INTRODUCTION
Cystic fibrosis (CF) is the most frequent inherited disease in the Caucasian population and its world prevalence is about 1/2,500 people 1. In Chile, the incidence is estimated in 1/8,000 to 1/10,000 live births 2.
The most common mutation is the deletion of a phenylalanine in the 508 (∆F508) position located in the CF transmembrane conductance regulator protein that produces defective water and electrolytes transport in epithelial cells. This mutation leads to changes in viscosity of epithelial fluids leading to chronic obstructive lung disease and pancreatic insufficiency associated with intestinal malabsorption and malnutrition 1,3.
In the US, the lifespan of CF patients has increased in 20 years in the last three decades, leading to new CF-related complications such as diabetes and bone disease (CFBD) 4. In Chile, after starting the CF National Programme in 2002, patient lifespan has also increased, so it is likely that such complications will be observed in our patients 5.
Although the CFBD pathogenesis is still unclear, risk factors have been identified 6 (Fig. 1). In adults, CFBD is characterized by low BMD, osteoporosis and a high frequency of spine and not spine fractures (14 and 19%, respectively) 7.

Figure 1. Risk factors in cystic fibrosis related bone disease. Adapted from Aris et al. J Clin Endocrinol Metab 2005 (3).
There exist known association between low bone mass and malnutrition in CF patients 8,9,10,11,12, but there is debate related to BMD in well-nourished children and adolescents with this disease. Some studies find CF patients have normal bone mass 13,14 and others find low BMD 15,16,17. Studies show that the prevalence of low bone mass varies between 9 to 38% in children and adolescents with CF.
Severe CFBD compromises lung function, quality of life and the possibility of lung transplantation. For these reasons, optimizing the nutritional status, vitamin D and K plasmatic levels and calcium intake associated with physiotherapy and an early treatment of lung infections could help to improve the clinical evolution of these patients by preventing CFBD 3.
In Chile, there are no studies about bone mineralization in children and adolescents with CF. We evaluated BMD and analyzed its association with lung function and 25OHD levels. Additionally, we evaluated body composition, nutritional status, food intake and physical activity in these patients.
SUBJECTS AND METHODS
We studied subjects with CF diagnosis, performed by sweat test 18. All of them were recruited from five hospitals in Santiago, Chile. To be included in the study, patients should be five to 18 years old and clinically stable. Patients with diseases that compromise bone mineralization were excluded. Patients were weighed and measured in minimal clothing using an electronic scale (SECA 708) according to standard method. We calculated body mass index (BMI) and height for age (HA) Z- scores for each patient. Well-nourished patients were defined as BMI Z-score between 1 and -1 and short stature as HA Z-score lower than -2, using the World Health Organization (WHO) charts 19. Tanner stage was determined by physical examination and patients were categorized in two groups: children (Tanner 1) and adolescents (Tanner 2 to 5).
BMD, fat mass (FM), lean mass and body mineral content (BMC) were measured by dual energy X-ray absorptiometry (DXA) using a Lunar iDXA equipment (software 13.7 version, General Electric). Low BMD was defined as BMD Z- score equal to or lower than -2, measured in lumbar spine (LS) and total body less head (TBLH) according to the International Society for Clinical Densitometry criteria for children and adolescents 20. We also defined "at-risk" if BMD Z-score was between -1 and -2 and normal if BMD Z-score ≥ -1. To analyze patient's results, we compared them with equipment reference data (USA, NHANES/Lunar). Bone size was evaluated using the Molgaard method provided by DXA. This method described bone mineralization in growing individuals in terms of three components: bone mineral content adjusted for bone area (BMC/BA), bone area adjusted for height (BA/H) and height adjusted for age (H/A) that defines light bones, narrow bones and short bones respectively 21. Then, fat free mass (FFM), fat free mass index (FFMI) and fat mass index (FMI) were calculated comparing our data with those published by Wells et al., who considered any value below the third percentile as low 22.
