INTRODUCTION
Cardiovascular disease (CVD) is the first cause of death and disability worldwide (1). Unhealthy diet is a leading risk factor for CVD where several studies indicated that excessive consumption of saturated fatty acids (SFA) increases the low-density lipoprotein (LDL) cholesterol, which may enhance the risk of developing CVD (1 2-3). Eckel et al. (2014) reported strong evidence that reducing SFA intake to 5-6 % of calories can be one important lifestyle modification for the management of CVD, mainly by lowering LDL cholesterol (4). However, several studies that evaluated the association of fat intake with CVD are controversial (5 6 7-8). Even though, for several decades, dietary guidelines have focused on the restriction of dietary cholesterol for heart health (5,6), numerous studies revealed that dietary cholesterol was not significantly associated with any coronary artery disease or ischemic stroke (7,8).
Epidemiological studies which examined the effect of monounsaturated fatty acids (MUFA) on CVD have shown mixed results. The Prevención con Dieta Mediterránea (PREDIMED) study reported that diets higher in MUFA reduced CVD events as compared with lower fat diets and, as a result, lowered the incidence of coronary heart disease (CHD) risk (9). Moreover, the Mediterranean dietary pattern, rich in MUFA, was recognized for its beneficial effects on CHD risk reduction in which a strong negative association was observed among followers of this dietary pattern and CHD risk (10). On the contrary, two metaanalyses of cohort studies found no significant association between MUFA and CHD events or death (11,12). Several studies investigated the effect of polyunsaturated fatty acids (PUFA) and the risk of CVD and the obtained results were conflicting (13 14-15). A meta-analysis of randomized controlled trials showed that the increase in PUFA intake actually reduced the risk of CHD death (14,16). However, some prospective cohort studies have shown that PUFA increased the risk of cardiovascular outcomes (13) or were not associated with risk (15).
Consumption of trans-unsaturated fatty acids was associated with a 34 % increase in all-cause mortality, 28 % increased risk of CHD mortality, and 21 % increase in the risk of CHD (17). However, no associations were observed for ruminant trans-fat with CHD (17).
This study aimed to explore the association between fat intake and the CVD risk in Jordan using a case-control design where a limited number of studies concerning risk factors for CVD has been published from the Middle East Countries. The concluded findings of this study would be of great importance for enhancing the public recognition about fat intake as a risk factor to develop CVDs. Those results could be used as a guidance to direct policy makers to initiate targeted nutritional and lifestyle strategies to prevent CVD events and alleviate their consequences. Also, those results could be used to establish more specified dietary guidelines regarding the intake of trans-fats and saturated fats for Jordanians.
SUBJECTS AND METHODS
PARTICIPANTS AND STUDY SETTING
A case-control study was conducted to assess the association between fat intake and CVD risk among Jordanians. Participants of the present study were enrolled conveniently from the catheterization section of the Cardiology Department of Prince Hamzah Hospital, a referral hospital in the capital Amman, between January and December 2015. A total of 399 participants who underwent coronary angiography were included. The cases and controls were age and gender matched with 1:1 ratio. Participants with kidney disease, liver disease or gastrointestinal diseases were excluded. All participants were requested to sign a written consent form to participate in the study. The study protocol was designed according to the ethical guidelines of the 1975 Declaration of Helsinki, and the study was approved by the Institutional Review Board Ethics Committee at Prince Hamzah Hospital. One day before undergoing coronary angiography, all data were collected from patients upon filling a standardized questionnaire by trained dietitians to record socio-demographic factors, previous health issues (hypertension, diabetes mellitus, dyslipidaemia), smoking status, and family history of CVDs information.
CORONARY ANGIOGRAPHY
Seldinger technique was used to insert a catheter by trained cardiologists into the radial artery, and the tip was advanced to the aortic sinus cusp. To visualize the arterial tree, X-ray images of the transient radio-contrast distribution within the coronary arteries were carried out. The degree of obstruction was estimated as percentage of the arterial lumen by comparing the area of narrowing to an adjacent normal artery. Consistent with prior studies, CAD was defined as ≥ 20 % stenosis of one or more coronary arteries (18,19). Participants with no stenosis (0 %) were enrolled as controls.
