INTRODUCTION
Overweight among women of reproductive age has been growing at an alarming rate in recent decades, becoming a serious public health issue in Brazil. Currently, 50.5% of adult women are overweight and 19.6% are obese, with a higher risk of developing chronic diseases and a tendency towards worse obstetric outcomes 1,2.
The pregnancy-puerperal cycle involves physiological adaptations that induce significant changes in body weight and composition 3. Excessive gestational weight gain and postpartum weight retention (PWR) are strong predictors of obesity development 3,4,5. The greater the gestational weight gain, the higher the PWR verified in one year, and the higher the body mass index (BMI) in subsequent years 5. Therefore, it is recommended that women return to pre-gestational weight within 12 months after delivery 5,6.
Nutritional counselling is effective in promoting PWR reduction 7,8,9,10. However, there is a lack of a specific protocol at Brazilian public primary health care to monitor health and nutrition of women in the postpartum period 11. Moreover, commitment to nutritional care during the postpartum period is challenging due to the demands of motherhood, which are notably worse for low-income women 12. Thus, there is a current call to action to development of new strategies that could better achieve this specific public 11,12.
The present study aimed to evaluate the effect of nutritional counselling at primary health care on the reduction of PWR in a low-income community in southeastern Brazil.
MATERIAL AND METHODS
STUDY DESIGN AND POPULATION
This pilot study was conducted from November 2016 to September 2017 in two primary health care centers located in a low-income community in southeastern Brazil.
All women registered in the health center's information system were identified with the potential to participate in the study. Individuals that met the following inclusion criteria were selected: women 6-9 months postpartum, with weight retention of any magnitude, BMI above 18.5 kg/m2, older than 18 years old, single-fetus pregnancy, a living infant, absence of diagnosis of chronic diseases (except for obesity), no history or diagnosis of eating disorders, and no bariatric surgery.
Individuals were invited to participate through phone calls or personally in the health centers waiting rooms and childcare groups. The project was widely disseminated among health professionals and community using posters and leaflets. Women who agreed to participate had their first appointment scheduled, during which the data regarding sociodemographic characteristics, obstetric history, pre- and postnatal care, and conditions of the child at birth were verified through a face-to-face interview and medical records.
INTERVENTION
The study participants attended four individual appointments with a nutritionist over three months of follow-up. Nutritional counselling was performed based on the Dietary Approach to Stop Hypertension (DASH) diet 13. The DASH diet is recognized as a healthy and beneficial dietary pattern for women of reproductive age 14. Most daily energy consumption should derive from plant foods, such as fruits, vegetables, seeds, oilseeds, beans, and whole grains, restricting the consumption of meat and other foods with high amounts of saturated fat, salt, and sugar 13. However, it is an American dietary pattern, so it had to be translated and adapted for this study, especially considering typical foods that were accessible to the Brazilian population (in press).
The meal plan delivered to women was organized into six meals, setting up a daily menu model with the recommended number of portions of the adapted DASH diet groups: 7-8 servings of cereals, preferably whole-grain cereals; 4-5 servings of vegetables; 4-5 servings of fruits; 2-3 servings of dairy products, preferably low-fat; 2-3 servings of oils; 1-2 servings of beans (typical Brazilian food); and up to two servings of meats. The consumption of seeds and/or nuts was indicated 4-5 times per week. Sugars and sugary beverages were advised against, without definition of a tolerable portion [in press].
The nutritional guidance material was developed in line with the proposal of the new Food Guide for the Brazilian Population 15, similar to others already used in the routine practice where the study was developed. A daily energy value of approximately 2,000 kcal was considered to meet the recommendation of minimum intakes for nursing mothers (1,900 kcal/day) 16.
The meal plan was delivered and explained in the first appointment. General recommendations were also made for a healthy diet, such as the amount of water intake, replacement of industrial seasonings with natural herbs and spices, reduction of consumption of ultra-processed food and moderation in the addition of salt, sugar, and fats. In subsequent consultations, with 30-day intervals, all orientation was reinforced or adjusted, according to the obtained results.
Despite the use of a common meal plan for all participants, nutritional counselling was conducted in an individualized and contextualized way based on the routine of each woman. Suggestions for foods and preparations were discussed with each participant, according to availability and affordability of certain items 17,18. Among available options, the best choices were suggested, so that women would be closest to the adapted DASH diet proposal. Physical activity was encouraged throughout the follow-up period and evaluated before and after the intervention 19.