Within the three months of DXA scan, all patients had a pulmonary function evaluation by standard spirometry. Patients were classified with forced expiratory volume in first second (FEV1) equal to or more than 90% and forced expiratory flow between 25 and 75 percentile (FEF25-75) equal to or more than 70% as normal 2. Fasting plasmatic levels of 25OHD were measured taking 3 ml of venous blood collected in unlighted tubes and analyzed by radioimmunoassay. We defined 25OHD values ≥ 30 ng/ml as sufficient, between 20 and 29 ng/ml as insufficient and < 20 ng/ml as deficient 23. Food intake was estimated by a frequency intake questionnaire performed by a nutritionist. Data was processed with the Food Processor(r) SQL software (Esha Research, Oregon, USA). Our results for energy intake were compared with theoretical information provided by the Cystic Fibrosis Foundation 4. Normal protein intake was defined as > 15% of total calculated calories 1, calcium intake between 800 to 1,300 mg/day and vitamin D 400-1,600 IU/day according age 2. A survey for physical activity habits with score 0 to 10 allowed patient classification as active (score 6 or more) or sedentary (score 5 or less) 24.
Information on age of diagnosis, presence of pancreatic and liver compromise or CF related diabetes, blood levels of calcium, phosphate and total alkaline phosphatase, use of systemic or inhaled corticosteroids, fracture history and number of admissions in the previous year was obtained from the clinical records. All the individuals with pancreatic exocrine insufficiency were on pancreatic enzymes and fat soluble vitamin supplements. This study was approved by the Ethics Committees at the Health Service of Santiago and the Institute of Nutrition and Food Technology (INTA). All parents and children older than eight signed informed consent.
Statistical Analysis
To detect an association between BMD and FEV1 we considered a correlation coefficient of 0.5, significance level of 0.5 and potency of 0.8, which determines a sample of 29 patients. Results were expressed as mean and standard deviation (SD) or median and interquartile range (IQR) according to variable distribution. Qualitative variables were expressed as percentages. We analyzed variable distribution with Shapiro-Wilk test and compared results using the t-test, Mann-Whitney or correlations test. Associations between qualitative variables were done by Fisher's test. All data were analyzed by STATA 12.0 software and p < 0.05 was considered as statistically significant.
RESULTS
From 91 patients, 51 met the inclusion criteria and fourteen were excluded (three had another disease that compromises bone mineralization, six refused participation and five had incomplete data). Our sample size was thus 37 patients.
Median age of diagnosis was fourteen months, 59% were males, 57.4% were children and 67% had exocrine pancreatic insufficiency. There were no patients with pubertal delay or CF-related diabetes (Table 1).
Table I. Characteristics of children and adolescents with cystic fibrosis (n = 37)
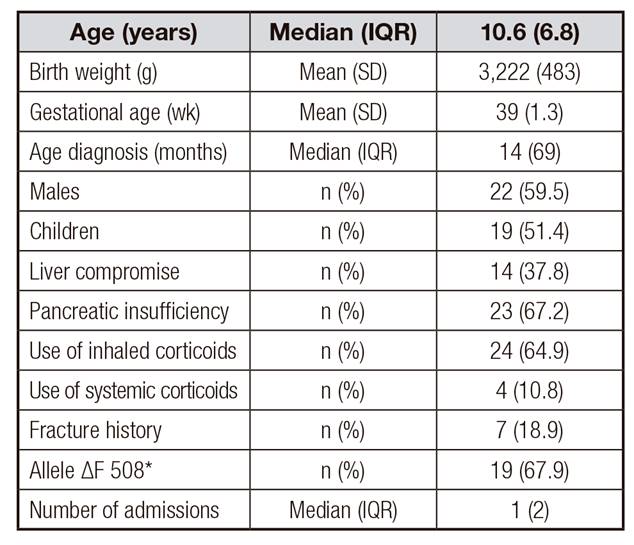
*From only 28 patients with genetic study.
Median (IQR) blood levels of calcium, phosphate and total alkaline phosphatase were normal (9.6 mg/dl [0.58], 4.96 mg/dl [0.67] and 274 UI/l [75.3], respectively).
Almost 76% of patients were well nourished and only one had short stature with no differences in BMI Z-score or HA Z-score by sex. There were no patients with low FM. Median FMI was higher in females (p = 0.002) (Table 2).
