, 30.8% had ≥ 2 CVD risk factors and the mean plasma resistin concentration was 10.27 ± 4.68 ng/ml; 69.2% had ≤ 1 CVD risk factors and the mean plasma resistin concentration was 9.14 ± 3.37 ng/ml. The difference was 1.12 (95% CI: 0.90-3.15) and was not statistically significant.
DISCUSSION
Since the first descriptions of resistin in rodents in 2001 (1), this molecule has been regarded as a key linking factor between obesity and insulin resistance, and many authors have attempted to confirm this relationship in both rodents and humans. The human findings are contradictory, some investigators having observed no relationship between plasma resistin levels and either obesity or insulin resistance (2). Studies in obese individuals who have lost weight as a result of dietetic measures or bariatric surgery have yielded inconsistent results. One publication involving morbidly obese patients subjected to bariatric surgery reported a decrease in serum resistin 3-6 months after the operation (6). In contrast, another study recorded a small increase in resistin with weight loss over a shorter period of follow-up (7), and a recent study has found no changes in plasma resistin levels after bariatric surgery, despite significant weight loss (8).
The main findings of our study are that plasma resistin concentration is not increased in morbidly obese individuals, and moreover does not experience changes with weight loss, despite improvement in sensitivity to insulin. We have observed significant differences between morbidly obese patients and lean subjects in terms of the anthropometric and adiposity variables studied, in the parameters related to carbohydrate metabolism and insulin resistance (glucose, HbA1c, insulin, adiponectin, QUICKI and HOMA), and in the inflammatory markers (hsCRP and IL-6). Furthermore, there was significant improvement of all these parameters in the obese subjects following important weight loss. However, the plasma resistin levels were not significantly different between obese patients and lean subjects and, in addition, did not change in obese patients after weight loss. Resistin was not related to the anthropometric variables, fat mass or insulin resistance indices. However, a weak positive correlation was found between resistin and HbA1c in the morbidly obese individuals at baseline. No clear clinical significance was observed, due to the lack of correlation with the rest of the carbohydrate metabolic and insulin resistance parameters. Our results support the opinion of many authors that resistin is not related to either obesity or insulin resistance in humans (2), and that, consequently, the levels of this molecule do not differ between obese and lean individuals, and remain without variations despite the improved sensitivity to insulin observed after weight loss secondary to bariatric surgery (8).
The discrepant results regarding the physiopathological role of resistin in humans and rodents could be explained by the fact that monocytes and macrophages constitute the main source of resistin in humans, while in rodents resistin is produced by adipocytes (1). In humans, only a small amount of resistin is produced by adipocytes, since resistin mRNA expression in human adipose tissue is only 1/20 of that observed in rodents (3). Resistin genic expression regulation studies can also help explain some of the contradictory findings in humans. Several studies have demonstrated an association between single nucleotide polymorphisms (SNPs) of the resistin RETN gene and resistin levels in humans. Several SNPs have been shown to be associated to high resistin levels, and up to two-thirds of the variations in plasma resistin concentration may be attributable to genetic factors (9). Therefore, resistin expression appears to be partially controlled by genetic programming at genotype level. These data point to the existence of several potential genetic modulators of resistin expression, with strong evidence of variants in the promoter region of the human resistin gene. However, such genetic signals have not been consistently correlated to resistin. Polymorphisms -638 G > A, -420 C > G and -358 G > A in the promoter region of the human resistin gene (RETN) have been found to be associated to resistin levels in Asian populations (10), though the data in Caucasians are contradictory.
The results of our study are solid, since they come from a longitudinal prospective study with one year of follow-up and a control group. The study has some limitations, however. Firstly, the study population was limited to Caucasian individuals; ethnic differences therefore may preclude generalization of the results obtained. Secondly, plasma resistin measurement was made on a point basis; as a result, the values might not be representative, due to possible circadian variations in the plasma levels of the molecule.
In conclusion, plasma resistin levels are not a key factor linking obesity to insulin resistance.
REFERENCES
1. Steppan CM, Bailey ST, Bhat S, Brown EJ, Banerjee RR, Wright CM, et al. The hormone resistin links obesity to diabetes. Nature 2001;409:307-12.
2. Lee JH, Chan JL, Yiannakouris N, Kontogianni M, Estrada E, Seip R, et al. Circulating resistin levels are not associated with obesity or insulin resistance in humans and are not regulated by fasting or leptin administration: Cross-sectional and interventional studies in normal, insulin-resistant, and diabetic subjects. J Clin Endocrinol Metab 2003;88:4848-56.
3. Patel L, Buckels AC, Kinghorn IJ, Murdock PR, Holbrook JD, Plumpton C, et al. Resistin is expressed in human macrophages and directly regulated by PPAR gamma activators. Biochem Biophys Res Commun 2003;300:472-6.
4. Curat CA, Wegner V, Sengenes C, Miranville A, Tonus C, Busse R, et al. Macrophages in human visceral adipose tissue: Increased accumulation in obesity and a source of resistin and visfatin. Diabetologia 2006;49:744-7.
5. Illán Gómez F, Gonzálvez Ortega M, Orea Soler I, Alcaraz Tafalla MS, Aragón Alonso A, Pascual Díaz M, et al. Obesity and inflammation: Change in adiponectin, C-reactive protein, tumour necrosis factor-alpha and interleukin-6 after bariatric surgery. Obes Surg 2012;22(6):950-5.
6. Vendrell J, Broch M, Vilarrasa N, Molina A, Gómez JM, Gutiérrez C, et al. Resistin, adiponectin, ghrelin, leptin, and proinflammatory cytokines: Relationships in obesity. Obes Res 2004;12:962-71.
p>7. Edwards C, Hindle AK, Fu S, Brody F. Downregulation of leptin and resistin expression in blood following bariatric surgery. Surg Endosc 2011:25(6):1962-8. p>8. De Luis DA, Terroba MC, Cuéllar L, Conde R, Primo D, Aller R, et al. Resistin levels in morbid obese patients following the biliopancreatic diversion surgery. Horm Metab Res 2011;43(3):205-8.9. Menzaghi C, Coco A, Salvemini L, Thompson R, De Cosmo S, Doria A, et al. Heritability of serum resistin and its genetic correlation with insulin resistance-related features in nondiabetic Caucasians. J Clin Endocrinol Metab 2006;91:2792-5.
10. Azuma K, Oguchi S, Matsubara Y, Mamizuka T, Murata M, Kikuchi H, et al. Novel resistin promoter polymorphisms: Association with serum resistin level in Japanese obese individuals. Horm Metab Res 2004;36:564-70.
 Correspondence:
Correspondence:
Elena Parreño Caparrós.
Department of Endocrinology and Nutrition.
Hospital de la Vega Lorenzo Guirao.
Ctra. de Abarán, s/n.
30530 Cieza, Murcia. Spain
e-mail: elenapcnet@yahoo.es
Received: 11/02/2017
Accepted: 17/05/2017