INTRODUCTION
The prevalence of obesity in children has increased all over the world (1,2), and has been declared a global public health problem (3). In fact, South American countries have shown greater increases in the prevalence of obesity in girls and boys (4). Preventing early obesity is one of the major concerns in the last years due to its association with cardiometabolic risk (CMR) factors (5) and various negative psychological factors (6). Many factors influence the development of obesity in schoolchildren, some of which are changes in lifestyle (i.e., physical activity (PA) patterns, sedentary behaviours, and nutritional level) (7). In this sense, a healthy lifestyle (8), including daily PA patterns, low screen time (ST) per day, and healthy food habits (i.e., the inclusion of daily water, fibres, fruits, and vegetables) are key targets for the prevention of CMR in children (9).
On the other hand, a good lifestyle is a modifiable factor that is inversely associated with obesity and CMR (10). The relevance of this is that, if carried on since childhood, it may influence the adoption of an active lifestyle (11), and prevent CMR (12); therefore, the study of the factors that influence lifestyle in children is a priority and needs to be carried out in depth. In this respect, some emotional states in children affect their lifestyle, as PA patterns and foods habits (13). Likewise, emotions such as loneliness, sadness, and social isolation are increasingly being acknowledged as risk factors for physical and mental health problems (14), and have been associated with unhealthy lifestyles in older and younger individuals (15), illustrating the importance of considering emotions as lifestyle factors. However, the relationship between different aspects, such as perceived health-related quality of life (HRQoL) and emotions (i.e., sadness and loneliness) with lifestyle (i.e., PA, ST, and nutritional level), remains unclear in children and needs to be studied deeply, since they are variables that are associated with obesity and CMR. Therefore, the objective of the present study was to determine the association between feelings and lifestyle (i.e., PA patterns and nutritional level) and, as secondary objective, to determine the association of HRQoL and lifestyle with obesity and CMR in Latin American schoolchildren.
MATERIAL AND METHODS
This cross-sectional study included a sample of 634 schoolchildren (girls (n = 282), 11.8 ± 0.8 years, boys (n = 352), 12.0 ± 0.8 years)) from primary public schools in Chile. Parents and guardians signed written consent forms for participation, and all schoolchildren gave their written assent on the day measurements were made.
Inclusion criteria were as follows; a) registered in the study educational centres; b) attends classes regularly, and c) age between 10 and 13 years. Exclusion criteria included: a) presence of musculoskeletal disorders; b) diagnosis of intellectual disabilities; c) any other known medical condition that might impact the participant’s health status and PA levels; d) did not complete all the planned measurements of the study; and e) absent on the day of the evaluation. The present study was carried out in accordance with the Declaration of Helsinki (2013), and was approved by the Local Ethics Committee (DFP16-0013. Project).
HEALTH RELATED TO QUALITY OF LIFE
The KIDSCREEN-10 was used to measure HRQoL and different feelings and behaviours (i.e., sadness, loneliness, and school behaviour). The questionnaire is a validated and widely used assessment tool, developed for monitoring overall HRQoL in children and adolescents (8 to 18 years of age). The KIDSCREEN-10 has 10 items, each answered on a five-point Likert scale indicating the frequency of a specific behaviour or feeling (1 = never; 2 = almost never; 3 = sometimes; 4 = almost always; and 5 = always) or the intensity of an attitude (1 = not at all; 2 = slightly; 3 = moderately; 4 = very much; and 5 = extremely). The responses to items 3 and 4 (negatively formulated) were recoded to have scorings from 1 to 5; the raw scores were used for different analyses. Higher values indicated a higher HRQoL (16) .
THE CHILDREN’S FOOD HABITS
The children’s food habits were assessed with the Krece Plus test (17), which is a tool to assess eating patterns and their relationship with nutritional status based on the Mediterranean diet. The form assesses a set of items concerning the diet being consumed. Each item has a score of +1 or -1, depending on whether it approximates the ideal of the Mediterranean diet. Total points are summed, and according to the score obtained the nutritional status is classified as follows: 1) Less than or equal to 5: low. 2) From 6 to 8: moderate; 3) Greater than or equal to 9: high.
SCREEN TIME AND PHYSICAL ACTIVITY AFTER SCHOOL
Lifestyle was evaluated with the Krece Plus test (17). The Krece Plus is a quick questionnaire that classifies lifestyle based on the daily average of hours spent watching television or playing video games as screen time, and the hours of PA after school per week. The classification is made according to the number of hours used for each item. The total points are then added, and the person is classified as having a good lifestyle (men: ≥ 9, women ≥ 8), regular lifestyle (men: 6-8: women: 5-7), or bad lifestyle (men: ≤ 5 and women: ≤ 4) according to the lifestyle score.