Table II. Evaluation of nutritional status and body composition by gender in children and adolescents with cystic fibrosis

*Data expressed as mean (SD);t-test.
†Data expressed as median (IQR); Mann-Whitney test.
‡Data expressed as n (%).
BMI: body mass index; HA: height for age; FM: fat mass; FMI: fat mass index; FFM: fat free mass; FFMI: fat free mass index.
FM, FFM and FFMI were significantly higher in adolescents (p = 0.001), compared to children, although 27% (10/37) had FFMI below the third percentile (Table 3). Eight of ten patients with low FFMI had normal BMI Z-score.
Table III. Evaluation of nutritional status and body composition by pubertal development in children and adolescents with cystic fibrosis

*Data expressed as mean (SD); t-test.
†Data expressed as median (IQR); Mann-Whitney test.
‡Data expressed as n (%).
BMI: body mass index; HA: height for age; FM: fat mass; FMI: fat mass index; FFM: fat free mass; FFMI: fat free mass index.
Mean values of FEV1 and FEF25-75 were 92.7 and 85.5% respectively, with no differences by sex or pubertal development. VEF1 and FEF25-75 were normal in 51 and 67.6% of patients, respectively.
25OHD plasmatic levels were insufficient in 51% of patients and deficient in 38%. Median was 23.3 ng/ml and there were no significant differences according to the season of the year in which the blood sample was taken.
Most of the patients had adequate energy and protein intake (84 and 78.4% respectively), with a daily average intake of 2,443 Kcal and 99.3 g of protein. Seventy eight percent of patients had low calcium intake and the same percentage had adequate vitamin D intake, and this fact was higher in males (p = 0.03). Patients without pancreatic insufficiency were not on fat soluble vitamin supplements and they were the only ones with vitamin D intake below the recommendation. There were no significant differences in 25OHD levels between patients with or without supplementation (21.8 and 23.6 ng/ml respectively).
Mean physical activity score was 4.2 with no differences by sex, but scores were significantly lower in children compared to adolescents (3.7 and 4.1 respectively, p = 0.01). Sedentary patients had significantly lower FFM and FFMI than active ones (p = 0.03).
We do not find any correlation between BMD and age of diagnosis, pancreatic or liver compromise, use of systemic or inhaled corticosteroids, number of admissions, physical activity or food intake.
The prevalence of low BMD was 8.1% in LS and 2.7% in TBLH; 24.3% of the sample had at-risk BMD Z-score in both locations. Mean BMD Z-score was normal in LS and TBLH, without significant differences by sex. Evaluation of bone size showed that females tended to have narrower bones than males (p ≥ 0.05) (Table 4).
Table IV. Evaluation of bone mineral density and bone size by gender in children and adolescents with cystic fibrosis
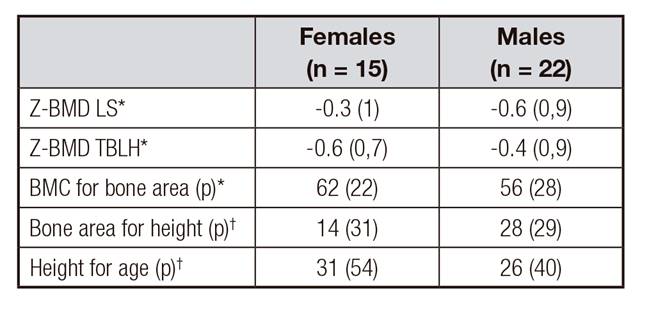
*Data expressed as mean (SD); t- test; p = ns.
†Data expressed as median (IQR); Mann-Whitney test; p = ns.
BMD: bone mineral density; LS: lumbar spine; TBLH: total body less head; BMC: bone mineral content; (p): percentiles.
Mean BMD Z-score in adolescents was lower than mean BMD Z-score in children in both locations, but not statistically significant (Table 5).
Table V. Evaluation of bone mineral density and bone size by pubertal development in children and adolescents with cystic fibrosis

*Data expressed as mean (SD); t-test; p = ns.
