INTRODUCTION
Bariatric surgery is performed to control body weight in individuals with class III and II obesity with associated diseases 1. It can generate benefits in the quality of life and it can significantly promote fertility in women with normalization of hormonal concentrations and menstrual cycle, thus facilitating pregnancy 2,3,4.
Among the existing surgical procedures, the most performed worldwide is the Roux-en-Y gastric bypass (RYGB) that accounts for 45% of surgeries 5. In Brazil, the choice for RYGB is even more expressive, accounting for 70% of surgeries 5. Despite the weight loss and improvement of the factors associated with obesity, metabolic disorders deriving from the surgical procedure can cause deficiencies 6,7 of macro and micronutrients 8, including vitamin A deficiency (VAD) 9.
VAD is considered a serious public health problem that affects 19 million of pregnant women in the world and can contribute to increased maternal and infant mortality rates 9. Furthermore, there are specific recommendations about the need of assessing the nutritional status of vitamin A during the prenatal care period 10.
Thus, the objective of the present study is to assess the inadequacy of the nutritional status of vitamin A caused by pregnancy, by RYGB, or by the occurrence of both pregnancy and RYGB concomitantly, as well as the impact of this vitamin deficiency on the mother and child health under the conditions addressed by the study.
METHODS
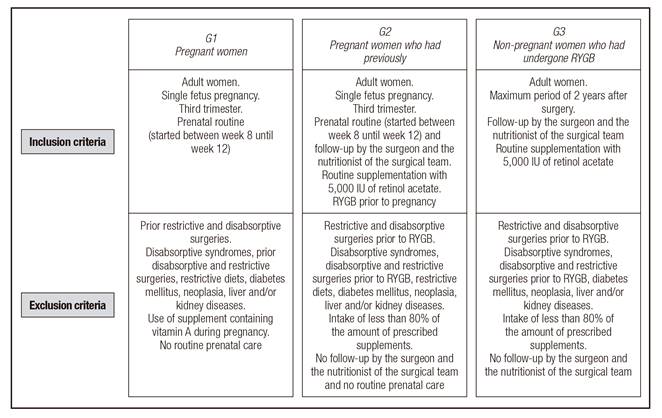
This is a retrospective analytical cross-sectional study conducted with adult women of reproductive age. Pairing by age and presurgery body mass index (BMI) was used for the women who had previously undergone RYGB, and pairing by age and prepregnancy BMI was used for pregnant women. The study was conducted in healthcare institutions located in the city of Rio de Janeiro from January 2011 to December 2012. The women who met the study inclusion criteria were divided into three groups (G1, G2 and G3), as described in Figure 1.
All participants read and signed an informed consent, in accordance with Resolution n.º 196 of 10/10/1996 of the National Council of Health. The study was approved by the Research Ethics Committee of Hospital Universitário Clementino Fraga Filho of the Federal University of Rio de Janeiro.
For the anthropometric assessment of G1 and G2, data were collected on height, prepregnancy weight informed or measured until pregnancy week 13, prepartum weight or weight recorded in the last prenatal visit, besides presurgery weight in G2. With respect to measures obtained in G3, data were collected on height and weight (presurgery and maximum of 2 years after surgery). In all groups, these variables were used to calculate BMI for their subsequent classification, according to the cut-off points established by the World Health Organization (WHO) (1998) 11.
In pregnant women, the other data collected were used to calculate the total gestational weight gain (TGWG) through subtraction of prepregnancy weight from prepartum weight. The adequacy of gestational weight gain was classified in accordance with the Institute of Medicine recommendation (2009) that considers a 5-9 kg weight increase appropriate and a weight increase below or above these values inappropriate 12.
For the anthropometric assessment of newborns, information on weight, height, and gestational age at birth (GAB) was selected. For classification of birth weight, the criteria of the Ministry of Health (2005) were used: low birth weight (less than 2,500 g), insufficient weight (between 2,500 and 2,999 g), appropriate weight (between 3,000 g and 3,999 g), and overweight or macrosomia (4,000 g or more) 13.