ANTHROPOMETRIC ASSESSMENT
The participants’ body mass (kg) was measured using a TANITA scale (model Scale Plus UM – 028, Tokyo, Japan); measurements were performed in light clothing, without shoes. Height (m) was estimated with a SECA™ stadiometer (model 214, Hamburg, Germany) graduated in mm. The body mass index (BMI), calculated as the body weight divided by the square of the height in metres (kg/m2), was used to estimate the degree of obesity. BMI is shown in the growth table of the Centers for Disease Control and Prevention, Overweight and Obesity (CDC), verifying the corresponding age and the sex-related percentile. Child obesity was defined as a BMI equal to or greater than percentile 95th and overweight as a BMI equal to or greater than percentile 85th among children of the same age and sex (18,19). Waist circumference (WC) was measured using a similar SECA™ stadiometer (model 214, Hamburg, Germany) equipment at the anatomic point of the umbilical scar (20).
CARDIOMETABOLIC RISK FACTORS
CMR was evaluated using the waist-to-height ratio (WtHR). The WtHR was calculated by dividing WC by height, with values ≥ 0.5 representing CMR according to international standards (21).
STATISTICAL ANALYSIS
The statistical analysis was performed using the Stata package, version 13.0 (Stata Corp, College Station, TX, USA). Continuous variables were expressed as median and percentile (5th-95th). Differences between sexes were determined using the Mann-Whitney test. Qualitative variables were expressed as proportions and compared between groups with the chi-squared test. To determine the association between feelings, lifestyle, and CMR an odds ratio (OR; with 95 % CI) was used. Besides, an interaction model was assessed between low nutritional level combined with bad lifestyle and CMR.
RESULTS
The characteristics of the study sample are shown in table I. According to weight status 25.2 % had overweight and 22.4 % had obesity. Likewise, 32.2 % reported CMR (WtHR ≥ 0.5). The nutritional level was mostly moderate (47.0 %). Boys reported a higher proportion of bad lifestyle when compared to girls (boys: 65.34 % vs girls: 53.9 %).
Table I. Characteristics of the study sample regarding anthropometric parameters, lifestyle, and HRQoL

The values shown are median (percentile 5-95), p-value, number (proportions) and Chi2. BMI: body max index; WC: waist circumference; WtHR: waist-to-height ratio; BF: body fat; PA: physical activity; HRQoL: health-related quality of life.
The items in the KIDSCREEN 10 questionnaire and risk categories for nutritional level, bad lifestyle, obesity, and CMR are explored in table II. Likewise, items that exhibited significant associations are shown. The schoolchildren that had felt sad (Q: Have you felt sad?) presented an association with low nutritional level (OR: 4.26, 95 % CI: 2.0-9.0, p < 0.001), bad lifestyle (OR: 2.14, 95 % CI: 1.0-4.54, p = 0.048) and obesity (OR: 2.0, 95 % CI: 0.89-4.54, p = 0.09). Moreover, schoolchildren that had felt lonely (Q: Have you felt lonely?) reported an association with low nutritional level (OR: 4.47, 95 % CI: 2.5-7.9), p < 0.001), bad lifestyle (OR: 1.78, 95 % CI: 1.01-3.1, p = 0.045), and obesity (OR: 2.05, 95 % CI; 1.04-4.0, p = 0.037). The schoolchildren that had had enough time for themselves (Q: Have you had enough time for yourself?) reported the highest association with bad lifestyle (OR: 0.69, 95 % CI: 0.47-1.02, p = 0.06), obesity (OR: 0.36, 95 % IC: 0.22-0.58, p < 0.001) and CMR (OR: 0.50, 95 % CI: 0.38-0.83, p = 0.005). In relation to the question “Have you been able to pay attention?”, the schoolchildren that answered seldom-never presented the highest association with bad lifestyle (OR: 4.64, 95 % CI: 72-12.56, p = 0.002).
