Introduction
Dual pathology is a research issue that has been widely addressed by the scientific literature on addiction. In PubMed it is observed that the number of articles increases by approximately 200 new publications each year. These include epidemiological studies of prevalence (Hasin & Grant, 2015; Kessler & Chiu, 2005), nosology of dual pathology (Carmiol et al., 2014), effectiveness of intervention modalities (Hobden et al., 2018; Najt, Fusar-Poli & Brambilla, 2011), or factors that affect the therapeutic outcome (Horsfall, Cleary, Hunt & Walter, 2009; Wise, Streiner & Gallop, 2017). Although prevalence rates differ between studies, the majority of reports in the literature indicate that psychiatric comorbidity is not an exception among drug use patients, but instead occurs most frequently among this population (Torrens, Mestre-Pintó & Domingo-Salvany, 2015).
From a care perspective, patients with dual pathology present a greater diagnostic complexity, poorer therapeutic outcomes, and a higher number of health and social problems than those patients without such comorbidity (Di Lorenzo, Galliani, Ferri, Landi & Guicciardi, 2014). The adopted therapeutic approach usually involves the mental health network and specialized addiction services, used sequentially or in parallel (Balhara et al., 2016). In Spain, for example, in most of the autonomous communities it is common to find protocols for joint action between both services to provide dual pathology patients with a coordinated care regime (e.g., Elvira, Berrocoso, & Santos, 2007; Dirección General Asistencia Sanitaria, 2012). Specifically, these protocols are based on the classification developed by Ries (1992), noting that coordinated care between both networks is indicated when patients have a mental disorder that is highly complex, and whose addiction is difficult to manage. However, there are also autonomous communities with integrated care units for patients with dual pathology. These patients receive their treatments for both disorders by the same therapeutic team.
Therefore, in organizational terms, these units are more adapted to the needs of these patients, increasing the likelihood that they receive consistent diagnoses of their disorders, thereby avoiding contradictory therapeutic indications and achieving more efficient therapeutic prescriptions (Drake & Mueser, 2000). This modality of care is less widespread, not only in Spain but also in the rest of Europe and North America, in spite of the fact that various studies have indicated that this approach could be more effective (Drake, Mueser & Brunette, 2007; Georgeson, 2009; Staiger, Howard, Thomas, Young & Mccabe, 2014; Staiger, Long & Baker, 2010). This is because the creation of these units is complex for logistical and economic reasons.
Following the therapeutic results framework developed by Simpson et al. (1997), the effectiveness of the treatments depends fundamentally on structural / organizational factors of the care services, the type of intervention, and factors related to the characteristics of the patients. In the case of patients with dual pathology, a number of studies have analyzed these factors with the aim of promoting greater integration between mental health care networks and addiction services. For example, in structural / organizational terms it has been emphasized that changes in the therapist / patient ratio, the number of appointments, the availability of specific services, or guidance in the training of professionals (McGovern, Lambert-Harris, Gotham, Claus & Xie, 2014; Padwa, Guerrero, Braslow & Fenwick, 2015; Priester et al., 2016; Timko, Dixon & Moos, 2005) could all serve to improve the care of these patients. In terms of the intervention used, various authors have shown through review studies how there are specific interventions that can be more effective for patients based on the clinical profiles they present (Kelly, Daly & Douaihy, 2012; Torrens et al., 2015). Moreover, in terms of the characteristics of the patients, there are numerous studies comparing profiles of patients with and without dual pathology, and the relationship with therapeutic outcomes. However, most of these studies have been carried out either with patients treated in mental health services (Martín-Santos et al., 2006), or with those treated in addiction services (Araos et al., 2014; Carou, Romero & Luengo, 2017; Gual, 2007; Martínez-Gras et al., 2016; Pereiro, Pino, Flórez, Arrojo, & Becoña, 2013; Vergara-Moragues et al., 2012). These results, although useful, offer limited scope for informing care policies adapted to the profiles of the patients of each healthcare network. In general, these are independent studies, carried out at different times and places, so that no firm conclusions can be drawn about the most appropriate (i.e. profile-dependent) care policies that should be implemented for dual pathology patients.
