INTRODUCTION
Metabolic syndrome (MS) is the presence of three or more of the following risk factors: abdominal obesity (AO), high blood pressure (HBP), high fasting plasma glucose, hypertriglyceridemia and low HDL cholesterol (HDL-C) 1. MS increases the risk of cardiovascular disease and type 2 diabetes 2, both of which are major causes of mortality in the world 3. The risk of these cardiometabolic diseases increases as the number of the MS components rise 4. Also, AO 5 and the rest of MS components are independent risk factors for the development of cardiovascular disease 4,6 and type 2 diabetes 4. The etiology of MS and each of its components is attributable to an interaction between genetic, metabolic and environmental factors 6,7,8.
The MS prevalence in the world ranges from < 10.0% to as much as 84.0%, depending on sex, age and ethnicity of the studied population, and the definition of the MS used 8. According to the diagnostic criteria of the National Cholesterol Education Program's Adult Treatment Panel III, MS prevalence amongst adults in several Latin American countries ranges from 18.8% to 43.3% 9, and particularly in Mexico it ranges from 24.4% to 36.8% 10,11. The most frequent MS component in Mexican population is AO (76.6%) 12 followed by low HDL-C (60.5%) 13. The high prevalence of MS and its components in adults coupled with its potential health consequences make this disorder a public health problem and a financial burden on the healthcare system 14.
The prevalence data of MS and its components among health professionals are scarce. The limited evidence shows that the prevalence of MS among health personnel from Latin American countries such as Brazil 15,16, Venezuela 17, Ecuador 18 and Colombia 19 is less than 17.0%, while in Mexico the frequency of MS in medical professionals ranges from 14.5% to 19.0% 20,21,22, and among nursing professionals the frequency is 33.0% 20,21,22. The most frequent MS component in this population group was also AO 15,16,18-20. However, more data from other groups of health workers are needed, and these data need to be complemented with data regarding the association of MS and its components with sociodemographic and lifestyle factors. In addition, it is necessary to evaluate these cardiometabolic risk factors in order to implement timely and specific actions. Because of the significant role that health professionals play in promoting health, their behaviors can potentially influence the health of the general population. It is thus important for them to maintain a low-risk health status. A positive association has been shown between health professionals' healthy behaviors and their patients having positive attitudes toward preventive recommendations 23 and preventive health practices 24.
Therefore, the objective of the present study was to evaluate the prevalence of MS and its components among young health professionals in Mexico at the University of Guadalajara, in relation to their sociodemographic characteristics and physical activity (PA) levels.
MATERIAL AND METHODS
STUDY DESIGN AND SAMPLE
A cross-sectional multicenter study entitled LATIN America METabolic Syndrome (LATINMETS) was conducted. LATINMETS is a study coordinated by the Universitat Rovira i Virgili in Spain that was carried out in five Latin American Countries (Mexico, Brazil, Argentina, Paraguay and Colombia), which together form the Ibero-American Network for the Study of Metabolic Syndrome (RIBESMET; www.ribesmet.org). This paper only analyzed results from Mexico.
Participants were university students enrolled in their final semesters of study and professionals in the fields of medicine, nursing, nutrition, dentistry, psychology and pharmaceutical biochemistry. In addition, participants either worked or studied at the University of Guadalajara or at the Civil Hospital of Guadalajara from January 2011 to July 2013 and were all in apparent good health. Invitations to take part in the study were initially issued at random to students and professionals at the University Center for Health Sciences, University of Guadalajara. However, due to a low response rate among the professionals, the study was opened to volunteers with the above-mentioned profiles. Pregnant or lactating women were excluded, as were oncological patients and individuals taking corticosteroid medications. Also, those who were not evaluated for some components of MS were eliminated. A total of 462 volunteers were invited to participate, of which 319 met the inclusion criteria. Of this number, three were eliminated (women under the age of 23 with no biochemical abnormalities) because their waist circumference or blood pressure measurements were not collected (data not shown).