Table II. Association between perceived HRQoL (KIDSCREEN-10 items) and low nutritional level, bad lifestyle, obesity, and abdominal obesity
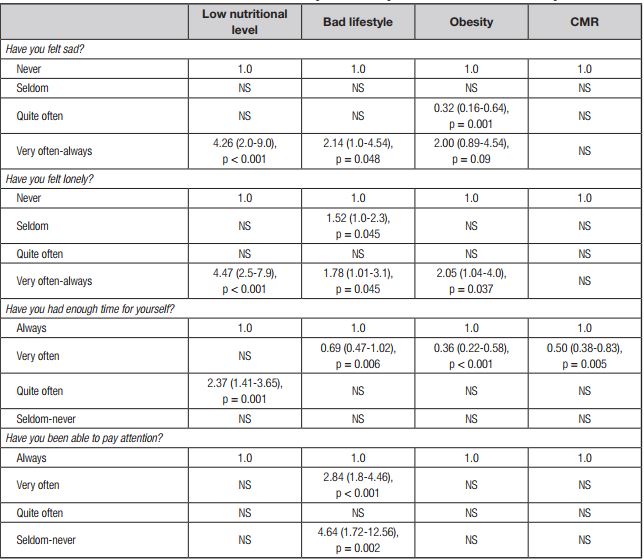
The data shown represent OR (95 % CI), p-value. p < 0.05 was considered statistically significant. Adjusted for age and sex. NS: not significant.
The distribution of the weight status category was evaluated in relation to nutritional level and lifestyle. A greater distribution of overweight, obesity and CMR (WtHR ≥ 0.5) was observed in schoolchildren with low nutritional level and bad lifestyle (Fig. 1A, Fig. 1 Fig. 1B).
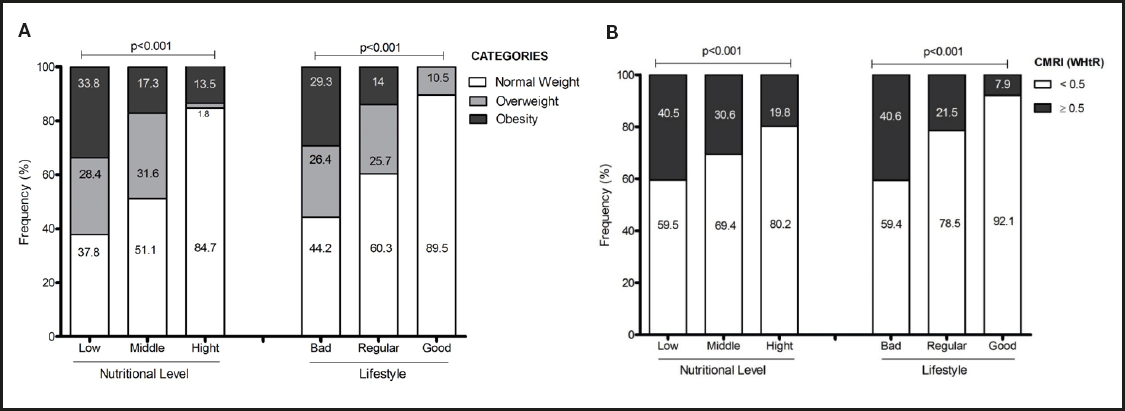
Figure 1. A. Weight status according to nutritional level and lifestyle. B. Cardiometabolic risk factors (WtHR ≥ 0.5) according to nutritional level and lifestyle.
Table III shows the association of variables. A bad lifestyle had the highest association with CMR (OR: 8.08, 95 % CI: 2.43-26.8, p = 0.001). Likewise, low nutritional level was associated with CMwR too (OR: 2.73, 95 % CI: 1.58-4.7, p < 0.001). An interaction model between low nutritional level and bad lifestyle was carried assessed; this model showed an association with CMR (OR: 2.6, 95 % CI: 1.76-3.84, p < 0.001).
DISCUSSION
The objective of the present study was to determine the association between feelings and lifestyle (i.e., PA patterns and nutritional level); a secondary objective was to determine the relationship of HRQoL and lifestyle with obesity and CMR in Latin American schoolchildren. The main findings were: a) a negative self-perception (i.e., sadness and loneliness) was associated when schoolchildren were classified in the bad lifestyle, low nutritional level, and obesitycategories; b) ST had the highest association with CMR; c) the interaction between low nutritional level and bad lifestyle showed a high and significant association with CMR. The evidence reports the importance of a healthy combination of lifestyle behaviours in childhood, including low ST, good PA patterns (i.e., daily PA) and healthy eating pattern (i.e., inclusion of vegetables and fruits) (7), whereas the results of the present study reported that perceptions of HRQoL as sadness and loneliness are associated with these behaviours.
