INTRODUCTION
Limiting egg consumption to avoid dyslipidemia has been customarily recommended, to reduce the risk of cardiovascular disease (CVD) 1. However, dietary cholesterol is known to have only a limited influence on total serum cholesterol and in low-density lipoprotein cholesterol (LDL-c) levels. Moreover, increasing egg consumption has been associated with beneficial moderate elevations in high-density lipoprotein cholesterol (HDL-c) 2 and even sometimes with beneficial overall serum lipid profiles when the size and number of lipoprotein particles were also taken into account 3) (5. Available meta-analyses do not find any association between egg consumption and the risk of CVD 2) (6) (7. Almost all previous guidelines recommended that cholesterol intake should be limited to no more than 300 mg/day, but the more recent and comprehensive evidence showed no demonstrable harms associated to egg consumption or to a greater dietary cholesterol intake 2) (6) (7) (8. It is widely assumed that dietary "cholesterol is not considered a nutrient of concern for overconsumption" 9. However, this conclusion has raised some debate 10 given that eggs are one of the major sources of dietary cholesterol, one unit (60 g) provides approximately 230 mg of cholesterol. Hence, the effect of egg consumption on serum lipid levels remains controversial 2) (8) (11) (12) (13, particularly on serum levels of total cholesterol and LDL-c. Some studies relating egg consumption to lipid levels used extreme and unrealistic categories of exposure, or classified subjects at post-hoc in subgroups according to whether or not they were "responders" 8. Most studies did not take into account the effect of ethnicity, dietary confounders and nutritional effect modifiers. Interestingly, some aspects of the overall dietary pattern may differentially affect the serum lipid response to egg consumption 14 and this response has shown marked between-subject variation and between-study heterogeneity 2 which is likely to depend, at least partially, on the overall diet. In this context, studies on different ethnic groups are important. The Mediterranean diet has been proposed by the Dietary Guidelines Advisory Committee as a healthy dietary pattern with strong and robust evidence of protection and its global use is currently on the rise 15. It is therefore interesting to assess the lipid responses to egg consumption in cohorts of free-living subjects who live in Mediterranean areas. We evaluated the association between the frequency of egg consumption and the incidence of hypercholesterolemia, low levels of HDL-c or high values of triglycerides in a large cohort of Spanish university graduates, the SUN (Seguimiento Universidad de Navarra) cohort.
METHODS
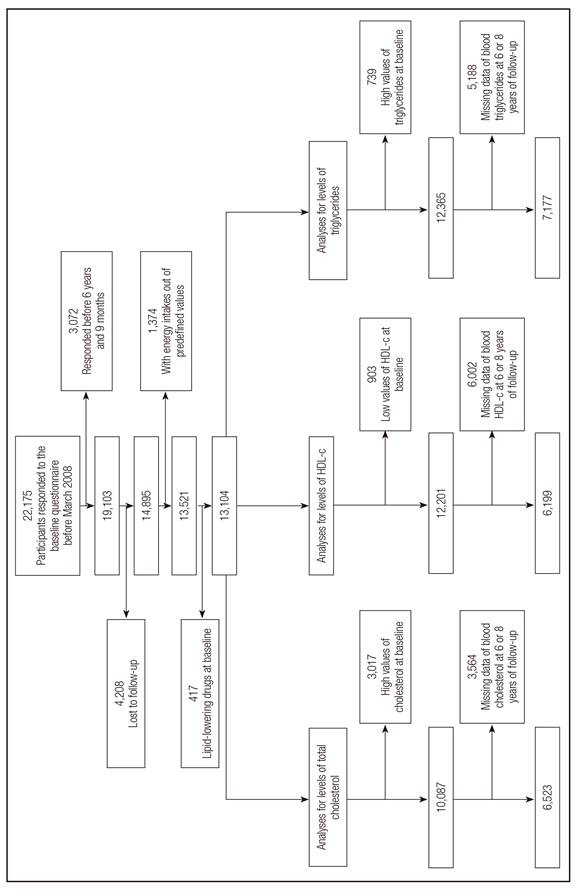
The SUN project is a prospective and dynamic cohort. The design, objectives and methods have been previously published 16) (17. More than 50% of participants in the SUN cohort are health professionals themselves. The recruitment started in December 1999 and it is permanently open (dynamic design). The answer of the first questionnaire is considered as provision of informed consent. Sociodemographic variables, lifestyles and medically-diagnosed diseases were collected through a baseline questionnaire at the time of recruitment. The protocol for the SUN cohort was approved by the Institutional Review Board at the University of Navarra. We inquired about serum total cholesterol levels and about the criteria for metabolic syndrome (MetS), including HDL-c, TG and fasting blood glucose levels, in the 6-year and 8-year follow-up questionnaires. This self-reported information provided by highly educated participants has previously been validated 18) (19. We also inquired about new medical diagnoses of hypercholesterolemia in all follow-up questionnaires (after 2, 4, 6, 8, 10, 12 and 14-year follow-up). We considered the follow-up time as the period between recruitment (reception of the baseline questionnaire) and the date of the last