To improve adherence to the diet, study participants received a kit containing three packages of skimmed milk powder (400 g each), two packages of linseed and/or sunflower seeds (250 g) and three seed and cereal bars (30 g each), at each visit.
In addition, as part of the intervention, the free instant messaging application WhatsApp® and the social media site Facebook® were used as tools to reinforce nutritional counselling 10,20,21. Messages regarding information on healthy eating were sent weekly. These digital tools were also used to communicate with the study participants, in order to promote self-motivation and self-monitoring 10,20,21. Women were encouraged to send pictures of meals and questions about food and nutrition, always in a private way, and were receiving answers from expert nutritionists.
ASSESSMENT OF DIET ADHERENCE
Food intake was assessed in the last appointment using a food frequency questionnaire (FFQ) validated for the Brazilian population 22. Analyses of individual food consumption were performed in Microsoft Excel. The amount consumed for each food, reported in usual units, was converted to grams/milligrams or liters/milliliters.
The frequencies of consumption reported in the FFQ as weekly or monthly were transformed into daily frequency 23. Using the Table of Nutritional Composition of Foods Consumed in Brazil 24, it was possible to verify daily consumption in kilocalories of energy and grams or milligrams of nutrients.
To evaluate the diet adherence, a DASH score 25 was used, considering the number of recommended portions in each food group, for each 1,000 kcal daily consumed: fruits (> 2.10 servings of 80 g), vegetables (> 2.10 servings of 50 g), dairy products (> 0.96 portion of 120 ml of milk or 40 g of cheese), whole grains (> 3.60 servings of 20 g), seeds/legumes (≥ 0.33 portion of 30 g of seeds/oilseeds or 80 g of beans), meat (≤ 0.80 portion of 170 g), oils/fats (≤ 1.20 portion of 5 ml) and percentage of saturated fat (< 7% of the total daily energy value).
For each food group in which the consumption recommendation was met, one point was recorded in the DASH score 25. Therefore, the score ranging from 0 (lower adherence) to 8 (higher adherence) was individually calculated. A score equal or greater than 4 was considered as good adherence to diet, and scores less than 4, as bad adherence.
ANTHROPOMETRIC EVALUATION
Anthropometric evaluation was performed in all visits, with measurements of weight (kg), percentage of body fat (%) and waist circumference (cm). Weight and percentage of body fat were measured with an electronic field balance, with bipolar bioimpedance. Participants removed their shoes and accessories and wore light clothing 26. Waist circumference was measured with a flat steel anthropometric tape, at the mean height between the iliac crest and lower costal margin 26.
Height (m) was measured at the first visit, with a fixed vertical stadiometer, in the absence of shoes and hair accessories 26. Blood pressure was measured in all consultations using a high precision digital device. The analyses for determining nutritional status were performed according to the current protocols published by the Ministry of Health of Brazil 26.
PWR was defined as the difference between the actual weight and pre-gestational weight found on the medical records. In the absence of such information, the weight recorded at the first prenatal visit was used, if it has occurred during the first trimester. The BMI was calculated using the formula BMI = weight (kg)/height2 (m).
STATISTICAL ANALYSIS
PWR was considered as the primary outcome of the study. Secondary outcomes were weight, BMI, waist circumference and body fat percentage. Due to the reduced sample size and its non-normality condition, tested with the Kolmogorov-Smirnov test, non-parametric statistical tests were adopted.
For the descriptive analyses, the results were presented as absolute and relative frequency for the qualitative variables and as median and interquartile range for the quantitative variables. The Mann-Whitney test was used to compare the medians of independent samples, while the Wilcoxon test was used for the comparison between dependent samples. The Chi-square test was used to compare qualitative variables using the Fisher's test.
Spearman's correlation was used to verify possible associations between covariables and the main outcome. Analyses were performed in the IBM SPSS Statistics version 21.0 software, adopting p < 0.05 for statistical significance of the results.
ETHICAL STANDARDS DISCLOSURE
This study was conducted according to the guidelines laid down in the Declaration of Helsinki and all procedures were approved by the Ethics Committee in Research of the National School of Public Health (CAAE 0251.0.031.031-10) and Brazilian Registry of Clinical Trials (RBR-4t46ry). Written informed consent was obtained from all study participants.