In relation to HRQoL, the schoolchildren who expressed having felt sadness and loneliness reported an ssociation with unhealthy lifestyles. In this line, children appeared to engage in emotional eating (i.e., eating in response to negative and positive emotion). In this sense, a study showed that children’s snack food consumption varied across emotional valences, revealing how happiness and sadness can shape children’s eating patterns (22). Likewise, an investigation that examined the associations among self-reported loss-of-control eating, emotion dysregulation, body mass, and objective energy intake among the youth, reported that emotion dysregulation may play a role in energy intake and obesity (23), and negative emotions pose a major threat to public health by increasing the risk of obesity (24). In the same way, in children stress stimulated eating in the absence of hunger, which could facilitate overweight (13). However, a study reported that emotional problems and school attendance did not show any significant correlation with BMI (25), results that differ from those of the present study.
On the other hand, schoolchildren that reported having enough time for themselves exhibited an association with bad lifestyle (i.e., high ST and low PA) and low nutritional level (i.e., Mediterranean diet adherence). These points are very important as parents are models of PA patterns and eating habits (i.e., lifestyle models) for children and need to be present in their lifestyle development and formation. In line with that, a study performed in children provided confirmation of the important influence that parents exert on their children’s PA behavior (26). Furthermore, parents’ encouragement and support can increase their children’s PA (27). Likewise, a study showed that more active mothers have more active children, and the authors also concluded that family-based PA remains an important element of children’s activity behavior regardless of age (28).
In line with that, the schoolchildren that said they had not been able to pay attention showed the highest association with bad lifestyle, that is, they had the highest ST and lowest PA after school. Evidence showed that PA has also been found to have positive effects on academic achievement and cognitive functioning (29). Along this line, a before-school PA intervention improved cognitive function (i.e., attention and memory) in Chilean schoolchildren (30). On the other hand, an investigation showed that the association between PA and cognitive function (i.e., working memory) was intensity-dependent as significant findings were only observed for vigorous PA (31). Likewise, other study showed that the components of executive function (i.e., inhibitory control, working memory, and cognitive flexibility) were more strongly related to physical fitness than to PA in males and females (32).
In schoolchildren ST (≥ 2 h/day) was associated with CMR; likewise, 5 h/day of ST showed the highest association with CMR. Similar results have been reported, for example, by a study carried out in adolescents that found that participants with prolonged ST had the highest levels of glucose and non-HDL-C. The authors concluded that higher levels of PA appeared to be more important than low levels of ST for CMR (33). Likewise, another investigation reported that ST was positively associated with CMR in overweight/obese adolescents (34). In this line, a previous study found that students with high ST levels had significantly higher anthropometric parameters including BMI and WC; furthermore, the findings of this study showed that the joint association of high ST and low PA is directly associated with abdominal obesity and overweight (35). Nowadays, despite accumulating evidence linking ST with poorer health outcomes among children, this prevalence continues to increase (36); consistent with that, a study showed that children with over 3 hours of ST had higher fat mass and insulin resistance than peers with lower levels of ST (37).
In our sample schoolchildren with low nutritional level showed an association with obesity and CMR. Consistent with that, a study carried out in adolescents found that higher intakes of fruit and non-starchy vegetables, dairy products, and grains were independently associated with having fewer CMR factors; likewise, the authors concluded that healthy food consumption patterns during adolescence may prevent CMR (12). Likewise, an investigation performed in Chinese schoolchildren reported that several dietary factors, such as sugar consumption, were significantly correlated with CMR (38). Along these lines, a previous study that included a prospective analysis with data from baseline and both 7- and 10-year follow-up reported that adherence at 7 years of age to a dietary pattern rich in energy-dense foods and processed meat, and low in vegetables, may increase several CMR factors at 10 years of age (39). Furthermore, an investigation that used longitudinal observations made over a period of 2 years among 448 students reported that a reduction in the consumption of total dietary fat and sodium may contribute to the prevention of excess body weight and hypertension in children and younger people (40).
LIMITATIONS
This study has some limitations. Although we used standardized PA questionnaires, we did not use accelerometer devices, which would have provided the more precise quantification of PA and sedentary behavior as ST. The strengths of this study include that we examined several variables associated to CMR in children, as lifestyle and self-perception of HRQoL, that contribute to a better understanding of the serious problem of physical inactivity and childhood obesity.
CONCLUSION
In conclusion, Latin American schoolchildren who had felt sadness and loneliness (i.e., negative feelings) reported unhealthy lifestyles (i.e., lower nutritional level, more ST exposure, and low PA), obesity, and thus a higher burden of CMR. Therefore, perceived HRQoL (i.e., feelings reported in KIDSCREEN-10) are an important tool that should be considered to prevent early unhealthy lifestyles and CMR in schoolchildren.