NUTRIENTS INTAKE ASSESSMENT
A validated Arabic quantitative food frequency questionnaire (FFQ) was used to assess the dietary intake pattern (20). The information dealing with dietary history of participants was investigated in the FFQ questions. During face-to-face interviews, the participants were asked to record how frequently, on average, they had consumed one standard serving of specific food items in nine categories (< 1/month, 2-3/month, 1-2/week, 3-4/week, 5-6/week, 1/day, 2-3/day, 4-5/day, or 6/day) during the past year. Food lists in the modified FFQ questions were classified based on types of food: 21 items of fruits and juices; 21 items of vegetables; eight items of cereals; nine items of milk and dairy products; four items of beans; 16 items of meat such as red meat (lamb and beef), chicken, fish, cold meat, and others; four items of soups and sauces; five items of drinks; nine items of snacks and sweets; and 14 items of herbs and spices. Food models and standard measuring tools were used for better estimation of portion size. Dietary analysis software (ESHA Food Processor SQL version 10.1.1; ESHA, Salem, OR, USA) was used to analyze dietary intakes with additional data on foods consumed in Jordan. After entering the amounts which were consumed daily from the raw fats, foods containing fats, fried foods and other foods to the ESHA program, total amounts of different fats were added and calculated. Recipes for Jordanian foods were entered and the total intake from these recipes was calculated. Energy (kcal), energy from fat (kcal), energy from saturated fat (kcal), energy from trans fatty acids (kcal), % of fat, fat (g), SFA (g), MUFA (g), PUFA (g), trans fat (g), cholesterol (mg), omega-3 (g), omega-6 (g), omega-3:omega-6, oleic (18:1) (g), linoleic (18:2) (g), lonolenic (18:3) (g), eicosen (20:1) (g), arachidon (20:4) (g), eicosapentaenoic acid (EPA) (20:5) (g), and docosapentaenoic acid (DPA) (22:5) (g) intake was assessed from the whole food items which are included in the used FFQ.
7-DAY PHYSICAL ACTIVITY RECALL (PAR)
A 7-day PAR validated questionnaire, which is an organized questionnaire, was used to calculate a participant's recall of time spent participating in exercise over a seven-day period (21). This questionnaire helps to divide individual physical activity levels into three categories. Participants were asked to respond to a PAR question based on the way they used to behave prior undergoing coronary angiography.
ANTHROPOMETRIC MEASUREMENTS
All anthropometric measurements were carried out by a trained dietitian. Body weight was measured to the nearest 0.1 kg, with minimal clothing and without shoes, using a calibrated scale (Seca®, Hamburg, Germany). Height and waist circumference were measured to the nearest 1 cm with participants in standing position without shoes using a calibrated portable measuring rod. Body mass index (BMI) was calculated as weight (kg) divided by height square (m2).
STATISTICAL ANALYSIS
SPSS version 20.0 software (SPSS Inc., Chicago, IL, USA) was used to perform the statistical analysis. The significance level was set at p ≤ 0.05. Mean ± standard error of mean (SEM) and percentages were used for descriptive statistics. To evaluate the differences between cases and controls in continuous variables, t-tests were used, and Chi-squared was used to detect the differences among categorical variables. Potential confounders (age, gender, BMI, smoking, physical activity, total energy intake, occupation, education level, marital status and family history) were chosen based on reported risk factors for CVDs. The quartiles were calculated using the cut-off points at 25, 50 and 75 % of total nutrients intake. The first quartile was determined if the intake was below 25 %, while the second one was determined if the intake was between 25-50 %. The third quartile was between 50-75 % and the fourth was above 75 %. Multinomial logistic regression model and linear logistic regression model were used to calculate odd ratios (OR) and its 95 % confidence interval (CI) and p-for-trend for trend, respectively. The energy adjustment was performed using the residual method of Willett in which residuals were computed from a regression analysis (22).