As for GAB, were considered born preterm the newborns with GAB < 37 weeks, at term those born between 37 and 42 weeks, and post-term those born with GAB ≥ 42 weeks, according to the date of the last menstrual period (DLMP) 13. Based on the information on weight and GAB, the correlation of weight/GAB was assessed according to the growth curve proposed by Pedreira et al. (2011), and the newborns were classified into small for gestational age (SGA < P10), appropriate for gestational age (AGA, P10-P90), and large for gestational age (LGA > P90) 14.
The referred information was used for assessment of neonatal intercurrences, and the newborn was classified into low weight, appropriate weight, and macrosomic according to birth weight, and into preterm, at term, or post-term according to GAB.
Information about the maternal intercurrences developed during pregnancy was collected through consultations of medical records, maternity cards, and interpretation of laboratory tests.
The following pregnancy intercurrences were: presence of hypertensive syndromes of pregnancy (HSP), anemia and urinary tract infection (UTI), as recommended by the Ministry of Health (2000) 15, as well as dumping syndrome in the case of pregnant women who underwent surgery before pregnancy. The cut-off point for the presence of anemia in the third trimester was 11.0 g/dl, in accordance with recommendations of the Centers for Disease Control and Prevention (1998) 16.
For assessment of serum concentrations of retinol and β-carotene, the method of High Performance Liquid Chromatography with ultraviolet detector (HPLC-UV) was used. The following cut-offs points were used to indicate inadequacy: retinol serum values < 1.05 μmol/L (30 μg/dL <) and β-carotene ≤ 40 µg/dL 17.
In the functional assessment of VAD, the presence of night blindness (NB) was investigated in the three groups through an interview standardized by the WHO (1996) 18 and the Pan-American Health Organization (1999) 19, and adapted and validated for pregnant women by Saunders et al. 20,21. Both the biochemical and the functional assessments were performed in G1 and G2 during or immediately after delivery and in G3 in the postoperative period, for a maximum of two years after surgery.
The instrument used in data collection was pre-tested and comprised a completed form filled by a single interviewer, with data from the interview and consultation of the prenatal care records.
In relation to the statistical analysis, for verification of normality the Kolmogorov-Smirnov and Shapiro-Wilk tests were used. Quantitative data were described in measures of central tendency and dispersion, and in the comparison of the means of the groups either the Mann-Whitney test or the Kruskal-Wallis test was used. To test the homogeneity of proportions between categorical variables the Chi-square test was used, and prevalence ratio was calculated. In the analysis, a significance level of 5% was adopted. The overall statistical assessment was carried out in the SPSS statistical package for Windows, version 21.0.
RESULTS
CHARACTERIZATION OF PATIENTS
The study was conducted with adult women aged 20-49 years. Pregnant women were paired by age (G1: 30.80 ± 4.45 vs. G2: 29.3 ± 5.35; p = 0.129) and prepregnancy BMI (G1: 26.84 ± 3.14 vs. G2: 25.72 ± 3.23; p = 0.072), while the women who had previously undergone bariatric surgery were paired by age (G2: 32.56 ± 4.69 vs. G3: 30.8 ± 4.45; p = 0.075) and presurgery BMI (G2: 42.91 ± 3.17 vs. G3: 43.10 ± 5.08; p = 0.809).When the postsurgical BMI of G2 (the last one recorded before pregnancy) and of G3 (end of the second year after surgery) were considered, no significant differences were found between the groups (G2: 26.84 ± 3.14 vs. G3: 26.43 ± 3.20; p = 0.638).
