INTRODUCTION
Sarcopenia is a disease (1) defined as a progressive and generalized disorder of skeletal muscle, and characterized by reduced muscle strength and muscle mass (2). It is associated with negative health outcomes such as motor dependence, increased risk for falls, and premature death (3), which increases hospitalization costs for older adults by 34 % (4). In this population sarcopenia has a prevalence of 10 % worldwide (5), and 17 % in Brazil (6). A consensus for the diagnosis of sarcopenia has been established by international agencies – EWGSOP (European Working Group on Sarcopenia in Older People) (2) and SCWD (Society of Sarcopenia, Cachexia and Wasting Disorders) (7) – based on skeletal muscle mass (SMM) loss.
Appendicular lean soft tissue (ALST), measured by dual-energy X-ray absorptiometry (DXA), is a consensual parameter for SMM among agencies. ALST includes the fat- and bone-free mass of the upper and lower limbs. It is equivalent to muscle tissue in arms and legs, except for a small amount of connective tissue and skin. For the diagnosis of sarcopenia ALST may be considered in absolute form (2,8) or adjusted for body size in different ways, using height-squared (ALST/height2, known as the ALST index) (2,7), weight (ALST/weight) (9), body mass index (ALST/BMI) (8), as well as the linear regression residuals method, when ALST is adjusted for height and body fat mass (residuals approach) (10). Thus, several studies have proposed ALST cut-off points to identify sarcopenia for different ethnicities (10 11 12 13 14-15).
In Brazil only one study proposed cut-off points from a DXA-measured ALST index to identify sarcopenia (16). However, it included only women and the young reference sample was small (n = 33), below the recommended size (n ≥ 100) (7). Other continental study, the SABE (Saúde, Bem-Estar e Envelhecimento), which involved seven big cities in Latin America and the Caribbean, was one of the largest longitudinal study with older people ever conducted in Brazil (17). The 25th and 10th percentiles of the ALST distribution in older adults were used as references for physical disability and frailty. Therefore, it had an epidemiological purpose and did not involve the diagnosis of sarcopenia as referenced in the young population. Furthermore, they used anthropometry measures to predict ALST (17), a tool not recommended by consensus for estimating SMM parameters for sarcopenia diagnosis purposes (2). To identify sarcopenia, the EWGSOP (2) and SCWD (7) recommend that ALST normative values for a population should be proposed from -2 standard deviations (-2SD) of their young adults. In this sense, other attempts to propose ALST cut-off points for Brazilian older individuals sought to identify this pathology using the linear regression residuals method (18 19-20). In this approach cut-off points are proposed based on the residuals (errors) between the values predicted and measured by DXA (21). Following the 2018 EWGSOP review, this type of analysis is no longer recommended (2). The ALST index measured by DXA is still the most widely used method in Brazil, but the cut-offs are based on international parameters (6), a practice that favors the occurrence of false positive cases for sarcopenia due to the existing variability of ALST between different ethnicities (22). Diagnosing healthy seniors as sarcopenic certainly may impact negatively the prioritization of treatments and the use of the available financial resources.
Therefore, the aim of this study was to propose ALST cut-off points from a young adult population of both sexes to identify sarcopenia in Brazilian older adults. The findings of this study may contribute to the advancement of epidemiological and health research on the impact of sarcopenia in Brazil.
MATERIAL AND METHODS
STUDY POPULATION
This was an observational study with a cross-sectional analysis of the original study data (23). Our sample derived from a larger study from our lab that involved 155 young university students (79 women) aged 18 to 30 years from the campus of Universidade de São Paulo, Brazil. Participants self-reported their ethnic group (brown, black, yellow or oriental, indigenous, white and hispanic) according to the classification of the Brazilian Institute of Geography and Statistics-IBGE (24). Recruitment (personal invitations, electronic dissemination, and university press) and study data collection took place from October 2016 to May 2017.
A sample size calculation was made to define the desired maximum error (e) and confidence level (Zy), previously knowing the population variability (s2) (25). For this purpose, data from a multiethnic study describing the ALST index of different populations were used as reference (22). The highest variability was observed for the ALST index of men over 18 years (SD = 2.35 kg). From the estimate of the predetermined error (e ≤ 1 %) and confidence interval (g = 0.95), the ideal n for our study was defined by the equation: n = [ZyDP/e]2(25). The minimum sample values for each gender (n = 22) were exceeded, even after applying the inclusion and exclusion criteria.