The study was conducted in accordance with the Declaration of Helsinki guidelines, and all procedures were approved by the ethics and research committees of the University Center for Health Sciences, University of Guadalajara (No. CI-13909). All participants signed an informed consent.
SOCIODEMOGRAPHIC AND LIFESTYLE VARIABLES
Sociodemographic variables, such as age, sex, occupational status (student or professional) and health sector, and lifestyle variables, such as smoking status (non-smoker or smoker), medication consumption and physical activity (PA), were collected from interviews and from a structured questionnaire. PA levels were evaluated based on a Spanish-language version of the Minnesota Leisure-Time Physical Activity Questionnaire 25. The amount of time spent weekly on PA and daily energy expenditure (kilocalories/day) on PA (MET*minutes*days per week) were calculated based on the frequency of each activity and the average time spent per day. For the purposes of interpretation, daily energy expenditure was categorized into quartiles.
ANTHROPOMETRIC VARIABLES
Measurements of body weight (TANITA UM-061® electronic scale, 0.1 kg), height (SECA® stadiometer, 0.1 cm) and waist circumference (fiberglass measuring tape, 0.1 cm) were taken in accordance with the International Society for the Advancement of Kinanthropometry. Using these data, body mass index (BMI) (weight [kg]/height [m]2) was calculated.
BLOOD PRESSURE
Systolic and diastolic blood pressure were measured on both the left and right arms (Omron HEM-705CP®) according to the recommendations of the European Society of Hypertension and the European Society of Cardiology 26. HBP was diagnosed based on the average of the systolic and diastolic blood pressure measurements from the arm which produced the higher pressure reading 26.
BIOCHEMICAL DETERMINATIONS
A 12-hour fasting blood sample was drawn from each participant. Subsequently, it was centrifuged (2,500 rpm, 4 °C, 10 min). The samples were immediately stored at -80 °C. Analyses were carried out in a local laboratory. Fasting plasma glucose was determined by the glucose oxidase method, HDL-C and triglycerides concentrations were assessed by the enzymatic colorimetric method.
METABOLIC SYNDROME DEFINITION
MS was diagnosed based on 2009 consensus criteria jointly developed by institutions focused on cardiovascular health 1. MS was defined as the presence of three or more of the following risk factors (components): abdominal obesity (waist circumference ≥ 80 cm in women and ≥ 90 cm in men; criteria for Central and South American populations), hypertriglyceridemia (triglycerides ≥ 150 mg/dl), low HDL-C (HDL cholesterol < 40 mg/dl in men and < 50 mg/dl in women), high blood pressure (systolic blood pressure ≥ 130 mmHg and/or diastolic blood pressure ≥ 85 mmHg) and high fasting plasma glucose (glucose ≥ 100 mg/dl). The intake of medication to treat any of the previously mentioned components (except abdominal obesity) was also considered as a criterion for determining the presence of abnormalities.
STATISTICAL ANALYSIS
A descriptive analysis of MS prevalence and its components was carried out. Categorical variables are expressed as numbers and percentages, and the association between them was calculated using the Chi-square statistical test.
The association between MS and its components, and sociodemographic and PA variables, was assessed using an age and sex adjusted logistic regression analysis. A value of p < 0.05 was considered as significant. Statistical calculations were performed using SPSS version 20 statistical software for Windows.
RESULTS
A total of 316 participants were analyzed. The majority were women (70.9%), students (59.5%) and under the age of 29 years (83.8%). The most highly represented health sectors were nutrition (24.8%) and pharmaceutical biochemistry (22.5%). Personal pathological antecedents such as dyslipidemia (3.8%), hypertension (1.3%) and type 2 diabetes (0.9%) were infrequent, as was the taking of drugs to treat these diseases (< 1%). The frequency of overweight was 24.7%, and 8.5% of participants presented obesity. Smoking was self-reported by 10.5% of the sample. The majority of subjects reported engaging in PA for more than 150 minutes per week (98.1%) or more than 30 minutes per day (95.9%) (some data not shown).