RESULTS
Following consultation of the records in the health center's information system, 478 women were identified, who would be 6-9 months postpartum during the time of data collection. Of these, 283 could not be reached. Among those who accepted to participate in the study and attended the first visit (n = 60), 19 did not meet the eligibility criteria. Forty-one women started the intervention and 26 completed it, accounting for a 36.6% loss of follow-up (Fig. 1). The mean duration of follow-up, encompassing the four visits, was 109 days (3.6 months).
The characteristics of the sample, as well as the comparison between women who completed or did not completed the study, are presented in table I. The median PWR was 5.50 kg. Regarding the nutritional status, 48.8% (n = 20) were obese and 39% (n = 16) were overweight. The median pre-gestational BMI value was 27.06 kg/m² (24.63-30.77). There was a greater loss of follow-up for younger women with higher BMI values (p < 0.05) (Table I). There were no significant differences in relation to the sociodemographic characteristics between women who completed or did not completed the study (Table I).
Table I. Characteristics of participants at baseline and comparison between individuals who have or have not completed the intervention (n = 41)
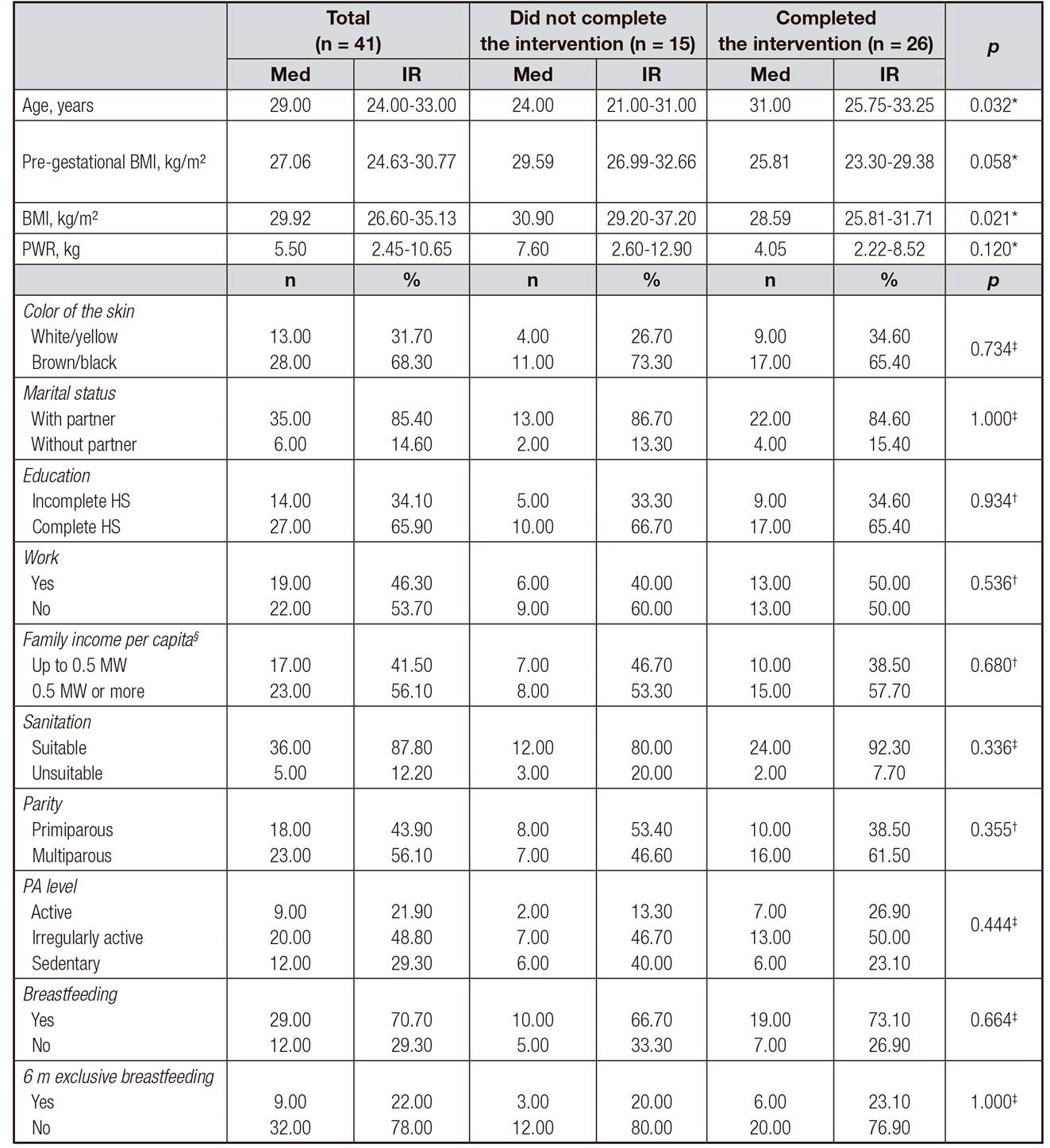
Med: median; IR: interquartile range; BMI: body mass index; PWR: postpartum weight retention; HS: high school; MW: minimum wage; PA: physical activity; 6 m: six months.