Inclusion criteria included: age between 20 and 30 years; not taking antidepressants or central nervous system stimulants; self-declaration of good health; no amputated body parts; not exceeding 10 hours of physical training per week. Exclusion criteria were defined as: discontinuity in the study, reporting pain in the limbs, or severe balance problems.
Our study was in agreement with the Helsinki Declaration. All participants volunteered for the study, were informed about the scope of the study, and provided their written consent. The study was approved by the Ethics Review Board at University Hospital, Ribeirao Preto School of Medicine, University of Sao Paulo (HC-FMRP/USP), Brazil, with CAAE number: 57511516.5.0000.5659.
PROCEDURES
All measurements were performed at the HC-FMRP/USP in the morning. Data collection took place in a single session, always performed by the same examiner for all measurements. Prior to the measurements, the participants were asked to empty their bladders. A DXA full-body examination was conducted with the participants wearing a disposable apron. After the exam anthropometric measurements were made according to the recommendations available in the literature (26).
MEASUREMENTS
Appendicular lean soft tissue (ALST)
ALST was measured by DXA (scanner Lunar GE Medical Systems - Prodigy Advance, software Encore, version 13.6), always by the same experienced technician. The variables of lean soft tissue (LST), fat mass, and bone mineral content were also measured. Before taking measurements the DXA device was calibrated as recommended by the manufacturer. The reliability records of the measurements were saved. The test-retest reliability evaluated in 11 subjects produced a coefficient of variation for ALST, LST, fat mass, and bone mineral content of 2.3, 0.8, 1.6, and 1.6 %, respectively. ALST was considered as the sum of the LSTs of the upper and lower limbs. The images of the limbs were isolated from the trunk and head with regional computer-generated default lines by the software, with manual adjustments by the technician when necessary. Specific anatomical landmarks were used following the manufacturer's manual to define the lower and upper limbs. Lower-limb LST was established as extending from a line drawn through and perpendicular to the axis of the femoral neck, and angled with the pelvic brim to the tips of the phalanges. Upper-limb LST was considered as extending from the center of the arm socket to the tips of the phalanges. ALST was considered in absolute form, and as ratio by squared height (ALST/height² [kg/m²]), which is designated the ALST index (2,7), by weight (ALST/weight), and by BMI (ALST/BMI).
Chronological age and anthropometric measurements
Chronological age was considered as the whole number of years. Body mass in kg was measured on a digital scale (Filizola®, personal model, Campo Grande, MS, Brazil) with an accuracy of 0.1 kg. Height in centimeters (cm) was measured in a fixed wall stadiometer with a precision of 0.1 cm. BMI was calculated by dividing body mass by squared height (kg/m²).
DATA QUALITY CONTROL
To ensure the quality of anthropometric measurements for body mass and height, the intra-evaluator technical error of measurement, both in absolute (TEM) and relative (TEM %) form, was assessed (27). Seven individuals were measured in duplicate. The TEM and TEM % values obtained were 0.05 kg and 0.09 % for body mass, and 0.35 cm and 0.21 % for height, respectively. TEM % values were within the recommended limits (< 1 %) (27). The other measures used in the study performed in our laboratory were within acceptable error limits (28).
STATISTICS
Central tendency measurements and 95 % confidence intervals were used to describe the sample. The normality of the ALST index variable was checked using the Kolmogorov-Smirnov test. Normality ensures that the proposed cut-off points are located at -2 SDs from the mean ALST of young individuals, according to the method proposed by Morley (7). All statistical analyses were performed separately for each sex using the SPSS version 20.0 (Chicago, IL, USA), with the previously established significance level (a = 5 %). This manuscript has been produced in accordance with the requirements of the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) checklist for cross-sectional studies.
RESULTS
Figure 1 shows the flowchart of recruitment progress through the analysis of the original study (2) and the current study data.

Figure 1. Flowchart showing theof young university students recruited in the original study and those included in the current study, Ribeirão Preto, Brazil, 2016/2017.
