INTRODUCTION
Childhood malnutrition is a major public health problem among children in developing countries. It can affect physical and intellectual growth and is also considered as the main cause of child morbidity and mortality.
High degrees of malnutrition have been reported in our country 1. The rate of stunting, underweight, and wasting were 9.53, 9.66 and 8.19%, respectively 2. In another study from Spain, the rate of malnutrition at the moment of hospitalization was 8.2 3. In a Brazilian study, 16.3% of children under five years of age presented malnutrition at admission 4. Most of this studies were carried out in apparently healthy school children. There are little published studies about nutritional assessment at hospital admission. The aim of this study is to evaluate the frequency of obesity and malnutrition among hospitalized children with no past medical history at the moment of hospital admission.
METHODS
This is a prospective, cross-sectional and observational study which was conducted for the assessment of children nutritional status. The study sample included 430 patients: 225 boys (56%) and 175 girls (44%), with a mean age of 5.39 (SEM 0.32) years for boys and 5.78 (SEM 0.38) years for girls. All subjects were hospitalized consecutively in the Pediatric Emergency Department of the Nemazee Teaching Hospital of the Shiraz University of Medical Sciences (Shiraz, Islamic Republic of Iran).
All children with evidence or history of chronic diseases such as liver cirrhosis, microcephaly, macrocephaly due to congenital infection or abnormal skull shape, and patients with muscular or neurological problems, with prolonged steroid usage, nephrotic syndrome, cardiac problems, and protein loosing enteropathy were excluded from the study. The duration of the study was six months starting from January 2016.
Parents or caregivers were informed about the aims of the study and verbal consent was obtained to take their children anthropometric measurements.
The instruments needed were a structured questionnaire and anthropometric measuring tools such as digital scale for weight with 0.1 kg accuracy and measuring tape with a 0.1 cm accuracy. The questionnaire included child age, sex, birth weight, height and head circumference (recorded from the child birth report card), which was completed by interviewing mothers or child caregivers.
Other required data were recorded through measuring height, weight, head circumference, and MUAC.
MEASURING WEIGHT
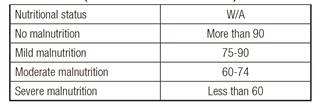
The child was weighed on a digital scale according to the standard way for the weight measurement. Evaluation of wasting was done according to the following formula: W/A: W/A: [observed weight/median weight (same age and sex)] x 100.
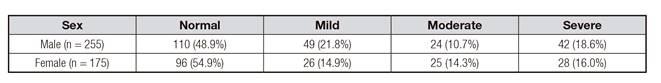
Classification of wasting was done as shown in Table I.
MEASURING LENGTH
The height of children aged < 2 years was measured in supine position (top of the head to the bottom of the heel), and the rest of children were measured in standing position, with an accuracy of 0.10 cm.
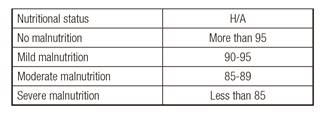
Height measurement was taken on the flat floor and against a wall (flat surface). The measuring tape was placed 50 cm above the floor (and recorded height was gathered with that). The children stood with their feet flat, together, and against the wall. Legs were straight, arms were at sides, and shoulders were level. The child looked straight ahead, with the line of the sight parallel with the floor. Height was evaluated according to the following formula: H/A: [observed height/median height (same age and sex)] x 100.
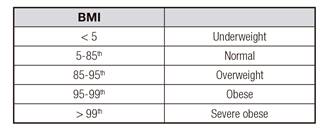
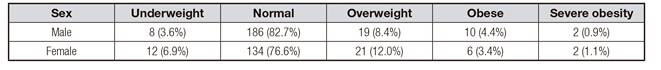
Stunting was classified as shown in Table II and the classification of body mass index is shown in Table III.
MEASURING MUAC
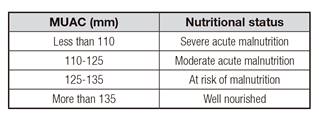
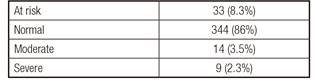
First, the child's arms were relaxed and hanged down the sides of the body. The tip of the left shoulder (acromion) and the tip of the left elbow (olecranon) were located, and midpoint was marked. Then, the position of the tape was corrected for measuring arm circumference while ensuring that the tape neither pinched the arm nor was loose. Severity of malnutrition was calculated according to Table IV.
MUAC has a high specificity and appears to be better predictor of childhood mortality than weight for height 5) (6.
Gomez and Waterlow classifications were used for evaluation of weight for age and height for age ratio. World Health Organization (WHO) growth charts were used for weight, height, and BMI evaluation. Overweight, obesity, and severe obesity were defined according to BMI 85-95%, 95-99% and > 99%, respectively (Table III).
STATISTICAL ANALYSIS
Statistical analysis was performed with SPSS, version 16 (Chicago, IL, USA). Continuous variables were performed as mean and standard error of mean (SEM), while categorical variables were presented as number and percentage. The Chi-squared test was used to compare differences in categorical variables and the independent t test for continuous variables between boys and girls. p value less than 0.05 was considered to be statistically significant.