Approximately half (55.5%) of all participants presented one or more MS components (0.6% had four, and no one had five). Significant differences were observed in the frequency of the number of components according to sex, age group, professional status and BMI classification (p < 0.05) (Table 1). The presence of one or more components was more frequent in subjects over the age of 30 (72.5%) and in those who were overweight or obese (82.9%) (p < 0.05).
Table I. Frequency of the number of metabolic syndrome components in young health professionals†
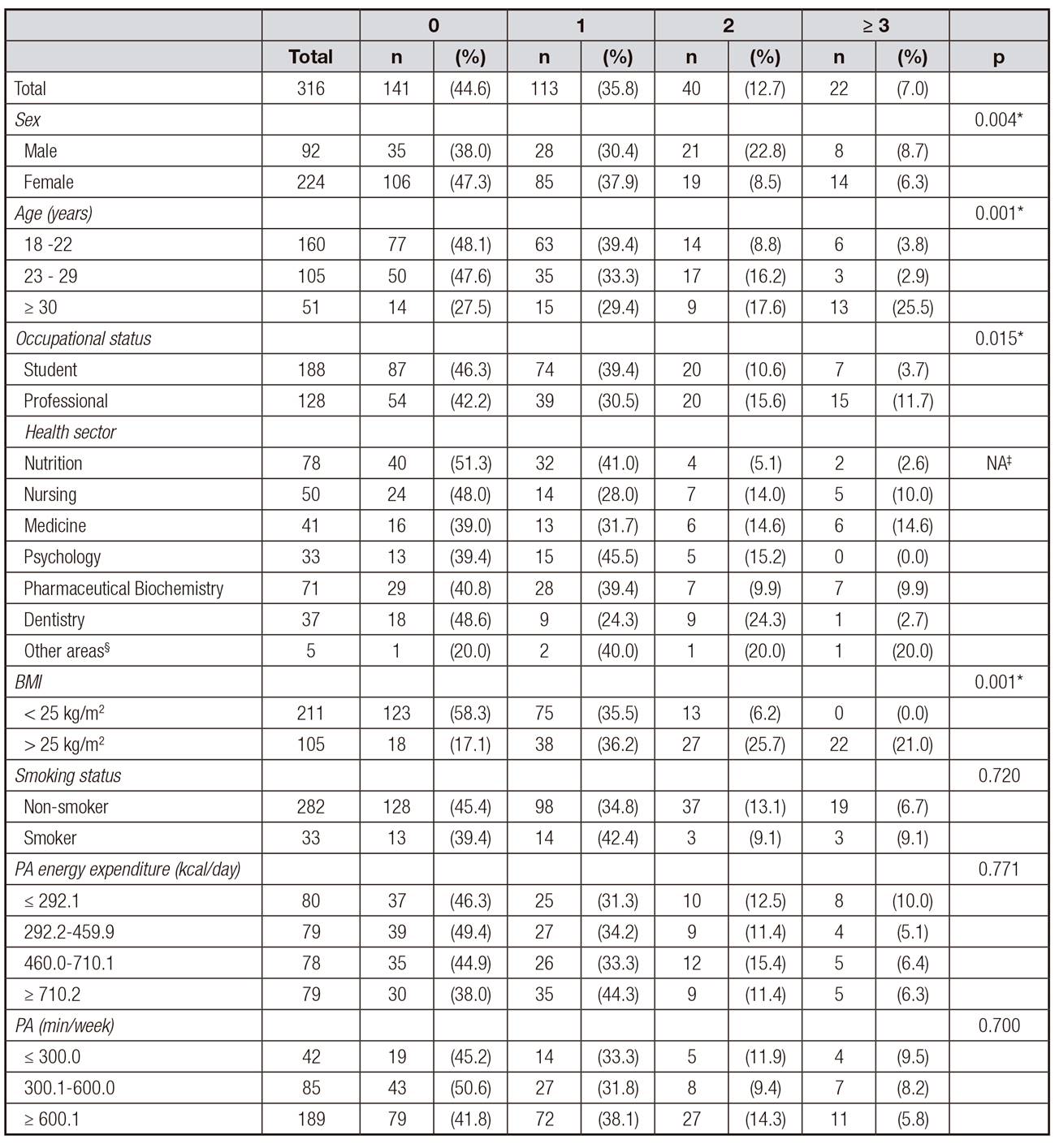
NA: does not apply; BMI: body mass index; PA: physical activity.