RESULTS
Briefly, 239 males and 160 females participated in this study. The study participants' characteristics are shown in table I and have been as mentioned elsewhere (23). The main characteristics of study subjects categorized by gender are summarized in table I. The cases had higher mean fasting blood glucose levels compared to controls. Moreover, cases showed higher blood triglyceride levels compared to controls. In addition, there were differences in physical activity measured as MET (min/week). Overall, the cases were less active compared to controls, and reported more previous health problems than controls, in both men and women.
Table I. General characteristics of study participants based on gender

*Significant difference was set at p < 0.05. SEM: standard error of mean; BMI: body mass index; MET: metabolic equivalent-minutes; LDL: low-density lipoprotein; HDL: high-density lipoprotein; CAD: coronary artery disease.
Table II reveals that no significant difference was detected between cases and controls in all types of fat intake either before or after energy adjustment. Also, the percentage of fat intake from total energy was within the recommended level. However, the amount of saturated fat (around 30 g; 9.0 %) was close to the amount of MUFA (around 33 g; 10.5 %) which is not consistent with a healthy diet. On the other hand, the intake of PUFA (19 g; 6.0 %) was lower than both saturated and MUFA. The consumption of cholesterol was below the recommended amount (intake: 255 mg vs recommended: 300 mg). Oleic fatty acid was the prominent type of fat among the cases and controls. Additionally, the intake of omega-6 and omega-3 among cases and controls was in agreement with the recommended amounts.
Table II. Fat and type of intake of cases and controls before and after the adjustment of energy intake
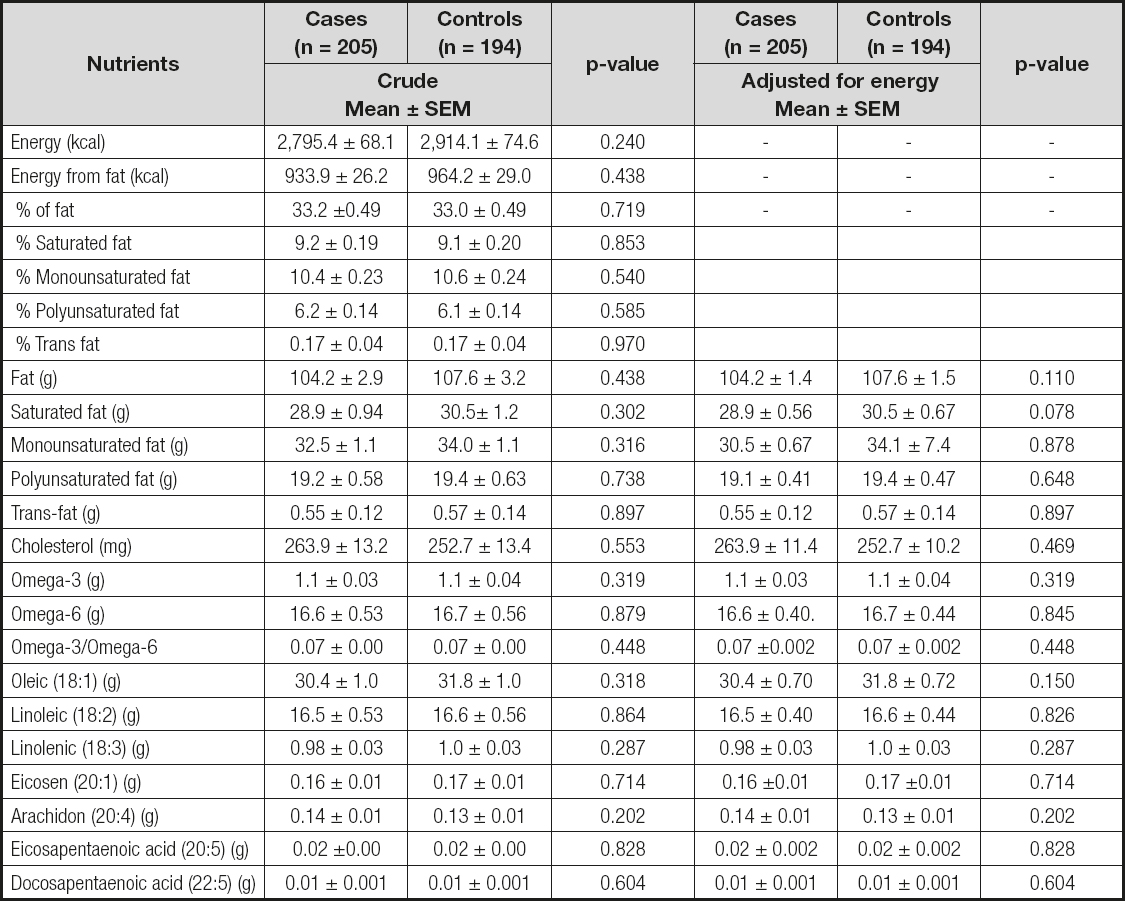
Table III shows the crude and adjusted ORs and their 95 % CI for CVD by fat types quartiles. OR and their 95 % CI for fat types were adjusted for age, gender, BMI, smoking, and physical activity. The intake of all fat types (except trans-fat) was not associated with the risk of developing CVD. Trans-fat intake in the second and third quartile increased the risk of CVD by adjusted for about 1.86 (95 % CI: 1.03-3.34) and 2.01 odds (95 % CI: 1.12-3.60), respectively. Similar results of the association between trans-fat and CVD obtained was obtained for the crude OR.
DISCUSSION
