INTRODUCTION
Malnutrition can affect up to 50 % of hospitalized patients and is one of the main public health problems in developing countries. However, when malnutrition is not neglected by healthcare professionals, unfavorable clinical outcomes can be prevented 1).
Longer hospital stays, increased costs, impairment of the immune system, increased risk of pressure injuries, post-surgical complications, increased number of infections, delayed recovery, and increased risk of mortality are well-described consequences of malnutrition in the literature (1,2).
Thus, nutritional screening must be performed using validated tools, followed or not by detailed nutritional assessment, within 48 hours of patient admission in order to enable the multidisciplinary team to maintain a more assertive clinical approach and adequate clinical management (1).
The Patient-Generated Subjective Global Assessment (PG-SGA) instrument, available in Portuguese and culturally adapted to Brazil, is one of the most widely used subjective tools for patient screening and nutritional evaluation (3,4).
In addition to PG-SGA, objective methods such as conventional anthropometry are indicated for screening malnutrition. Among the most commonly used and available methods, especially in public hospitals, body mass index (BMI), calf circumference (CC), arm circumference (AC), tricipital skinfold (TSF), arm muscle circumference (AMC), and adductor pollicis muscle thickness (APMT) stand out (1).
Recently, APMT has emerged as an alternative nutritional status assessment as it is a direct measure, independent of adipose mass, and unaffected by hydration status. Moreover, APMT is a non-invasive, low-cost, easily applicable bedside method (5,6).
In the same way, handgrip strength (HGS) has also emerged as a highly used parameter by various healthcare professionals. Recently, HGS has been shown to be useful for assessing nutritional and functional status, especially in hospitalized patients (7).
Thus, considering the increasing need for improved nutritional care within hospitals, and the need to enhance the clinical prognosis of patients hospitalized for clinical and/or surgical procedures, this study aimed to assess whether APMT and HGS were correlated with conventional anthropometric variables in hospitalized patients, and to assess their relationship with nutritional status as determined by PG-SGA.
METHODS
STUDY DESIGN
A cross-sectional study with a non-probabilistic convenience sample design was conducted from June 2019 to September 2019 at the Department of Internal Medicine and Surgery at a University Hospital in Brazil.
ELIGIBILITY CRITERIA
Patients of both sexes admitted to the clinical or surgery ward within 48 hours of admission, aged 50 years or older, who were able to answer all PG-SGA items were invited to participate in this study. All patients signed an informed consent form after being consulted and informed about the research objective.
The following exclusion criteria were adopted: patients under respiratory precaution, with edema in the hands, with cognitive deficits, neurodegenerative diseases, rheumatic conditions or serious psychiatric disorders and indigenous population.
SOCIODEMOGRAPHIC AND CLINICAL CHARACTERISTICS
Sociodemographic variables were age, marital status, work status, and economic class according to the Brazilian Economic Classification criteria of the Brazilian Association of Research Companies (ABEP) (8).
The following clinical variables were assessed in the medical records of patients: clinical diagnosis, reason for hospitalization (clinical/surgical), and previous chronic diseases - diabetes mellitus, high blood pressure, and rheumatic diseases (none, 1 to 3, 3 or more).
NUTRITIONAL STATUS
Conventional anthropometry
The following measures were considered: current weight (kg), height (m), body mass index (BMI, kg/m2), arm circumference (AC, cm), calf circumference (CC) (cm), and tricipital skinfold (TS, mm). Arm muscle circumference (AMC, cm) and corrected mid-upper arm muscle area (cAMA) were calculated. For measurement and classification we adopted the World Health Organization (WHO) criteria for BMI (9-11).
In order to minimize variability and increase reliability, all evaluators were trained, and the research equipment was calibrated as needed.
Adductor pollicis muscle thickness (APMT)
APMT was measured in each individual in a sitting position, with the arm flexed at approximately 90° and with the forearm and the hand resting on the knee, keeping the hand relaxed, as requested. We used a skinfold caliper, which exerted a continuous pressure of 10 g/mm² to pinch the adductor pollicis muscle at the apex of an imaginary triangle formed by the extension of the thumb and the index finger (5). The procedure was performed in both hands, in triplicate, using the mean value obtained as the final value. Cut-off points of 24.2 mm and 19.4 mm were adopted for men and women, respectively (12).
Handgrip strength (HGS)
A manual hydraulic dynamometer, which expressed values in kilograms, was used to assess HGS. Each individual was asked to sit with their feet flat on the ground, with their arm close to their chest and the elbow flexed at 90°, without being supported. Each measure was taken in triplicate, in both hands, considering the highest value as the result (13). The cut-off points used were those proposed by the European Working Group on Sarcopenia in Older People EWGSOP2 by sex (men: < 27 kg/f; women: < 16 kg/f) (14).
Patient-Generated Subjective Global Assessment (PG-SGA)
This study used the PG-SGA version validated for Brazilian Portuguese (3,4).