*p < 0.05 was considered as significant.
†Associations between qualitative variables were analyzed using the Chi-square statistical test.
‡Chi-square test not used; more than 20% of expected values are < 5.
§Other areas: Biology, Chemistry, Ph. D. in Public Health.
The most common MS components were AO (27.2%) and low HDL-C (26.6%). Only 0.9% had high fasting plasma glucose (Table 2).
Table II. Frequency of metabolic syndrome components in young health professionals†
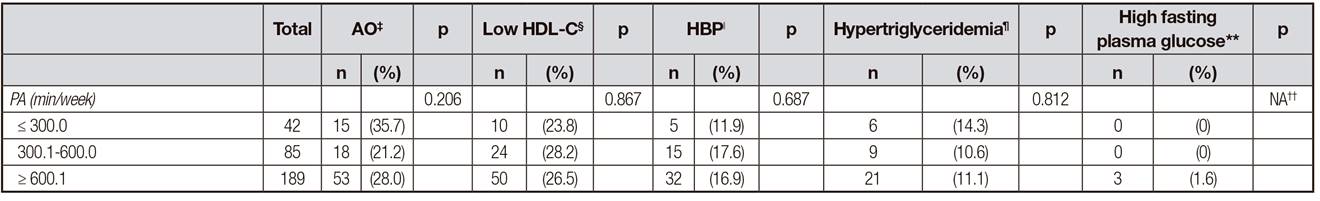
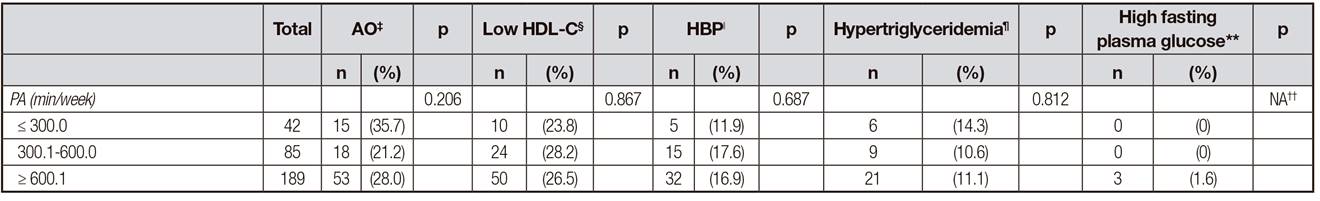
AO:abdominal obesity; HBP: high blood pressure; NA: does not apply; BMI: body mass index; PA: physical activity.
*p < 0.05 was considered as significant.
†Associations between qualitative variables were analyzed using the Chi-square statistical test.
‡Abdominal obesity: waist circumference ≥ 80 cm in women and ≥ 90 cm in men (criteria for Central and South American populations).
§Low HDL-C: HDL cholesterol < 40 mg/dl in men, and < 50 mg/dl in women.
ǁHigh blood pressure: systolic blood pressure ≥ 130 mmHg and/or diastolic blood pressure ≥ 85 mmHg.
¶Hypertriglyceridemia: triglycerides ≥ 150 mg/dl.
**High fasting plasma glucose: glucose ≥ 100 mg/dl. The intake of medication to treat any of the previously mentioned components (except abdominal obesity) was also considered as a criterion for determining the presence of abnormalities.
††Chi-square test not used; more than 20% of expected values are < 5.
‡‡Other areas: Biology, Chemistry, Ph.D. in Public Health.
AO, HBP, and hypertriglyceridemia were observed more frequently (p < 0.05) in subjects older than 30 years and overweight or obese subjects. AO was more frequent in the medicine area and less frequent in the area of nutrition (p = 0.013). HBP and hypertriglyceridemia were more frequent in men (p < 0.05) while low HDL-C was more frequent in female subjects (p = 0.018). Contrary to what was observed in the other components, no significant differences (p > 0.05) were observed in the frequency of low HDL-C according to age, health sector and IMC (Table 2).