One of the few studies that addressed this issue was that conducted by Havassy, Alvidrez, and Owen (2004). These authors carried out a study in the United States and used as their starting point the hypothesis that for dual pathology patients, there would be clinical differences between those who attended mental health services and those who used specialized addiction services. However, these authors found little difference between dual pathology patients treated in the two care networks. In Spain, the 'Madrid Study' (Arias et al., 2013a, 2013b, 2013c) was carried out with patients treated in the addiction center network and those treated in the mental health network. This study revealed differences between the care networks in terms of the prevalence of dual pathology patients (36.1% in mental health and 70.3% in the addiction center network), although no results were presented regarding a comparison of the profiles of these patients. In addition, there are as yet no clearly defined profiles of those patients where there are clinical indications for the use of receiving coordinated care. Therefore, the aim of the present work was to provide one of the first national in-depth studies of the profiles of patients in which there are indications for coordinated care. In particular, our goal was to compare the patients that follow this therapeutic indication with two other groups that attend only one of the two centers of the healthcare network. To this end, our two objectives were as follows: i) to analyze if there are differences in socio-demographic characteristics, substance dependence, and psychopathology according to the type of care modality that the patients receive; ii) to determine if any of these characteristics could affect attendance to each of these therapeutic modalities. In terms of a hypothesis, Havassy et al. (2004) found little difference between the two networks and, whilst in the present work we will study patients in which there are indications for coordinated care, according to the protocols there should be no differences between patients. Thus, it can be hypothesized that: 1) there should be no socio-demographic differences between patients according to the type of care services they attend; 2) the substance dependency profile should not differ between patients according to care modality; and, 3) there should be no differences in terms of other mental disorders depending on the type of care.
Method
Participants
The sample frame of the study consisted of patients diagnosed with dual pathology and treated in the Community Mental Health Units (CMHU) of Huelva and the Provincial Service of Drug Addiction of Huelva (ADH). The CMHU consists of multidisciplinary teams providing walk-in and domiciliary services belonging to the network of specialized care centers for people with mental health problems. The ADH is an outpatient treatment center coordinated by a multidisciplinary team whose service portfolio is focused on preventive care and treatment for people with addiction problems. The ADH also fulfills the function of coordinating all outpatient addiction treatment centers in the province of Huelva. To participate in the study, patients had to meet the following inclusion criteria: 1) to have a general level of functional activity, as evaluated by the Global Activity Assessment Scale (EGA) < 50; 2) to have been diagnosed with at least one substance dependence disorder in the last year according to DSM-IV-TR criteria; 3) to have been diagnosed in the last year with at least one other mental disorder with severe mental symptoms other than substance dependence according to DSM-IV-TR criteria; 4) to have clinical indications for receiving treatment in the coordinated service between the CMHU and ADH centers. The exclusion criteria were: 1) to have been diagnosed exclusively with nicotine dependence disorder, according to DSM-IV-TR criteria; 2) to meet criteria indicating abuse of one or more substances according to DSM-IV-TR, without having a diagnosis of dependence; 3) to have been diagnosed with mental retardation or another type of disorder that makes the interview impossible; and, 4) not giving signed informed consent.
Based on these inclusion and exclusion criteria, the care coordinators of the CMHU and the ADH prepared a list of 263 candidate participants. Accidental sampling was used, so that all patients who attended their therapeutic appointments were invited to participate in the study. The final sample consisted of 170 patients (64.6% of the census). Of these, 51 patients were treated exclusively in the CMHU, 64 patients in the ADH and 55 patients were treated in a coordinated manner between the CMHU and the ADH. Of the patients on the list who did not participate in the study, 25.9% did not attend their therapeutic appointment and could not be reached, and 9.5% refused to participate in the study.
Instruments
Mini International Neuropsychiatric Interview -MINI- (Sheehan et al., 1998). The MINI is a brief diagnostic structured interview, widely used in the field of psychiatry. In this study, the Spanish version was used (Ferrando, Bobes, Gilbert, Soto & Soto, 2000), through which 16 modules corresponding to the main Axis I psychiatric disorders are evaluated. These 16 modules are evaluated by 82 items, organized as follows: 1) Major depressive episode (6 items); 2) Dysthymic disorder (4 items); Suicide risk (6 items); Manic / hypomanic episode (4 items); 5) Anxiety disorder (7 items); 6) Agoraphobia (2 items); 7) Social phobia (4 items); 8) Obsessive-compulsive disorder (6 items); 9) Post-traumatic stress disorder (5 items); 10) Dependence / abuse of alcohol (3 items); 11) Dependence / abuse of other substances; 12) Psychotic disorders (13 items); 13) Anorexia nervosa (6 items); 14) Bulimia nervosa (8 items); 15) Generalized anxiety disorder (3 items); 16) Antisocial personality disorder (2 items). Each item presents a dichotomous response format that corresponds with the diagnostic criteria established in the DSM-IV.
Several studies have linked the MINI with the Composite International Diagnostic Interview (CIDI) and the Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II) showing Kappa agreement values between 0.76 and 0.93 (Lecrubier et al, 1997; Sheehan et al, 1997). In terms of internal consistency, values ranging from α = .654 (obsessive-compulsive disorder) to α = .951 (major depressive disorder) were found in the present sample.