PG-SGA classifies individuals into: A (well nourished), B (suspicion of or moderate malnutrition), and C (severely malnourished). In addition, this method generates a score that helps the multidisciplinary team to define nutritional interventions, making specific decisions regarding patient and family guidance, symptom management, and adequate nutritional intervention: 0 to 1: no need for intervention; 2 to 3: requires nutritional education with the patient and family; 4 to 8: requires nutritional intervention; and total score ≥ 9: requires critical nutritional intervention and control of symptoms (3,4).
DATA ANALYSIS
Data were analyzed using the IBM SPSS Statistics® software (v.22, SPSS An IBM Company, Chicago, IL). A descriptive statistical analysis was performed using mean and standard deviation for continuous variables, and percentage for categorical variables. Pearson's correlation coefficient was used for the correlations of interest, setting the significance level at 5 %.
RESULTS
The sample consisted of 73 patients with a mean age of 66.9 ± 9.6 years. Most patients were men (53.4 %), elderly (≥ 60 years) (79.1 %), married (64.4 %), belonged to economic class C (71.2 %), and were not working (69.9 %) (Table I). Most patients were admitted to undergo surgical procedures (53.4 %), and 79.5 % had one to three chronic diseases when assessed.
Table I. Study sample characterization
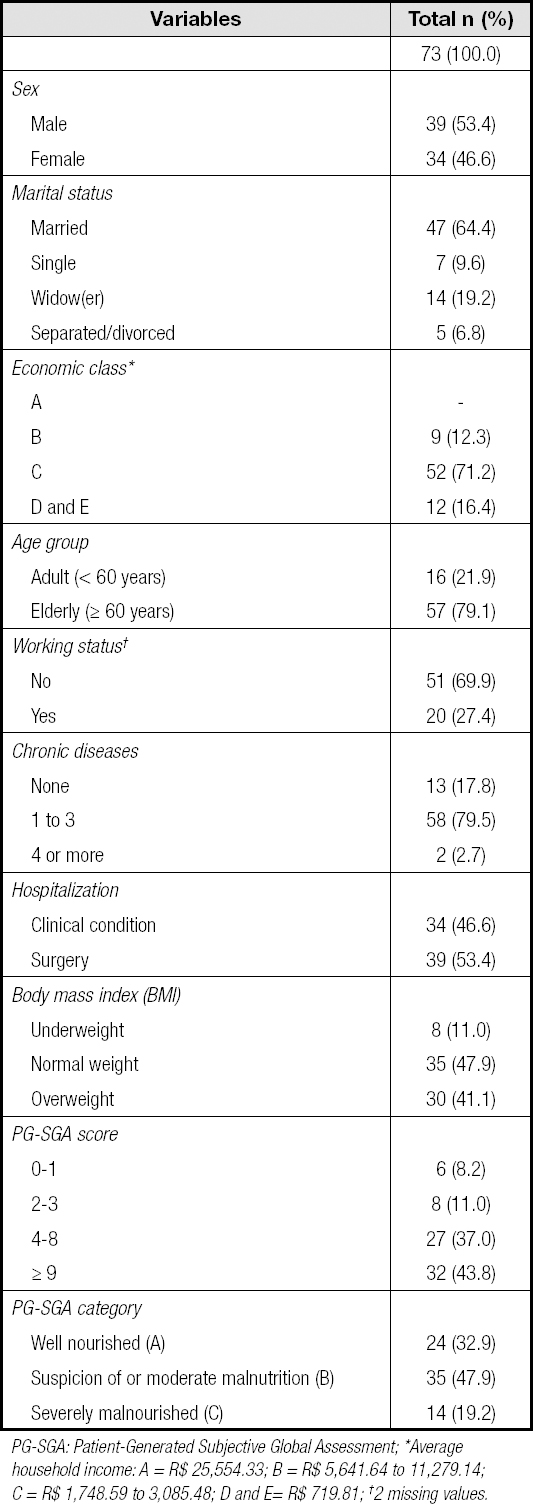
PG-SGA: Patient-Generated Subjective Global Assessment; *Average household income: A = R$ 25,554.33; B = R$ 5,641.64 to 11,279.14; C = R$ 1,748.59 to 3,085.48; D and E= R$ 719.81; †2 missing values.
Patients with an adequate BMI prevailed (47.9 %), whereas according to PG-SGA most patients (67.1 %) had some degree of malnutrition (B and C). Regarding the PG-SGA score, patients were predominantly classified with a score lower than 9 (56.2 %).
Patients mostly had a reduced APMT in both hands, while most patients had adequate HGS (Table II).
Table II. Distribution of individuals according to adductor pollicis muscle thickness and handgrip strength classification

APMT: adductor pollicis muscle thickness; HGS: handgrip strength (right hand: 9 missing values; left hand: 8 missing values).
Table III outlines the mean and standard deviation of the continuous variables that were used to investigate the nutritional status of patients, such as conventional anthropometry, APMT, and HGS.
Table III. Mean and standard deviation of the continuous variables investigated for nutritional status by sex

APMT: adductor pollicis muscle thickness; R: right; L: left; HGS: handgrip strength; BMI: body mass index; cAMA: corrected arm muscle area; AC: arm circumference; TSF: tricipital skinfold; CC: calf circumference.