follow-up questionnaire, the date of a new diagnosis of hypercholesterolemia or death, whichever came first. From a total of 22,175 participants in the SUN cohort (Fig. 1), we excluded those participants with less than 6 years and 9 months of follow up (n = 3,072), and those who were lost to follow up or had missing values in the variables of interest (n = 4,208). We also excluded participants taking lipid-lowering drugs at the time of inclusion in the study (n = 417) and those who were outside pre-defined values for total energy intake (< 800 or > 4,000 kcal/day for men and < 500 or > 3,500 kcal/day for women) (n = 1374) 20. The 13,104 remaining participants were available for different analyses. For the assessment of the association between egg consumption and follow-up values of total blood cholesterol, we excluded participants with baseline values of total blood cholesterol above 200 mg/dl (n= 3,017) and those who did not report their total blood cholesterol data at 6 or 8 years of follow up (n= 3,564). Therefore, we included in this analysis 6,523 participants without baseline hypercholesterolemia and with available data for blood total cholesterol at follow-up. To assess the association between egg consumption and HDL-c levels, we excluded participants with prevalent low levels of HDL-c, below 40 mg/dl in men or below 50 mg/dl in women (n = 903) and those who had been in the cohort for less than 6 years (they could not provide lipid values at 6 or 8 years of follow-up) or did not report their levels of HDL-c at 6 or 8 years of follow-up (n = 6,002). The available subsample for the analysis on HDL-c was 6,199 participants. Finally, to study the prospective association between egg consumption and incidence of hypertriglyceridemia we excluded from the initial sample (13,104 participants), participants with triglycerides levels above 150 mg/dl at baseline (n= 739) and those who did not report their data of triglycerides blood levels at 6 or 8 years (n = 5,188). The final subsample for assessing the association between egg consumption and hypertriglyceridemia was 7,177.
DIETARY ASSESSMENT
Baseline egg consumption was assessed with a semi-quantitative 136-item food frequency questionnaire repeatedly validated in Spain 21) (22. The amount of egg contained in other products (pastries or sauces) was not considered and the method for the culinary preparation of eggs was not taken into account. Response options were nine categories: from never or almost never to more than six times a day. We assigned the value 0 egg consumption to participants with missing values in the corresponding item of the food frequency questionnaire (77 for total cholesterol analysis, 71 for HDL-c analysis and 86 for triglycerides analysis). Nutrient intake was calculated and trained dietitians updated the data bank using the latest Spanish food composition tables 23) (24.
EXPOSURE ASSESSMENT AND OTHER VARIABLES
The initial questionnaire included questions on medical history and conditions including dyslipidemia, family history of cardiovascular disease, prevalent diagnoses of hypertension or diabetes, lifestyles (smoking habits, physical activity and alcohol consumption) and sociodemographic variables. Participants were classified according to their smoking habits as never smokers, current smokers and former smokers. In addition, physical activity was assessed at baseline with a validated 17-item questionnaire 25. The index of metabolic equivalent task hours per week (METs-h/week) was computed by using the time spent engaging in 17 activities and multiplying the time spent by the resting metabolic rate (MET-score) specific for each activity. The METs-h/week for all activities were combined to obtain a value of total METs-h/week 26. The validity of self-reported weight, BMI, leisure time physical activity and hypertension in the SUN cohort was assessed in specific validation studies 25) (27) (28. Adherence to the Mediterranean diet was defined according to the 9-item score proposed by Trichopoulou et al. 29.