AO, HBP and hypertriglyceridemia were positively associated with being older than 30 years, and these three components were also positively associated with BMI ≥ 25 kg/m2 after adjusting for age and sex. HBP and hypertriglyceridemia were negatively associated with being female while low HDL-C was positively associated with this gender after adjusting for age. AO was the only component negatively associated with PA (300 to 600 minutes per week) after adjusting for age and sex. None of the MS components was significantly associated with occupational status and smoking status after adjustment (Table 3).
Table III. Metabolic syndrome components† and their association with sociodemographic and lifestyle variables‡

AO: abdominal obesity; HBP: high blood pressure; OR: odds ratio; CI: confidence interval; NA: does not apply; BMI: body mass index; PA: physical activity.
*p < 0.05 was considered as significant.
†Metabolic syndrome components were diagnosed based on 2009 consensus criteria jointly developed by institutions focused on cardiovascular health (1).
‡The associations between the metabolic syndrome components and the variables of interest were analyzed using logistic regression analysis.
§Abdominal obesity: waist circumference ≥ 80 cm in women and ≥ 90 cm in men (criteria for Central and South American populations).
ǁLow HDL-C: HDL cholesterol < 40 mg/dl in men, and < 50 mg/dl in women.
¶High blood pressure: systolic blood pressure ≥ 130 mmHg and/or diastolic blood pressure ≥ 85 mmHg.
**Hypertriglyceridemia: triglycerides ≥ 150 mg/dl.
††High fasting plasma glucose: glucose ≥ 100 mg/dl. The intake of medication to treat any of the previously mentioned components (except abdominal obesity) was also considered as a criterion for determining the presence of abnormalities.
‡‡OR is presented as adjusted for age and sex (sex is presented adjusted for age and age is presented adjusted for sex).
§§It was not possible to perform logistic regression analysis due to the low frequency of high fasting plasma glucose.
MS prevalence was 7.0%, with no significant differences by sex. MS was more frequent in subjects older than 30 years (25.5%, p < 0.05), and it was also positively associated with this age group. In addition, MS was more frequent in overweight or obese subjects (21.0%, p < 0.05), and all subjects who presented MS were overweight or obese as determined by BMI and AO. PA was not significantly associated with MS (Table 4).
Table IV. Metabolic syndrome† and its association with sociodemographic and lifestyle variables‡

OR: odds ratio; CI: confidence interval; PA: physical activity.
*p < 0.05 was considered as significant.
†Metabolic syndrome was defined as the presence of three or more of the following risk factors: abdominal obesity (waist circumference ≥ 80 cm in women and ≥ 90 cm in men; criteria for Central and South American populations), hypertriglyceridemia (triglycerides ≥ 150 mg/dl), low HDL-C (HDL cholesterol < 40 mg/dl in men and < 50 mg/dl in women), high blood pressure (systolic blood pressure ≥ 130 mmHg and/or diastolic blood pressure ≥ 85 mmHg) and high fasting plasma glucose (glucose ≥ 100 mg/dl). The intake of medication to treat any of the previously mentioned components (except abdominal obesity) was also considered as a criterion for determining the presence of abnormalities.
‡Associations between metabolic syndrome and the variables of interest were analyzed using logistic regression analysis.
§OR is presented adjusted for age and sex (sex is presented adjusted for age and age is presented adjusted for sex).
DISCUSSION
Half of this sample of young professionals, most of whom were students enrolled in health programs at the University of Guadalajara, presented one or more MS components, mainly AO and low HDL-C. MS prevalence was 7.0% in these participants. MS, AO, HBP and hypertriglyceridemia were positively associated with age and BMI. After adjusting for age and sex, AO was the only component negatively associated with PA. None of the sociodemographic variables or PA were significantly associated with MS after adjustment.