APMT (R) was significantly correlated with the measures cAMA, CC, APMT (L), FFP (R), and HGS (L). APMT (L) was significantly correlated with the measures cAMA, AC, AMC, CC, PG-SGA score, and right and left HGS. Both HGS (R) and HGS (L) were significantly correlated with the measures CC, PG-SGA score, and APMT in both hands (Table IV).
Table IV. Adductor pollicis muscle thickness and handgrip strength correlation with anthropometric variables, dynamometry, and the Patient-Generated Subjective Global Assessment Score

r: Pearson's correlation coefficient; p: p-value; *significant; APMT: adductor pollicis muscle thickness; R: right; L: left; HGS: handgrip strength; BMI: body mass index; cAMA: corrected arm muscle area; AC: arm circumference; TSF: tricipital skinfold; CC: calf circumference.
DISCUSSION
Correlations of adductor pollicis muscle thickness and handgrip strength with CC and with the PG-SGA score were observed.
CC is the most commonly used measure to ascertain muscle depletion in the elderly, and has already been shown to predict performance and survival in this population when using the 31.0 cm cut-off point (15). Furthermore, CC can be used for muscle mass diagnosis in institutions lacking other muscle mass assessment methods (14).
An observational cross-sectional study conducted in 2015 with patients in anintensive care unit (ICU) found that APMT (R) was significantly correlated with BMI and CC. They reported that the lower values of APMT may have resulted from the sample composition, which included mostly elderly people (16). Conversely, a more recent epidemiological study conducted exclusively in elderly patients with chronic kidney disease (CKD) reported a significant correlation between APMT and conventional anthropometric measures such as CC, AC, TSF, and BMI (17). Including unconventional anthropometric measures in nutritional assessments is important considering their efficacy in detecting complications and risks of muscle depletion (14).
The PG-SGA tool is known to be a specific and sensitive instrument and is considered the gold standard for nutritional assessment in hospitalized patients. Thus, the significant correlation observed between PG-SGA and HGS and APMT highlight the latter two as complementary assessments of nutritional status in the hospital setting and for studies (3,18-20). Besides that, muscle strength can also be used to determine sarcopenia in adults and in the elderly (21). Our findings are supported by other studies. In a recent study with cancer patients APMT was significantly correlated with the PG-SGA score and with HGS in both hands (22). In the same way, another study conducted with 150 patients also showed significant associations between APMT, PG-SGA, and other conventional anthropometric measures (6). It should be noted that the cut-off points used by the authors in both studies were those proposed by Bragagnolo (23). Despite the fact that more stringent cut-off points were used in our study, our results were very similar. Schwanke et al., in a study to evaluate the association between APMT and nutritional parameters in hospitalized elderly patients in Brazil, reported that APMT was associated with all the investigated nutritional parameters, including MNA, BMI, AC, CC, and HGS (24).
Most participants in this study showed reduced APMT values and adequate HGS values. The sample of our study mainly consisted of elderly people, most of whom were not working, which may account for their loss of muscle mass. Physiologically, increased skeletal muscle mass losses are also inherent to age itself (25). It is important to highlight that although previous studies have reported that APMT could be used as a proxy of low lean mass in a clinical scenario, for epidemiological studies this measure cannot be used as single predictor of lean mass in health subjects (12).
Although HGS is also affected by the decrease in muscle mass, peripheral muscle strength is more related to the worsening of overall and cognitive function of the patient. Furthermore, in the elderly, this measure decreases with impairment of their daily living activities, functional dependence, risk of falls, and changes in gait (26,27). The prevalence of patients undergoing elective surgery in our sample, who possibly continued to perform their activities prior to hospitalization, may also explain the adequate HGS.
This study also underscores the use of objective and subjective parameters in clinical practice. Despite the fact that most patients were classified as ‘adequate' or ‘overweight' by their BMI, most were considered malnourished when assessed by APMT and PG-SGA. This finding shows that BMI should not be prioritized as an indicator of nutritional status in hospitalized individuals, especially when used alone. Factors which affect the functional decline of an individual, especially age-related changes such as those observed in the elderly population, and changes in muscle systems and strength, should be carefully monitored to establish preventive, recovery-related, and other interventions that may delay or prevent the functional decline of patients to improve their prognosis (28). A recent systematic review raised the question about the reliability of APMT measurement and that future studies should established cut-off values that are hand-, age-, sex-, and ethnic-specific before APMT can be used as a component of nutritional screening (29).
Our study is limited by its sample size and sample profile (mainly elective surgery). In addition, the cross-sectional design limits the evaluation of collected variables, especially of causal relationships. Despite including the number of chronic diseases, we did not use a validated comorbidity scale with prognostic value. We recommend that future research should use a expanded sample of hospitalized patients in order to provide more robust results. Furthermore, future research should investigate specific cut-off points for hospitalized patients with multiple morbidities.
CONCLUSION
APMT and HGS correlated with CC and PG-SGA in hospitalized patients. These measures should be implemented in clinical practice for the nutritional assessment of hospitalized patients to establish a reliable nutritional diagnosis and adequate nutritional therapy. They may boost the performance of the entire multidisciplinary team to outline strategies and interventions, including prevention and patient rehabilitation.