*Mann-Whitney test.
†Chi-square test.
‡Fisher's test. Confidence interval 95%.
§Missing (n = 1), 2.4%.
The sample contained a majority of black women (68.3%), married (85.4%), with high school education (65.9%), adequate sanitation at home (87.8%), multiparous (56.1%) and with low adherence to physical activities (78.1%). Most women maintained breastfeeding (70.7%), but exclusive breastfeeding up to six months was reported by only nine of them (22%).
Table II shows the anthropometric results before and after the intervention. Measurements of all parameters presented a reduction (p < 0.05) after intervention, except for body fat percentage (p = 0.346). The median systolic (SBP) and diastolic (DBP) blood pressure did not change after the intervention (initial SBP = 109 versus final SBP = 112, p = 0.909 and baseline DBP = 68 versus final DBP = 68.5, p = 0.808).
Table II. Comparison of anthropometric measurements before and after the intervention (n = 26)
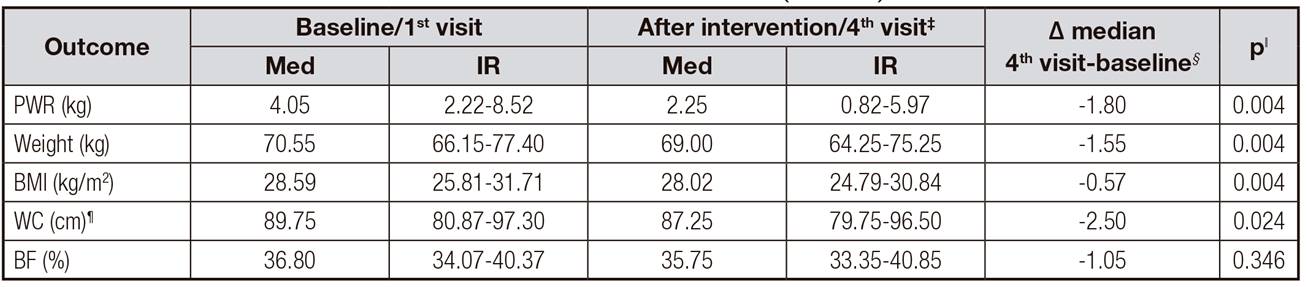
Med: median; IR: interquartile range; PWR: postpartum weight retention; BMI: body mass index; WC: waist circumference; BF: body fat.
*Mean time between 1st and 2nd visits: 38 days.
†Mean time between 2nd and 3rd visits: 37 days.
‡Mean time between 3rd and 4th visits: 34 days.
§Mean duration of the intervention: 109 days (3.6 months).
ǁWilcoxon test, comparison with baseline, confidence interval 95%.
¶Missing (n = 2).
Regarding the adherence to diet (Table III), the frequency of women who consumed the portions indicated for each food group was 50.00% for fruits, 33.33% for vegetables, 87.50% for dairy products, 16.67% for whole grains, 91.67% for seeds and legumes, 70.83% for oils and fats, 91.67% for meat and 75.00% for saturated fat. Analysis of DASH score showed that 91.67% of women presented good adherence to diet. Two women did not respond to the FFQ, as they claimed little time for the consultation.