Irrespective of the MS prevalence observed in this study, the studied population is considered to be a cardiometabolic risk group because half of its members presented one or more MS components. In other groups of young population (18 to 25 years old) the presence of at least one MS component is also frequent 21,27,28,29,30. This information is relevant because the MS components are interrelated with each other and usually do not present in isolation 6. This means that anyone having one component is highly likely to develop more of them, particularly as age increases. In a sample of Mexican medical students it was observed that a significant proportion had one or more MS components (69.2%), and this frequency increased six years later (76.4%), mainly increased the frequency of OA and excess weight by BMI (> 25 kg/m2)21. Two other longitudinal studies conducted in Brazilian health students showed, 15 years 31 and 20 years 32 after the first evaluation, significant increases in the frequency of hypercholesterolemia, hypertension and excess weight by BMI (> 25 kg/m2), as well as a significant increase in the average value of glucose. Moreover, there is even risk of incidence of cardiometabolic disease from the presence of one component, and this risk increases as the number of the components present increases 4.
In addition, the most frequent components were AO, which is an independent risk factor for the development of MS, cardiovascular disease and type 2 diabetes 5, and low HDL-C, which is associated with an increased risk of cardiovascular disease morbidity and mortality 6. These two components have also been the most frequently presented components in other studies conducted on adults 10,11, young people 29,30 and health professionals in Mexico 20, and health personnel from Brazil 15. In addition, AO was the most frequent component in the LATINMETS studies in Colombia 19 and Brazil 16.
The third most frequent component in this study was HBP (16.5%). However, frequency of this component was greater than that observed in a sample of young Mexican population (12.1%) 30 and in health professionals in Brazil (9.3%) 16, both studies evaluated under consensus diagnostic criteria. Likewise, frequency of HBP was lower than that observed in general population from Mexico 10 and in samples of health professionals from Mexico 20, Colombia 19 and Brazil 15. On the other hand, the less frequent components in this study were hypertriglyceridemia (11.4%) and hyperglycemia (0.6%); both components were only similar to the frequency observed in medical students in Ecuador (hypertriglyceridemia: 10.96% for women and 13.27% for men; hyperglycemia: 0.2% for women and 0.34% for men) 18. Several studies where the most frequent components were AO and low HDL-C showed that hyperglycemia was the least frequent component 15,16,18,29,30.
In Latin America, etiological factors that favor the development of MS components include lifestyle factors (unhealthy food, sedentary lifestyle, and smoking, among others) as well as others of a genetic/metabolic nature (predisposition to obesity and metabolic disorders) and fetal malnutrition 6,7. In addition, health professionals have cited limited time, variable schedules, excessive workload and insufficient space as barriers to the establishment of self-care actions (healthy eating, rest/sleep, and having sufficient recreational time) 33).
All of the above suggests that the continuous monitoring of these risk factors within this young population should be carried out. Chief among these factors are AO and low HDL-C (in addition to the routine monitoring of weight, BMI and total cholesterol), given their high frequency, increased likelihood of presence with age and their potential influence on cardiometabolic health status. Systematic monitoring will ensure the availability of up-to-date scientific data on this population's health status, which will in turn aid in decision-making related to the above-mentioned health issues.
The MS prevalence rate observed in this analysis (7.0%) was lower than the prevalence reported among the general Mexican adult population (> 24.0%) 10,11. It was also lower than the frequency found among young Mexicans (< 24 years) (> 13.0%) based on consensus diagnostic criteria 29,30. Additionally, it was lower than the frequency observed in health professionals (> 30%) 20,22,34 and medical students (14.5%) 21 in Mexico. And finally, the MS prevalence observed in this study was lower than that found in the LATINMETS Colombia study (17.5%) 19. It was comparable to the MS prevalence reported in two studies that evaluated university students (18 to 25 years old) from the United States (< 1.5%) 27,28, as well as those reported in the LATINMETS Brazil study (4.5%) 16, among medical students in Venezuela (3.3%) 17 and Ecuador (7.5%) 18, and among health personnel from Brazil (12.8%) 15. Age-adjusted comparisons of MS prevalence among LATINMETS countries have already been sent to be published (Vizmanos B, Betancourt-Núñez A, Márquez-Sandoval F, et al. Prevalence of metabolic syndrome among health professionals in the multicenter study LATIN America METabolic Syndrome [LATINMETS]; 2018; unpublished data) and varied with respect to the original value in accordance with the average age of the sample. As in other studies, the MS prevalence observed in the present study was higher among groups that were older and that had higher BMI 8,10,15,16,19.