ASSESSMENT OF INCIDENT HYPERCHOLESTEROLEMIA, HYPERTRIGLYCERIDEMIA OR LOW LEVELS OF HDL-C
The baseline questionnaire included a question on whether the participant had previously received a medical diagnosis of hypercholesterolemia (≥ 240 mg/dl) 30 or hypertriglyceridemia (triglycerides ≥ 150 mg/dl) and the age of these diagnoses. Baseline HDL-c levels also were self-reported in a period of less than 5 years previous to the baseline questionnaire. Information on the concentrations of total serum cholesterol, triglycerides and HDL-c was collected at 6 and 8 years of follow-up. Participants reported their results obtained from their blood test and medical check-ups that they routinely undergo in Spain at no cost using the clinical services of the National Health System or from their Occupational medical services. Information about LDL-c also was collected in the 6- and 8-year follow-up questionnaires, but participants were not asked at baseline about their blood concentrations of LDL-c, therefore we could not exclude those who were prevalent cases at baseline, and due to this reason we did not include in this work any analysis relating egg consumption to serum levels of LDL-c. We assumed that participants had elevated baseline cholesterol (prevalent hypercholesterolemia) if they reported having been diagnosed of hypercholesterolemia by a medical doctor or if they were under usual treatment with lipid-lowering drugs. Incident cases of hypercholesterolemia were defined as those participants without any baseline diagnosis of hypercholesterolemia and without any treatment with lipid-lowering drugs at baseline who subsequently reported a medical diagnosis of high blood cholesterol during follow-up.
STATISTICAL ANALYSIS
We divided participants according to their usual egg consumption in four categories: < 1 egg/week; 1 egg/week; 2-4 eggs/week and > 4 eggs/week. Odds ratios (OR) and 95% confidence intervals (CI) for incident hypercholesterolemia were estimated for the three upper categories of egg consumption using multivariate logistic regression models adjusted for potential confounders. The lowest category of egg consumption was considered as the reference category. We adjusted for the following confounding factors: age (continuous), sex, total energy intake (continuous), quartiles of body mass index (BMI), smoking (never smoker, former smoker and current smoker), physical activity during leisure time (METs-hours/week, continuous), adherence to the Mediterranean dietary pattern (continuous), alcohol intake (continuous), family history of CVD (yes/no), diabetes at baseline (yes/no) and prevalent hypertension (yes/no). Multiple linear regression models were used to evaluate the multivariable-adjusted differences in total cholesterol, HDL-c and triglycerides between each of the 3 upper categories of egg consumption and the lowest category, adjusting for the previously mentioned potential confounding factors. For triglycerides blood concentrations analyses we additionally adjusted for carbohydrate intake as an independent covariate in the regression models. The analyses were run with Stata software version 12 (Stata Corp). Statistical significance was set at the conventional cut-off of p < 0.05.
RESULTS
Baseline characteristics of participants according to their baseline categories of egg consumption in the subsample of total cholesterol analysis are presented in Table I. The mean age of participants was 38.4 years (range 20-89) and their median egg consumption was 2.79 eggs/week. Table II shows the ORs for the association between baseline categories of egg consumption and the diagnosis of high levels of total blood cholesterol, low concentrations of HDL-c or high concentrations of triglycerides during follow-up (either at 6 or 8 years of follow up). We classified also as cases of incident hypercholesterolemia those participants who reported values of total cholesterol above 240 mg/dl in the 6-year or 8-year follow-up questionnaire. We observed an inverse association between egg consumption and high blood cholesterol in the crude model with a significant linear trend (p = 0.03). The comparison between extreme categories also showed, but only in the crude model, a significant inverse association (OR: 0.71; 95% CI: 0.52 to 0.96, p < 0.05). However, when we adjusted for age, sex and total energy intake, the inverse association weakened and the statistical significance was lost.
Table I Baseline characteristics of participants of the SUN cohort classified according to categories of egg consumption in the subsample of total cholesterol analyses (n = 6,523)*

*Baseline characteristics of participants are presented as means ± SDs for quantitative variables and as n (%) for categorical variables.
Table II Odds Ratios (ORs) for incidence of high total cholesterol levels (TC), low high-density lipoproteins (HDL-c) levels and high triglycerides (TG) levels according to categories of egg consumption in the SUN cohort at 6 and 8 years of follow-up

*p < 0.05; **p < 0. 01.