Table III. Assessment to diet adherence and DASH score (n = 24)
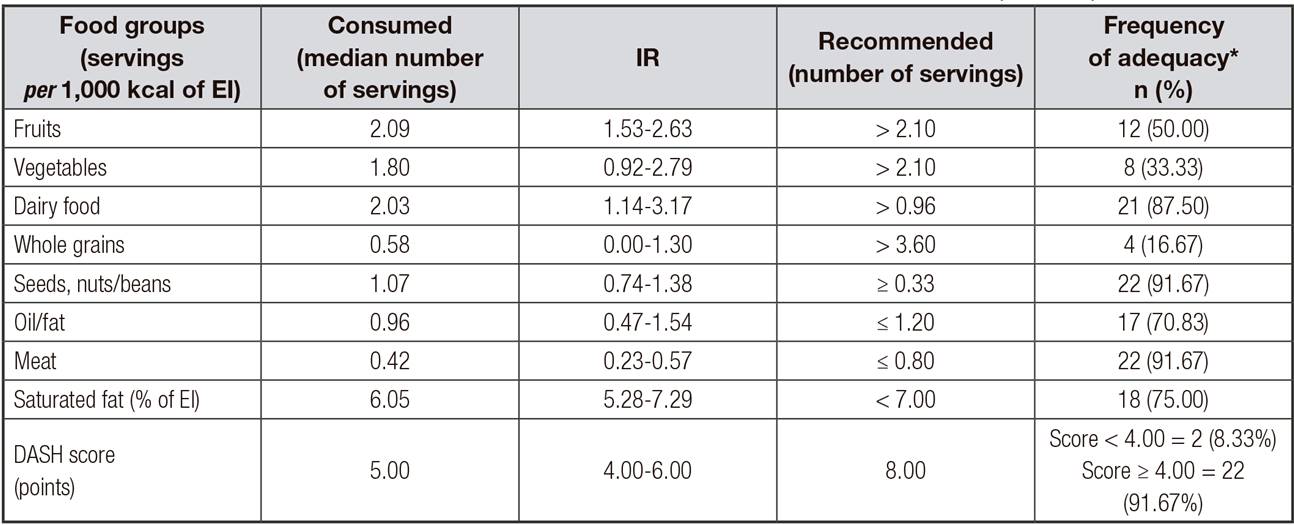
EI: energy intake; IR: interquartile range; DASH: Dietary Approach to Stop Hypertension. Median (IR) of daily energy intake: 1,876.19 (1,639.80-2,488.42) kcal.
*Number and percentage of women who individually reached the recommended intake.
About the level of physical activity, only three of the 26 women who completed the consultations were classified as "active" and this was maintained before and after the intervention. All others were "irregularly active" (n = 14) or "sedentary" (n = 9). Therefore, it was not possible to evaluate the potential impact of physical activity on postpartum weight retention.
Time after delivery and the breastfeeding period (in days) presented a negative correlation with PWR after the intervention (ρ -0.406, p = 0.040 and ρ -0.437, p = 0.025, respectively). Energy intake presented a positive correlation with PWR (ρ 0.536, p = 0.007), which did not occur for the individually assessed food groups. No correlation was observed between PWR and the following covariates tested: maternal age (p = 0.244), gestational weight gain (p = 0.203), parity (p = 0.171) and per capita family income (p = 0.677).
DISCUSSION
Our results showed that nutritional care offered to women during the postpartum period, at primary health care, contributed to the reduction of PWR, BMI and waist circumference, as women presented good adherence to a healthy dietary pattern.
The location of the study was a neighborhood with elevated levels of violence and police confrontations, which contributed to a limitation of the study, which is the small sample size. The selection and follow-up of women were constantly hampered by this social context, especially exacerbated during the study period. Lack of security limits the routine activities of women residing on-site. Attending consultations, following a diet plan, and focusing on personal goals related to nutritional status has become especially challenging in this hostile environment.
To mitigate the damages caused by these conditions, it was strategic to use communication technologies (WhatsApp® and Facebook®). Thus, it was possible to maintain communication with the study participants and promote motivation for adherence to nutritional guidelines, even when the attendance schedule was compromised. Participants sent photos, questions and comments about food and nutrition. In this way, it was possible to provide constant support and enhance the link between the research team and study participants.
A second limitation refers to the lack of a comparison group (control). This is because the project is part of an initiative to increase the supply of services to the population of the territory under study. Therefore, it was understood that all identified eligible women who expressed an interest in participation should have access to nutritional care. This option limited the elaboration of more robust conclusions regarding the cause and effect relationship of the intervention; however, it increased the range of the benefits resulting from the study.