The low MS prevalence observed in this study is not attributable to the diagnostic criteria used 1, as this study employed criteria for the diagnosis of MS (such as drug consumption and cut-off points with lower numbers for AO diagnosis) that are more inclusive than those used in other definitions. The low MS prevalence may be attributable to the fact that the majority of participants were young (83.8% < 29 years), presented a low frequency of obesity (by BMI ≥ 30 kg/m2) (8.5%), had an undergraduate level of university studies and engaged in PA at a rate higher than 90% in accordance with the World Health Organization recommendations 35. Among Mexican adults, lower education levels have been positively associated with MS compared to higher education levels 10, and engaging in more than 30 minutes of PA per day 11, or in at least 150 minutes a week 35, has been negatively associated with MS compared to inactive people. In addition, the inclusion of volunteers in the study had the effect of increasing the number of participants with high interest in caring for their own health, as individuals with higher risk factors would have been less likely to participate. For example, doctors often avoid routine medical check-ups by other professionals because they tend to self-assess their own health 33. Our approach was based on a random sample from a sample census, but the low participation of this population group forced us to cease convenience sampling.
Participating in PA was not significantly associated with MS, in contrast to what had been reported in other studies 11,35. The absence of an association in the present study may be due to the fact that the majority of subjects reported engaging in PA for more than 150 minutes per week (98.1%) or more than 30 minutes per day (95.9%). Besides, the MS prevalence was low. However, engaging in 300-600 minutes of PA per week was negatively associated with AO in this population group. It has been shown that engaging in more than 150 minutes of PA per week has health benefits 35.
AO, HBP, hypertriglyceridemia and MS were all positively associated with overweight or obesity, a result consistent with the scientific evidence that MS is a consequence of the metabolic complications of obesity 36.
One of this study's strengths is that it provides current data on the cardiometabolic risk factors present within a previously unstudied population of young Mexican health professionals. Another strength of this study is that MS was evaluated using MS diagnostic criteria from the most up-to-date consensus, which include cut-off points for the diagnosis of AO that are specific to each ethnic group 1.
In conclusion, half of the participants presented one or more MS components, particularly AO and low HDL-C. The frequency of MS in this sample of young health professionals from the University of Guadalajara (Mexico) was 7.0%. After adjusting for age and sex, AO, HBP and hypertriglyceridemia were positively associated with BMI ≥ 25 kg/m2, and AO was negatively associated with engagement in PA. MS was not associated with sociodemographic variables or with PA after adjustment.
It is necessary to implement programs of continuous epidemiological surveillance of major modifiable cardiometabolic risk factors (LDL hypercholesterolemia, hypertriglyceridemia, hypertension, metabolic syndrome, inflammatory and genetic markers, type 2 diabetes, abdominal obesity, physical inactivity, smoking, alcohol consumption, stress and unhealthy diet) in young populations with and without overweight, in order to implement timely and specific actions.
In addition, multidisciplinary care should be provided to individuals who present one or more MS components, and initiatives for the treatment and prevention of overweight, obesity and AO should be implemented as a strategy to lower the frequency of MS components and, in consequence, of cardiometabolic risk 6. Depending on the characteristics of the population being studied, efforts could focus on facilitating access to healthy food (with the aim of reducing processed carbohydrates, total fat and total energy intake, while also increasing the intake of foods rich in antioxidants and fiber) and plain water (as a substitute for sweetened drinks). The encouragement of behaviors that promote low-risk health status could start in universities, hospitals or workplaces, environments in which this population spends a substantial part of each day.