This study aimed at evaluating the association between the intakes of different fat types and the development of CVD among Jordanians. Due to the discrepancy in the findings of multiple studies, the research is still unclear to judge if there is really a positive association between SFA and CVD, as traditionally speculated. The main findings of this study did not support the results of many other studies which stated that total dietary fats, saturated fats and cholesterol were positively associated with the risk of developing CHD (12,24,25). However, our findings came in agreement with several other studies (17,25,26). De Souza et al. (2015) reported null associations between saturated fat intake and all-cause mortality (relative risk 0.99, 95 % CI: 0.91 to 1.09), CVD mortality (0.97, 0.84 to 1.12), total CHD (1.06, 0.95 to 1.17), ischemic stroke (1.02, 0.90 to 1.15), and type 2 diabetes (0.95, 0.88 to 1.03) (17). Siri-Tarino et al. (2010) illustrated that the intake of saturated fat was not associated with an increased risk of CHD, stroke, or CVD; the pooled relative risk estimates that compared extreme quantiles of saturated fat intake were 1.07 (95 % CI: 0.96, 1.19; p = 0.22) for CHD, 0.81 (95 % CI: 0.62, 1.05; p = 0.11) for stroke, and 1.00 (95 % CI: 0.89, 1.11; p = 0.95) for CVD (25). Additionally, Harcombe et al. (2016) revealed that none of the studies included in their meta-analysis found a significant relationship between CHD deaths and total dietary fat intake (26). Factors such as food matrix, source of saturated fat, and fatty acid chain length may influence the health effects of saturated fats and therefore, might explain the contradiction in the current evidence regarding their association with CVD (27,28).
Although the 2015-2020 Dietary Guidelines for Americans recommend substituting both MUFA and PUFA for saturated fats, the consistency in the current evidence is lacking (27,28). Higher intakes of PUFA were found to be significantly associated with a lower risk of CHD comparing the highest and lowest quintile for PUFAs 0.80, (0.73 to 0.88; p-trend < 0.0001) (29). On contrary, Chowdury et al. (2014) reported no relationship between dietary PUFA and coronary disease, with a risk ratio 0.98 (CI: 0.90 to 1.06) in eight cohort studies containing 206,376 participants with 8,155 events (12). The proportions among daily intake of different types of fat might provide a partial explanation for the inconsistent evidence concerning the association of unsaturated fats with CVD (30,31); the optimal balance among daily intake of different fatty acids can effectively improve the health while the incorrect ratio may increase disease risk (30,31). Here, no significant association was detected between the intake of PUFA, MUFA, omega-6 or omega-3 and CVD risk among cases and controls. Two main reasons might have contributed to the null findings; firstly, our study findings revealed that the intake of PUFA (around 19 g/day; 6.0 %), MUFA (around 32 g/day; 10.5 %), omega-6 fatty acid (16 g/day) and omega-3 fatty acid (1.1 g/day) was similar in cases and controls. Secondly, all of these types of fat were consumed in approximately the recommended doses (32).