Nutritional care initiated during pregnancy and continued postpartum is more effective in reducing weight retention than those provided only after delivery 7,9. However, in the present study, the intervention was initiated in the late puerperium. It is likely that the results may be more robust if counselling and monitoring of gestational weight gain were provided during prenatal care.
To date, no studies have been identified using the DASH diet to reduce PWR. The Mediterranean diet, with similar composition, was tested in a US study 27, over four months, in overweight postpartum women. The difference after the intervention was -2.31 kg in weight, -0.85 kg/m² in BMI, -3.47 cm in waist circumference and -1.19% in the percentage of body fat. These results were similar to ours (-1.55 kg, -0.57 kg/m², -2.50 cm and -1.05%, respectively). However, the American study was one month longer than ours.
In a survey performed at primary health care in Sweden 9, overweight postpartum women who received individual nutritional counselling for 12 weeks showed a mean reduction of 6.1 kg in weight at the end of the intervention. This weight loss was higher than the one presented here, however, an energy restriction of 500 kcal was applied in the individual food plan. In the present study, there was no energy restriction, because the meal plan had a qualitative focus.
There was a greater follow-up for older women with lower BMI values, which cannot be explained with other sociodemographic factors. However, the values of pre-gestational BMI were lower among these women, with a borderline result for statistical significance (25.81 kg/m² versus 29.59 kg/m², p = 0.058). The lower pre-gestational BMI is associated with greater weight change during and after gestation 3,4. It is possible that this more pronounced body change has motivated participants to better adhere to nutritional care than those who already have higher pre-gestational BMI.
We observed good adherence to the adapted DASH diet, especially limiting the intake of meat and saturated fat while improving consumption of dairy products and seeds, nuts and beans. These recommendations were emphasized during the nutritional orientation because they are recognized DASH markers 13 and are part of the recommendations of the Food Guide for the Brazilian Population 15. Thus, these results were associated with reduction of RPPP in other studies 28,29,30.
It is important to consider that adopting a healthy dietary pattern is a challenge for low-income women living in areas of social vulnerability, either because of financial constraints or little availability of fresh and non-industrialized foods, locally 31,32. Popular beliefs and food-related myths that prioritize the consumption of foods with higher energy density during the lactation period were also verified 33. Whole grains, vegetables and fruits had the lowest frequency of consumption adequacy, which may be associated to some of these factors. On the other hand, the better adherence to consumption of dairy products and seeds/nuts was possibly favored by the donation of these products during the intervention.
Another relevant issue, reported by a large part of the study participants, was the lack of time due to the excess of responsibilities related to family and maternity, which was considered as the main barrier to attend appointments, to commit to physical activity and to adhere to the food plan. Most studies involving postpartum women reported large loss of follow-up, generally associated with such factors 12,35.
However, the improvement in the anthropometric indicators of nutritional status and overall diet quality after the intervention indicate that, even though there is limited access to some types of foods and barriers to postpartum care for women's health, adherence to most of the recommendations has been achieved. Therefore, it is important to implement personalized guidelines to meet individual's needs, with the aim to provide available and affordable food options and share practical suggestions for meal planning and preparation.
It is known that weight loss is natural during the first year after delivery, due to the return to physiological and anatomical pre-gestational conditions and to breastfeeding 34. In fact, postpartum and breastfeeding time showed negative correlations with PWR at the end of the study. Corroborating previous findings 36, the total daily energy intake, rather than the consumption of certain food groups, correlated positively with the outcome.
The DASH diet was originally developed for the reduction of systemic arterial pressure 13. In this study, it was not possible to observe a decrease in SBP and DBP; however, the median blood pressure levels were within the normal range before and after the intervention.
Despite the unfavorable context, it was possible to successfully implement this pilot intervention in a community of economic and social vulnerability in southeast Brazil. There was a significant decrease in PWR, BMI and waist circumference. Positive results can be attributed to the good adherence to the adapted DASH diet and to contextualized nutritional counselling, with a focus on women's health. It is relevant to highlight the importance of the digital communication tools used to maintain the follow-up, although this strategy was not measured alone as an outcome of the study, but rather as part of it.
Larger trials are needed to show whether counselling on diet can improve nutritional status of postpartum women and how it should be effectively done. Currently, there is no protocol that prioritizes and guides nutritional care for women in the postpartum period at Brazilian public primary health care. Thus, this kind of study may support the improvement of pre- and postnatal care in public health services.