†Data expressed as median (IQR); Mann-Whitney test; p = ns.
BMD: bone mineral density; LS: lumbar spine; TBLH: total body less head; BMC: bone mineral content; (p): percentiles.
Patients with FFM lower than the third percentile had a higher risk of low or at-risk BMD Z-score in both locations (LS p = 0.006, TBLH p = 0.001) (Fig. 2).
We found significant correlations between BMD Z-score with BMI Z-score (r = 0.5. p = 0.001) and BMD Z-score with HA Z-score (r = 0.6, p = 0.0001), and no correlations between BMD Z-score and pulmonary function or 25OHD levels.
DISCUSSION
In our study, conducted with a sample of children and adolescents with CF, a lower prevalence of low BMD in LS (8.1%) than that described by other authors was found (17 to 38%) 8,12,17,25. Moreover, 24.3% of patients had an at-risk BMD Z-score in both locations, which is also lower than that shown in previous reports (28 to 40%) 12,26,27,28. In spite of this, the fact that adolescents have lower mean BMD Z-score than children (difference near significant in TBLH, p = 0.07) could mean that adolescents are gaining less bone mass than expected for their age. This situation has been described in longitudinal studies in children and adolescents with CF 29,30. Low BMD prevalence could increase in our older patients if lower bone mass gaining is sustained over time.
In spite of an adequate number of patients to detect a correlation coefficient of 0.5 (power 80%), no significant correlation between BMD and pulmonary function was found. This lack of correlation could be explained by a lower dispersion of FEV1 and FEF25-75 values, most of them within a normal range. In other published studies, where this correlation is significant, patients had different degrees of lung function compromise 9,12,17,25.
Although similar to other reports 31,32, 89% of patients had low 25OHD plasmatic levels, no significant correlation with BMD was found. This is in accordance with other reports, however, no clear explanation has been proposed 10,17,25,33,34. It is known that 25OHD plasmatic levels lower than 20 ng/ml are associated to an increase in parathyroid hormone (PTH) which could generate a greater loss of bone mass. Because PTH was not measured, we do not know which children could have secondary hyperparathyroidism 23).
25OHD deficiency in our patients is troublesome because it means that vitamin D supplements are not enough to reach optimal plasmatic levels and this could have negative effects in bone mineralization 35 and pulmonary exacerbations 36,37.
Only 8% (3/37) of patients had a BMI Z-score less than -1, but 27% (10/37) had low FFMI, and eight of these had normal BMI. Low FFM was significantly associated with low BMD. These results are clinically important because they provide evidence that normal or high weight in these patients are the result of increases in FM that hide low FFM, a phenomenon that has been described in children and adults with CF 38,39. This is relevant because low FFM is associated with worse pulmonary function 17,40,41 and low bone mass 12,29. Our findings point to the need to evaluate body composition frequently.
The high proportion of individuals with low FFM in the context of adequate caloric and protein intake could be explained, in part, for the high levels of sedentary activity. It is known that lean mass exercise influence over bone development 42, thus promoting physical activity in these patients should increase lean mass as well as bone mineralization.
Most of studied subjects (78%) had a calcium intake lower than the recommendation, which is contrary to what has been published in many other studies 9,11,13,15,16. This could reflect the low calcium intake in our healthy adolescents 43. Although calcium intake was not associated with low BMD, its intake is important in the long term because physical activity and calcium intake are the main environmental factors related to maximum bone mass 44.
There are different methods to measure body composition in children and adolescents such as multiple skinfold anthropometry, DXA, bioelectrical impedance analysis and air displacement plethysmography, among others. We choose DXA because it measures fat mass, lean tissue mass and bone mineral content directly. In addition, it is easy to perform, the radiation dose is extremely low (equivalent to the natural background radiation exposure in one day) and it is highly reproducible 45. We know that if we want to measure body composition repeatedly, it would be better to use a cheaper and no radiation method.
In summary, our findings indicate the need for systematic evaluation of body composition, increasing physical activity as a part of treatment to improve FFM and increasing calcium and vitamin D intake with the aim to sustain an adequate BMD in children and adolescents with CF.