Trans-fat intake was found to be significantly associated with CVD among Jordanians, which is consistent with many studies (12,33). Trans-fats from foods may adversely affect the risk of coronary disease by raising LDL cholesterol levels and lowering high-density lipoprotein (HDL) cholesterol levels (34), increasing Lp(a) lipoprotein levels (34), raising triglyceride levels (34), and interfering with essential-fatty acid metabolism (35). Trans-fats were associated with all-cause mortality, total CHD, and CHD mortality, probably because of higher levels of intake of industrial trans-fats than of ruminant trans-fats (17). Industrial and ruminant trans-fats consist of the same positional trans isomers, but in different proportions. The isomer profile depends on conditions of hydrogenation, such as catalysts used and temperature of hydrogenation for industrial trans-fats and rumen pH, and the composition of oils in the diet for ruminant trans-fatty acids (36). Chowdhury et al. (2014) revealed in their meta-analysis that the intakes of SFA, MUFA, alpha-linoleic acid, long-chain omega-3 or omega-6 fatty acids were not associated with coronary disease (12). However, they found that trans-fats increased the incidence of coronary disease (RR 1.16, 95 % CI: 1.06 to 1.27) (12). Li et al. (2015) studied 84,628 women (Nurses' Health Study, 1980 to 2010) and 42,908 men (Health Professionals Follow-up Study, 1986 to 2010) who were free of diabetes, cardiovascular disease, and cancer at baseline, and found that trans-fat intake was significantly associated with an increased risk of CHD (HR: 1.20, 95 % CI: 1.09 to 1.32; p-trend = 0.002) (29). It has been estimated that the consumption of about 5 g of trans-fat per day is associated with 25 % increase in the risk of CHD (29). Although the association between CVD and trans-fat appears to be causal, no randomized controlled trial with hard endpoints has been reported (37).
Regarding cholesterol findings, our results showed no significant association between the intakes of cholesterol and CVD risk, with insignificant difference in the mean intake of cholesterol for cases compared to controls. McNamara (2000) demonstrated in his review that the analysis of the available epidemiological and clinical data indicated that, for the general population, dietary cholesterol makes no significant contribution to atherosclerosis and risk of cardiovascular disease (38). A recent study of Rhee et al. (2017) performed on 30,068 participants (mean age 40.8 years; 84.5 % men) in a health screening program in Korea documented that dietary cholesterol intake did not show any association with LDL level or with risk for coronary artery calcification in apparently healthy Korean adults (39). The Scientific Report of the 2015 Dietary Guidelines Advisory Committee (DGAC) in the United States concluded that “cholesterol is not a nutrient of concern for overconsumption”, suggesting that there no longer be a recommended upper limit for dietary cholesterol intake (40). This conclusion came after decades of the recommendation of 300 mg/d as the upper limit for dietary cholesterol. Despite eliminating the upper limit from the Dietary Guidelines, individuals should eat as little dietary cholesterol as possible as part of their healthy eating pattern to hinder CVD risk. Therefore, the lack of association between the dietary cholesterol and CVD in the current study could be due to the considerable low daily consumption of cholesterol (< 300 mg/day) for both cases and controls.
The main strength points of this study are the use of a validated Arabic FFQ that was modified to reflect the food consumption pattern in Arab countries, especially Jordan, as well as the use of food models and measuring tools to estimate portion sizes. There are limitations in this study; for example, the one year dietary recall period may not be an accurate amount of time in which to conclude that an association exists between fat intake and CVD development. Nevertheless, we believe that the recall period of one year is very likely reflective of the previous years. Thus, the association between fat dietary intake and CVD may have been developing for several years.
In conclusion, no association has been found between cholesterol, saturated fats, PUFA and MUFA and the risk of CVD. On the contrary, a significant association has been detected between trans-fats and the development of CVD. This may be attributed to the fact that the intake of most of these fat types (except trans-fats) are within the recommended percentages and amounts.