Multivariable 1: adjusted for age (continuous), sex and total energy intake (continuous).
Multivariable 2: additionally adjusted for quartiles of body mass index (continuous), smoking status, hypertension at baseline, family history of cardiovascular disease, diabetes at baseline, physical activity during leisure time (continuous), adherence to the Mediterranean food pattern (continuous) and alcohol intake (continuous).
Multivariable 3: additionally adjusted for carbohydrate intake.
Neither the observed ORs for each of the 3 upper categories, nor the linear trend tests showed any significant association between egg consumption and a medical diagnosis of low HDL-c. For the association between egg consumption and the incidence of hypertriglyceridemia (values of blood levels of triglycerides > 150 ml/dl) we observed a significant inverse association only for intermediate levels of egg consumption (2 to 4 eggs/week vs. less than 1 egg/week) with OR: 0.71 (95% CI: 0.54 to 0.93, p < 0.05) in the multivariable-adjusted model. We additionally adjusted for carbohydrate intake (g/day) and we observed similar results (OR: 0.71; 95% CI: 0.54 to 0.94, p < 0.05). However we did not observe any statistically significant linear trend relating higher egg consumption to lower risk of hypertriglyceridemia.
We also treated the lipid levels as continuous variables and applied multiple linear regression models. Table III and Table IV show the regression coefficients that represent the adjusted differences in mean levels of lipids between each of the three upper categories of egg consumption versus the lowest category (< 1 egg/week) which was always the reference category. Table III presents differences in means after 6-years of follow-up and Table IV, after 8-years of follow-up. For average total cholesterol we observed small and non-significant differences between groups of egg consumption. Only in the crude model, higher egg consumption was associated with lower means of HDL-c blood levels (p for trend = 0.004).
Table III Multivariable-adjusted differences of blood concentrations of total cholesterol (TC), high-density lipoproteins (HDL-c) and triglycerides (TG) according to categories of egg consumption in the SUN cohort at 6 years of follow-up

*p < 0.05; **p < 0.01.
Multivariable 1: adjusted for age (continuous), sex and total energy intake (continuous).
Multivariable 2: additionally adjusted for quartiles of body mass index (continuous), smoking status, hypertension at baseline, family history of cardiovascular disease, physical activity during leisure time (continuous), adherence to the Mediterranean food pattern (continuous) and alcohol intake (continuous).
Multivariable 3: additionally adjusted for carbohydrate intake.
Table IV Multivariable-adjusted differences of blood concentrations of total cholesterol (TC), high-density lipoproteins-(HDL) and triglycerides (TG) according to categories of egg consumption in the SUN cohort at 8 years of follow-up
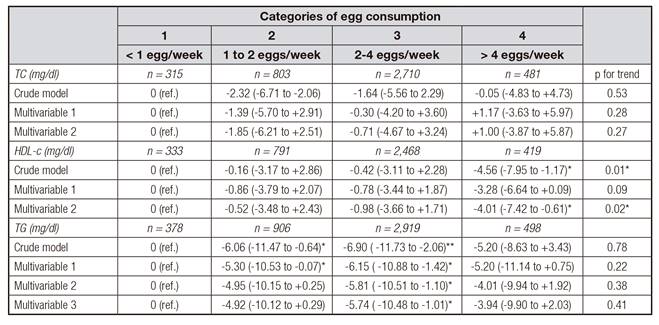
*p < 0.05; **p < 0.01.
Multivariable 1: adjusted for age (continuous), sex and total energy intake (continuous).
Multivariable 2: additionally adjusted for quartiles of body mass index (continuous), smoking status, hypertension at baseline, family history of cardiovascular disease, physical activity during leisure time (continuous), adherence to the Mediterranean food pattern (continuous) and alcohol intake (continuous).
Multivariable 3: additionally adjusted for carbohydrate intake.