The descriptive analysis of all variables for both sexes is shown in table I. Women and men had a nutritional status classified as eutrophic, with an average BMI between 18.5 and 25.0 kg/m². However, 20 % of the sample was classified as being overweight (n = 25), and only 1.6 % as obese (n = 3). In the comparison between genders there were significant differences in all variables except age. Men had higher values for body mass, height, BMI, bone mineral content, LST, ALST, and ALST index. But they had lower values for fat mass when compared to women (p < 0.05).
Table I. Descriptive data of young university students from Ribeirão Preto, Brazil, 2016/2017, stratified by sex (n = 125)
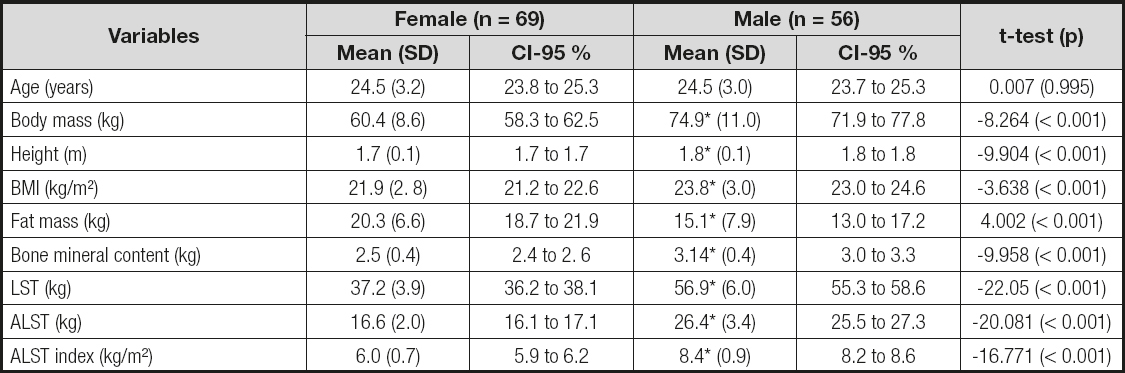
*p < 0.001 vs. female. SD: standard deviation; CI-95 %: 95 % confidence interval; p: statistical significance; BMI: body mass index; LST: lean soft tissue; ALST: appendicular lean soft tissue.
The self-reported ethnic frequencies of our university students of both sexes are shown in table II. Six racial groups were self-reported: brown, black, yellow (oriental), indigenous, white, and hispanic. There was a predominance of white ethnicity in both sexes. There were no differences in the proportions of each ethnicity in the comparison between sexes.
Table II. Absolute (n) and relative (%) frequency of self-reported ethnicities by university students from Ribeirão Preto, Brazil, 2016/2017, stratified by sex (n = 125)

p: statistical significance (female vs. male).
There were no differences in ALST between ethnicities for both genders: women (FANOVA= 0.447, p = 0.814) and men (FANOVA= 1.834, p = 0.137). There was a normal distribution of the ALST index by the Kolmogorov-Smirnov test for women (statistics = 0.075; p = 0.200) and men (statistics = 0.086; p = 0.200). This ensured that the proposed cut-off points were located at -2 SDs from average.
Figure 2 shows the ALST index distribution histogram for women (a) and men (b), respectively. In the center of the abscissa axis is the mean ALST index. The three values on the right/left represent the three positive/negative SDs, respectively. The ordinate axis shows the ALST index distribution frequency, more heterogeneous for women than men.