RESULTS
The study sample included 430 patients: 225 boys (56%) and 175 girls (44%), with a mean age of 5.39 (SEM 0.32) for boys and 5.78 (SEM 0.38) for girls. Our patients were placed in four categories according to age: < 2 years (n = 124), 2-5 years (n = 120), 6-10 years (n = 78), and > 10 years (n = 78).
According to W/A data (current weight/ideal weight), 188 (47%) of the patients studied were malnourished: 118 (29.5%) presented mild malnutrition; 54 (13.5%), moderate; and 16 (4%), severe (Table V).
Table V Malnutrition among children admitted to the hospital according to W/A ratio (Gómez classification)
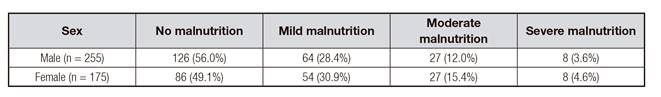
According to H/A data (current height/ideal height), 194 (48.5%) of the patients studied were stunted, 75 (18.8%) were mild, 49 (12.3%) were moderate, and 70 (17.5%) were severe (Table VI).
According to BMI, 40 (10%) patients from the sample were overweight, four (16%) were obese, and four (1%) were severe obese (Table VII). Regarding MUAC, 56 (14%) of the patients studied were malnourished, 33 (8.3%) were at risk, 14 (3.5%) presented moderate malnutrition, and nine (2.3%) were severely malnourished (Table VIII).
DISCUSSION AND CONCLUSION
In our study, we found that 47% of patients were underweight (low weight for age), 48.5% were stunted (low height for age), and 14% were malnourished according to MUAC. In the study by Moreno Vilares et al. 7, prevalence of malnutrition was 7.1% for moderate and 0.7% for severe malnutrition, which is significantly lower than that of the current study. In the study by Durá Travé et al., prevalence of malnutrition at the moment of hospitalization was 8.2%, which was lower than in our study 8. In their study, children with congenital malformations were included. In our study, children with chronic disease or abnormal skull shape were excluded. In the study by Lee and Ahmad 9, the prevalence rates of acute and chronic undernutrition were 11% and 14% respectively, that is, lower than in our study. In another study from Brazil, the prevalence of malnutrition was 10%, 185%, 21% and 14.7% according to weight for height, weight for age, height for age and BMI, respectively 10. In this study, children with Down syndrome and children with bone deformity were excluded 10. Consistent with our study, Mahdavi et al., in a study carried out in Tabriz (Iran) covering 140 patients aged 2-12 years, found chronic malnutrition in 30.7% of cases according to H/A, and acute malnutrition in 48.6% of cases according to W/A results 11. In a study conducted in Turkey including 528 patients with a mean age of 5.8 years, Dogan et al. found chronic malnutrition in 27% of cases according to H/A and acute malnutrition in 52.4% of cases according to W/A 12. In another study which was done by Veghari and Vakili, the rate of underweight and stunting was estimated to be 3.20% and 4.93%, respectively 13. A study done by Nouri Saelidou et al. on children under five years in Azerbaijan, Iran, indicated that the rate of underweight and stunting was 2.3% and 7.3%, respectively 14. In another study, prevalence of underweight among Iranian children according to CDC percentiles was 13.9% 15. In the study by Moeeny et al., malnutrition was present in 25.2% of inpatient children 16.
In another study from Turkey, according to the Gomez classification, malnutrition was present in 46.8% of the cases 17. In this study, patients with recurrent hospitalizations, neurological sequelae, and neonates were excluded; these exclusion criteria are similar to those of the current study. In the study by Ogunlesi et al., carried out in Nigeria, 18.3% of children had severe acute malnutrition according the Wellcome classification 18.
In the current study, 10% of the cases were overweight, 4% obese, and 1% were severe obese. In the study by Veghari and Vakili, prevalence of overweight was 3.3-5.2% between 1998 and 2013 13. In a study from Iran, prevalence of overweight was 10.4% 19. In line with our study, a study was done in Azerbaijan by Nouri et al. where the prevalence of obesity and overweight was 1.3% and 5.1%, respectively 14. In a multicenter study from Spain 20, overweight and obesity were seen in 37.9% of children, which is significantly higher than the percentage observed in the current study.
According to MUAC, 2.3% of the patients studied had severe malnutrition, 3.5% had moderate malnutrition and 8.3% were at risk of malnutrition. There are some differences between the results of these studies. These differences may be due to the different criteria which were used for the definition of malnutrition. In the current study, all children with a history of chronic disease or malformations were excluded. But in the study by Durá Travé et al., patients with congenital malformations were included 8.
CONCLUSION
In conclusion, our study demonstrates that the frequency of malnutrition among hospitalized children is relatively high. This higher prevalence of malnutrition needs more consideration because malnutrition has adverse effect on the outcome of the patients admitted in hospital.
The main limitation of the study was that it is a single center study.