When we repeated this assessment using HDL-c values after 8-years of follow-up we did find an association between egg consumption and lower HDL-c levels (p for trend = 0.02) with a fully adjusted difference of -4.01 (-7.42 to -0.61) mg/dl in HDL-c between extreme categories of egg consumption (> 4 vs. < 1 egg/week). Results for blood levels of triglycerides showed lower means of triglycerides in each of the three upper categories of egg consumption than in the lowest category (< 1 egg/week). Results were statistically significant for all comparisons after 6-year follow-up and for many of them after 8-year follow-up. However, the linear trend test was never significant in the follow-up after 8-years (Table IV), it lost its statistical significance in the fully-adjusted model after 6 years (Table III) and the point estimates suggested a plateau effect instead of a monotonically decreasing trend. As sensitivity analyses we fitted logistic regression and multiple linear regression models after adjusting for BMI as a continuous variable instead of quartiles of BMI and we observed similar results (data not shown). We did not observe any significant interaction between egg consumption and adherence to the Mediterranean dietary pattern (cut-off ≥ 6 vs. < 6 in the 9-item Trichopoulou score) 31.
DISCUSSION
This longitudinal study did not identify any clear harmful association between egg consumption and the incidence of hypercholesterolemia or hypertriglyceridemia in a prospective cohort of highly educated Mediterranean subjects. We did observe an inverse association between egg consumption and mean serum HDL-c levels with a decreasing linear trend that was statistically significant only after 8 years of follow-up. Lower average concentrations of HDL-c were observed in subjects who consumed more than 4 eggs/week after adjusting for a wide array of potential confounders. However, the size of the difference was small and probably it was not clinically relevant, because we did not observe any increased risk of a new diagnosis of low HDL levels (considered as a clinically relevant dichotomous outcome). On the other hand, we found a reduction in the incidence of medically-diagnosed hypertriglyceridemia and lower average levels of triglycerides in subjects who had higher egg consumption. Due to the fact that egg is the major source of dietary cholesterol, metabolic studies have focused on the effect of dietary cholesterol contained in eggs on serum lipids but their influences on plasma concentrations of serum cholesterol the effect is quite small 32) (33. Thus, it seems more appropriate to recommend healthy dietary habits and active lifestyle instead of recommendations focused on the restriction of dietary cholesterol from eggs. In this same cohort we found no association between egg consumption and the incidence of CVD among 14,185 university graduates 34. Furthermore, in a prospective cohort study of 21,327 participants from the Physicians' Health Study, the consumption of ≥ 6 eggs/week had no major effect on the risk of CVD and mortality and the consumption of ≥ 7 eggs/week was associated with a modestly greater risk of total mortality 35) (36) (37. Other studies with experimental designs 4 reported that daily whole egg consumption during moderate carbohydrate restriction diets were associated with greater increases in plasma HDL-c and improvements in HDL-c profiles in patients with the MetS 38) (38) (39) (40. Therefore, our unexpected result of an inverse association with HDL-c in some analyses (only present after 8 years), should be viewed with caution, because it is not consistent with previously reported results and with our analyses after 6 years. Approximately one third of individuals tend to have a high plasma response to dietary cholesterol (hyper-responders). The increases in LDL-c and HDL-c due to increased egg consumption in hyper-responders are not likely to be related to an increased number of LDL or HDL-c particles but, to an increase in the less atherogenic lipoprotein subfractions. These data suggested that additional dietary cholesterol did not increase the risk of developing an atherogenic lipoprotein profile in healthy men, regardless of their response classification.
The most apparent potential limitation of our study is the self-report nature of lipid levels, but these self-reported values were previously validated in specific studies conducted in sub-samples of the SUN cohort 18) (19. A second potential concern may be related to the generalizability of our findings which are based on a young cohort of university graduates that is a non-representative sample of the general population. On the other hand, their high educational level ensures a more accurate response. In addition, egg consumption might be underestimated because FFQs inquired about units of egg consumed and the amount of eggs contained in other products (pastries or sauces), were not considered. In addition, we only assessed egg consumption at baseline. However, several important strengths are the prospective design and large sample size of our study, our long-term follow-up, a high retention rate (81.5%), the ability to control for a wide array of potential confounders, the robustness of our results in sensitivity analyses and the existence of published validation studies for self-reported measurements, including dietary assessment 18) (21) (22) (25) (27) (28.
Our data do not support that higher egg consumption is associated with abnormal blood levels of total cholesterol or triglycerides; however, an inverse association with HDL-c as a quantitative variable was found in only one of our assessments and future studies are warranted to confirm this result. Results from the SUN cohort do not provide any evidence to recommend a reduction in egg consumption in healthy subjects as a means to reduce lipid levels.