INADEQUACY OF VITAMIN A
The percentages of inadequacy of retinol and β-carotene showed significant differences among the three groups (Table I). Women who became pregnant after RYGB showed percentage of inadequacy of retinol three times higher when compared to women who only became pregnant or women who just underwent bariatric surgery (p < 0.001*, for both). It was also noted that although the percentage of inadequacy of retinol in G1 and G3 remained similar, β-carotene was significantly higher in women in the latter group (p = 0.001).
Table I Percentage of inadequacy, means and standard deviation of retinol, β-carotene and presence of night blindness in the assessed groups

Chi-square test was used for categorical variables and Kruskal Wallis test was used for continuous variables (*p < 0.05); G1: comprising 80 pregnant women; G2: comprising 40 pregnant women who had previously undergone RYGB; G3: comprising 77 non-pregnant women who had previously undergone RYGB.
When considering the mean concentrations of retinol and β-carotene, it was observed that both were significantly higher for the women who became pregnant when compared to the women who became pregnant or did not become pregnant after RYGB (p < 0.001*, for all) (Table I). In addition, pregnant women who had previously undergone RYGB showed means of retinol and β-carotene significantly below those found in the women who had only undergone this surgery (p = 0.0052 and p = 0.014, respectively).
Thus, it was noted that RYGB, per se, had a greater impact on the inadequacy of retinol and β-carotene when compared to non-surgical pregnant women. When surgery was associated with pregnancy, more than 75% of inadequacy of vitamin A (retinol and β-carotene) was noted, as well as a higher percentage of individuals with NB. Similar results were found for NB, as demonstrated below (Table I).
FUNCTIONAL ASSESSMENT OF VITAMIN A
The percentage of women with NB was significantly higher in G2 when compared to G1 or G3 (p < 0.001 and p = 0.001, respectively), and yet, women who had only undergone RYGB presented higher NB percentages than pregnant women who had not undergone this surgery (p = 0.016) (Table I). In addition, we found association and concordance between inadequacy of retinol and presence of NB in G1 and G3 (association: p = 0.006; p = 0.008 and concordance: p = 0.003; p = 0.006), and between inadequacy of retinol and inadequacy of β-carotene and presence of NB in G2 and G3 (association: p = 0.01; p < 0.001 and concordance: p = 0.002; p < 0.001).
OBSTETRIC VARIABLES AND GESTATIONAL AND NEONATAL INTERCURRENCES
Analysis of the obstetrical variables showed that mean time interval between the DLMP and the RYGB in women who became pregnant after surgery was 21.07 ± 14.15 months. Moreover, gestational intercurrences were significantly higher when pregnancy occurred after surgery, namely UTI (G1: 1.3% vs. G2: 35%, with p < 0.001) and anemia (G1: 30% vs. G2: 75%, with p < 0.001); however, HSP showed no significant differences between the groups (G1: 10% vs. G2: 2.5%, with p = 0.269).In relation to neonatal intercurrences, preterm (G1: 5% vs. G2: 2.5%, with p = 0.664), SGA (G1: 7.5% vs. G2: 17.5%, with p = 0.122), LGA (G1: 7.5% vs. G2: 0%, with p = 0.177), macrosomia (G1: 2.5% vs. G2: 0%, with p = 0.552) and low birth weight (G1: 6.3% vs. G2: 2.5%, with p = 0.662) showed no differences between the groups. In addition, it should be noted that dumping syndrome was present in almost half of the women in G2 (42.5%).
When comparing the serum concentrations of retinol and β-carotene among women who showed gestational intercurrences, we observed that the concentrations of retinol (G1: 2.08 ± 0.95 vs. G2: 1.07 ± 0.22, with p < 0.001) and β-carotene (G1: 80.72 ± 65.15 vs. G2: 28.81 ± 13.77, with p < 0.001) were significantly lower in pregnant women who underwent bariatric surgery, with β-carotene showing mean below the cut-off point. In relation to the presence of neonatal intercurrences, a similar result was found since the mean concentrations of retinol (G1: 2.08 ± 0.94 vs. G2: 0.75 ± 0.46, with p < 0.001) and β-carotene (G1: 82.18 ± 35 vs. G2: 9.75 ± 15.01, with p = 0.017) were significantly lower in G2.