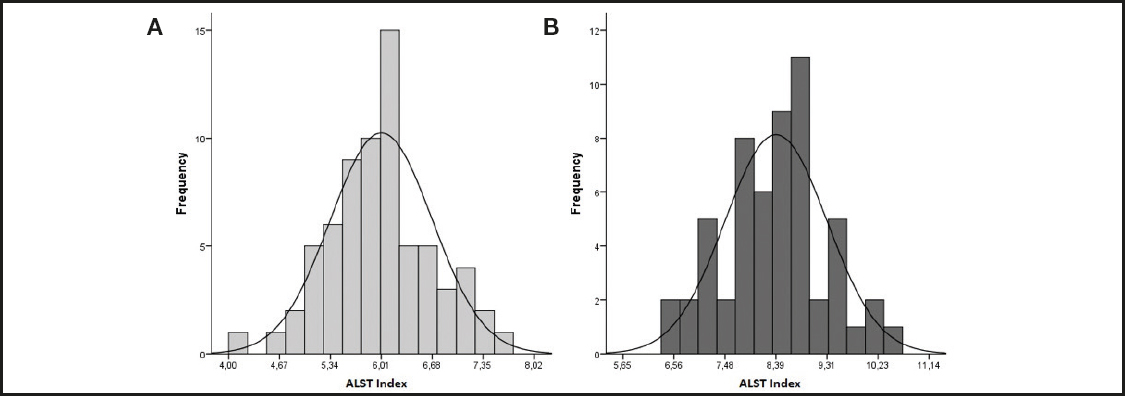
Figure 2. Histogram showing the frequency distribution of the ALST index among female university students in A (n = 69), and male students in B (n = 56), from Ribeirão Preto, Brazil, 2016/2017 (n = 125).
The ALST index cut-off points (-2SD) to identify sarcopenia in older adults as found in our study were ≤ 4.67 kg/m² for women and ≤ 6.56 kg/m² for men. For a more conservative diagnosis according to EWGSOP (≤ -2.5 SDs) (2), the values would be ≤ 4.33 kg/m² for women and ≤ 6.10 kg/m² for men.
Although in this study the ALST index was the approach adopted for proposing cut-off points,table III lists other ALST indicators (absolute and as ratio by body mass [ALST/weight] and BMI [ALST/BMI]) obtained from our sample. These indicators follow the criteria recommended by the EWGSOP (2) for cut-off points and eventual comparisons in Brazilians.
DISCUSSION
Our ALST index references to identify sarcopenia in female (≤ 4.67 kg/m²) and male (≤ 6.56 kg/m²) older adults in Brazil are markedly lower when compared to values reported in the international and national literature. Among the factors that may explain part of these differences in ALST are the intrinsic characteristics of each ethnicity; the methodological or statistical strategy used to propose the cut-off points; and the instruments/resources chosen to determine ALST measures. We will address the impact of these issues in the three following paragraphs.
The specific anthropometric and body composition characteristics of the reference population adopted in the international literature depend on the typical ALST value for each ethnicity (22). Considering average lifespan values, Asians have a lower ALST, followed by Hispanics, Whites, and African Americans (22). Differences remain even after weight or height adjustment (22). Thus, the EWGSOP recommends that each ethnicity have their own values defined, and referenced in their young population (2). We understand race as a person's physical characteristics (biological approach), while ethnicity is a person's cultural identity (social science concept). Even within the same race, in different ethnicities ALST values may vary. In Americans, for example, regarding ALST values with reference in adults 18 to 40 years (n = 229), cut-offs are 5.45 kg/m² for women and 7.26 kg/m² for men (11). In Australians (n = 682) of similar age (20-39 years) the cut-off points obtained were slightly lower at 5.30 kg/m² for women and 6.94 kg/ m² for men (13). These values are higher than those in our study for both sexes, with equally higher cut-off average values for the ALST index at ≤ -2 SDs (female = 4.67 kg/m²; male = 6.56 kg/ m²) and for ≤ -2.5 SDs (female = 4.33 kg/m²; male = 6.10 kg/m²).
Another determining factor of ALST cut-off values may be derived from the method used in their assessment. The method that considers ALST values ≤ -2 SDs from the average of young adults as sarcopenic is the most widely used in propositional studies (11,13,16). It is also highly recommended by consensus (2,7). Another less commonly used method for establishing ALST thresholds for both sexes considers the lowest 20th percentile from an older adult sample, very similar to the previous method (10,29).
ALST measurements vary among DXA device and equipment manufacturers, which may impact estimates. However, four different devices were compared and there were no differences between them besides a very high correlation (r ≥ 0.989) for ALST measurement (30). This confirms the validity of DXA for measuring ALST, although there are estimates using anthropometry. Three Brazilian studies (31 32-33) have suggested cut-off points for sarcopenia based on the total SMM estimated by anthropometric equationa (34). All considered the smallest quintile (< 20th percentile) to propose their cut-off points (6.37, 6.47 and 6.64 kg/m² for women, and 8.90, 8.76 and 8.83 kg/m² for men, respectively). They were larger as compared to our study for both sexes. However, this way of considering total SMM may overestimate cut-off values as they represent higher values when compared to ALST (74 % of total SMM) (35). Moreover, considering ALST thresholds for classifying SMM is a methodological error.