When dividing women who showed such intercurrences according to the groups studied, we found that G2 had serum concentrations of retinol and β-carotene significantly lower in relation to the presence of anemia and SGA infants (Table II). It is important to note that G2 was also seven times more likely to develop anemia and 42 times more likely to develop UTI. Thus, it was observed that G2 showed increased prevalence ratio for developing gestational/neonatal intercurrences (UTI, SGA, and anemia), when compared to G1.
DISCUSSION
The gestational period is a physiological time which, in isolation, results in increasing demands of numerous vitamins and minerals, especially vitamin A that can have its requirements increased by 40% for maintenance of placenta and fetal development 22,23. In addition, bariatric surgery, per se, can also facilitate the occurrence of these inadequacies and, in this scenario, vitamin A stands out as it has been considered one of the most reduced micro-nutrients 24,25. This can be observed in the current study, since the percentage of inadequacy of retinol in both G1 and G3 was more than 20%, and β-carotene was the most depleted in women who underwent the surgical procedure.
This greater reduction of serum concentrations of β-carotene can be justified by the likely bioconversion to retinol, since it is its most powerful precursor, demonstrating the existence of a synergistic relationship between them 26. The highest percentage of inadequacy observed in G3 can be justified by metabolic disorders derived from the surgical procedure, especially regarding the exclusion of the duodenum in conjunction with the proximal portion of jejunum, main sites of absorption of micronutrients such as vitamin A 24,27,28.
Thus, the occurrence of pregnancy after bariatric surgery can worsen VAD, especially in the third trimester of pregnancy, period of the greatest transfer of this vitamin to the fetus. This can occur not only due to the changes caused by surgery regarding digestion, absorption and transport, but also due to the hemodilution that occurs in pregnancy in a physiological way 29.
In this context, the current study showed that the serum concentrations of retinol and β-carotene were significantly lower in pregnant women who had previously undergone RYGB compared to pregnant women, or women who only underwent this surgical procedure. In addition, means of retinol and β-carotene in G2 were below the mean of adequacy (retinol: 0.99 ± 0.39; β-carotene: 28.87 ± 15.07), while in G1 they were above the mean of adequacy, and in G3 only β-carotene showed means below recommendation. Such findings show that post-bariatric pregnancy can contribute to greater demands of vitamin A, and that the surgery, in isolation, can exert more influence on the inadequacy of the nutritional status of vitamin A when compared to pregnancy without a prior surgery.
Post-bariatric pregnant women also showed a percentage of gestational intercurrences significantly higher for UTI (G1: 1.3% vs. G2: 35%, p < 0.001) and anemia (G1: 30% vs. G2: 75%, p < 0.001), and those who developed anemia in pregnancy had the mean concentrations of this vitamin below the cut-off point, and these concentrations were significantly lower when they were compared to the ones found in G1 (retinol: G1: 2.05 ± 0.86 vs. G2: 1.02 ± 0.28, p < 0.001*; β-carotene: G1: 81.55 ± 66.84 vs. G2: 27.96 ± 14.13, p < 0.001*).
The increase in cases of anemia in G2 can be justified by hemodilution in pregnancy, in addition to the presence of hypochlorhydria in the postoperative period and to the high percentage of pregnant women with VAD (G1: 30% and G2: 75%) 30.
It has been recognized that anemia is a common complication after RYGB, iron deficiency being its main etiology 31. Belogolovkin et al. (2012) 32 reported that the odds of developing anemia are 4.3 times higher in pregnant women who had previously undergone bariatric surgery when compared to pregnant women who had not undergone this surgery, a finding in line to the one in the current study with prevalence ratio 7 times higher.