Among the strengths of our study, we followed all the recommendations by the SCWD and EWGSOP for proposing ALST cut-off points (2,7): the reference group should consist of healthy young adults aged 20 to 30 years; more than 100 subjects should compose the sample with the same ethnic characteristics as the older adults. In addition, young people should not have limb pain or severe balance problems (7), conditions ensured by the participants' self-declaration as healthy young adults. Sample losses after applying inclusion criteria had no influence on the final result of the study. Once the sample was analyzed for each gender (female = 69; male = 56), it exceeded the required number obatined from the sample size calculation for each gender (n = 22).
Early identification of sarcopenia in aging individuals enables more effective preventive interventions with an action plan for monitoring body changes in older adults and their functional performance (36). Sarcopenia is a chronic public health problem with a considerable economic impact (3). Financial investment in public policies to prevent and treat diseases may ensure future savings (37). This has a relevant impact on low- and middle-income countries such as Brazil, as the aging population will increase in coming years (38). By 2050 developing countries will have about 1.2 billion older people of an estimated 1.5 billion world total (38). Over the next 30 years an increase in new cases of sarcopenia by 63.8 % to 72.4 % is expected in Europe alone (39). Therefore, the highest accuracy in the diagnosis of sarcopenia should represent savings for public health both worldwide and in each country. Using estimates of total SMM to verify the incidence of sarcopenia, as is done in Brazil based on ALST index cut-off points, increases the chances of misdiagnosis since ALST is only about three quarters of the total SMM, as it represents only the muscular structures of the arms and legs (40). This raises the number of false positive cases. As an example of a false positive diagnosis, a hypothetical case can be shown: a Brazilian male with 19.7 kg in ALSTDXA and 1.70 m in height would have an ALST index of 6.82 kg/m². Using the international EWGSOP thresholds (≤ 6.94 kg/m²) this would be classified as low muscle mass, one of the criteria in the diagnosis of sarcopenia. However, when considering our thresholds (≤ 6.56 kg/m²), this criterion would not be confirmed. Even if he met the other criterion for the diagnostic confirmation of sarcopenia (low muscle strength), there would be no false positive result. Therefore, the use of appropriate references (cut-off points) with greater diagnostic accuracy in future studies of this nature would allow adequate estimates of the prevalence, incidence, and causes of sarcopenia. This will enable the development of more effective intervention strategies in the prevention and treatment of this disease.
The main limitation of this study involves a sample not representative of the real Brazilian population. Our data are regional and derive from a sample selected for convenience. However, there are no national reference values for Brazilians, and our study is the first one that meets the recommended criteria. Other international proposals generally do not adopt population stratification criteria or national representativeness, although there are studies with larger numbers of participants (13). Another limitation is the small racial representativeness of our sample, as for instance indigenous were not represented in the male group. Nevertheless, there was no statistical difference in our data when comparisons of ALST between races were made. There was also great ethnic variability in our sample, with evidence of the high racial miscegenation that is typical of Brazilian people.
CONCLUSION
This was the first Brazilian study to propose ALST cut-off points for the diagnosis of sarcopenia in older adults of both sexes using DXA. The international methodological and statistical requirements for this purpose were met in the present study. Thresholds are lower as compared to other international/national proposals. As well as the diagnosis of osteoporosis, the cut-offs were referenced in young adults. Our proposal represents an advance in the field of public health, facilitating the early diagnosis of sarcopenia and the best management of this disease that has harmful effects on geriatric populations. However, these cut-off points apply to older adults with similar characteristics to those in our study, and require caution in generalization, even when applied to other regions of Brazil. Therefore, validation is needed in the discrimination of relevant body components (visceral adipose tissue, intermuscular adipose tissue) or markers for metabolic risk, inflammation, and physical function.












 Curriculum ScienTI
Curriculum ScienTI