There is evidence that VAD can also be related to UTI since its presence can facilitate the negative impact on the immune system, favoring its development 33. This can occur with growing intensity during pregnancy, due to the anatomical and physiological changes occurring in the urinary tract such as: increased urine output and the expansion of the collector system caused by uterus compression, hypertrophy of the ureter musculature, and peristaltic activity reduction resulting from the action of progesterone. The referred changes promote urinary stasis and, consequently, the presence of UTI 34. In this regard, G2 was 42 times more likely to develop urinary infection when compared to G1, which may indicate that such clinical symptoms can be intensified after bariatric surgery.
In relation to neonatal intercurrences, G2 was 2.6 times more likely to give birth to SGA infants when compared to G1, and, moreover, serum concentrations of retinol and β-carotene were significantly lower, which may suggest a possible influence of this nutrient on SGA infants, an intercurrence that can happen more intensely in this segment 35.
It is important to highlight that dumping syndrome, found in almost half of the pregnant women in G2 (42.5%), may have contributed to the greatest inadequacies of vitamin A and to the gestational/neonatal intercurrences shown. This syndrome can have intensified the decrease of food intake and contributed to a tendency to avoid the consumption of various foods, including those considered good sources of vitamin A after RYGB 7.
Regarding the functional assessment, we noted that pregnancy made possible the occurrence of NB in 20% of the participants, which can be justified by major demands of vitamin A (retinol/β-carotene) imposed by such physiological status. Similar results were found in studies conducted in Brazil showing percentages of pregnant women affected by NB with values ranging from 9.9% to 18.7% 36,37. It is worth mentioning that gestational NB has high prevalence in several regions of the world and is not only limited to regions of extreme poverty. High prevalences of VAD in pregnant women were observed in developed countries, as demonstrated in a recent systematic review carried out by 38.
It should be noted that in cases of zinc deficiency, the hepatic synthesis of retinol-binding protein (RBP) can be damaged, resulting in secondary deficiency of vitamin A even in the presence of adequate liver stores of this vitamin. Therefore, in situations of high nutritional demand, such as the gestational period, zinc deficiency can occur and decrease RBP production, which can lead to VAD 39.
Thus, it can be observed that the percentage of pregnant women with no previous surgery with NB in national studies feature values close to those found in the present study even when they are not located in regions of extreme poverty. In addition, information on the role played by zinc in the formation of RBP and its transport to target tissues was also added.
Regarding RYGB, it was possible to evidence that it contributes to the lack of vitamin A, as the percentage of women affected doubled, possibly due to the absorptive changes promoted by the surgery. When pregnancy occurred after RYGB, the percentage of individuals affected was even more expressive (75%), and it is worth highlighting that the occurrence of both pregnancy and RYGB can further compromise this segment. In addition, association and concordance were found between the presence of NB and the inadequacy of retinol or β-carotene in all groups, thus pointing out the existing relationship. Such aspect was confirmed by a recent systematic review highlighting that VAD in women who became pregnant after bariatric surgery was a contributing factor to the presence of gestational NB 40.
This study was the first to evaluate the biochemical and functional status of vitamin A nutritional status in three distinct segments and its purpose was to measure and compare the magnitude of inadequacy and possible adverse consequences of VAD to the mother and child binomial, although showing a small sample size and no assessment of serum zinc and RBD. Since NB was exacerbated in pregnant women after bariatric surgery, we suggest further investigation about the synergy between vitamin A, zinc and RBP, under the conditions studied here.
CONCLUSION
Our study showed that RYGB, in isolation, provides greater negative impact on the nutritional status of vitamin A compared to pregnancy. When pregnancy occurs after surgery, it can result in even greater risks for the serum inadequacy of retinol and β-carotene in addition to the occurrence of NB, which intensifies gestational and neonatal intercurrences. Thus, this study reinforces the importance of monitoring the serum concentrations of this vitamin in the segments studied, aiming to adjust the nutritional status of vitamin A and, consequently, bringing benefits to the mother and child health.