Personality Inventory for DSM-5-PID-5- (Maples et al., 2015). We administered the 100-item Spanish version (Díaz-Batanero, Ramírez, Domínguez-Salas, Fernández-Calderón & Lozano, 2017), which evaluates, through a Likert response format ranging between 0 ('Totally false or often false') and 3 ('Very true or often true') the 25 traits included in Section III of the DSM-5 (American Psychiatric Association, 2013). The score for each trait is obtained by calculating the average of the scores of the items. Following Samuel et al. (2013), the scores corresponding to scores T <65 of the normative scores were considered indicative of clinically significant pathological traits. In this study, we used the normative scores developed by Gutiérrez et al. (2017). The internal consistency for each of the disorders showed values between α = .69 (obsessive-compulsive personality disorder) and α = .79 (antisocial personality disorder).
Procedure
A psychologist with experience in the evaluation of patients administered the tests in individual sessions. Before starting the data collection period, the psychologist received specific training for the administration of these tests. After the therapist had made contact with the patients, the interviews were carried out in the centers where the patients received their treatment. The therapist also informed the patients that the study was unrelated to their therapeutic process. Initially, the psychologist that administered the tests explained the objectives of the research and reported the voluntary nature of their participation. They were also told that the information collected would not be part of their clinical history without their express authorization. They were then read their informed consent, and if they wished to participate, they were asked to sign the form. Once the patient had given their consent, the interview began.
The ethics committee of the University of Huelva, and the hospital center (to which the Community Mental Health Units belong) both approved the study.
Analysis
The socio-demographic variables of the present study were analyzed as nominal variables, with the exception of age, which is a continuous variable. In the case of diagnoses, these are expressed in a dichotomous way, with a value of '0' indicating their absence and the value of '1' indicating their presence. Initially, a two-stage conglomerate analysis was applied to identify the profiles according to the main drugs of consumption. The Bayesian (Schwarz) criterion was used to determine the number of conglomerates, whilst the chi-square statistic was used to analyze the association between categorical variables. An ANOVA was conducted to determine the relationship between categorical and continuous variables.
Odds ratios were calculated through a logistic regression analysis, indicating the probability that an event occurs versus the probability that it will not occur. In the specific case of this study, an odds ratio for a given disorder higher than 1 would indicate that it is more likely to be observed in the reference group with respect to the comparative group. An odds ratio below 1 is taken to indicate that the disorder is less likely in the reference group with respect to the comparative group, whilst an odds ratio equal to 1 indicates that there is the same probability of observing the disorder in both groups.
Finally, a logistic regression analysis was applied, using the stepwise procedure to determine which variables have a greater explanatory capacity with respect to the therapeutic modality. The variables introduced in the model were those that showed a value of p < .05. All the statistical analyzes were conducted with the STATA version 14.0.
Results
Profile of consumption and prevalence of mental disorders in the sample
Patients with problems of alcohol abuse / dependence represented 41.8% of the sample, cannabis 45.9%, cocaine 45.3%, and heroin 24.1%. The cluster analysis revealed a solution of four clusters (Figure 1): 1) the first was composed of 51 patients, of whom 100% had problems of alcohol dependence and 31.4% problems with cannabis. This is, therefore, a cluster of patients with alcohol dependence, although there are also patients who have problems with cannabis use; 2) the second cluster is composed of 50 patients, 100% of which are cocaine dependent, 40% dependent on alcohol, 52% on cannabis, and 22% heroin. This cluster represents a group of patients with cocaine dependence, which also frequently consumes other drugs. This cluster could thus be regarded as one of cocaine-poly-drug patients; 3) the third cluster consists of 36 patients exclusively dependent on cannabis; and, 4) this final cluster consists of 33 patients of which 90.9% are dependent on heroin, and 81.8% dependent on cocaine. In Andalusia it is not uncommon to find this profile of users, who consume a mixture based on cocaine and heroin, often referred to as 'rebujao'.
With regard to Axis I disorders, 77.6% of the sample presented diagnostic criteria compatible with such a disorder. Of these, excluding substance use disorders, the most prevalent were anxiety disorders (64.1%). and mood disorders (50.6%). The prevalence of patients with lifetime psychotic disorder was 52.9% and current psychotic disorder 26.5%, whilst 20.6% had antisocial disorder, and 2.4% had an eating disorder. Personality disorders were detected in 50% of the sample. The most prevalent of these disorders were avoidant (30.6%), borderline (28.2%), and schizotypal (24.1%).
Socio-demographic characteristics according to modality of intervention
Table 1 displays the socio-demographic characteristics of patients according to the type of care they receive. As can be seen, the analysis of gender, age, marital status and level of study does not reveal that these characteristics are more likely in certain intervention modalities than others. However, it is observed that in the group of patients treated in the ADH there is a lower probability of finding patients receiving a pension with respect to the other therapeutic modalities. Specifically, the probability of finding people who receive a pension is 2.14 (1 / 0.468 = 2.14) lower than that observed in the other intervention modalities. With respect to economic status, the results show that there is a probability of 2.04 of finding patients who report an economic deficit in the ADH compared with the other modalities. In contrast, the group of patients treated at the CMHU are 2.72 (1 / .367 = 2.72) times less likely to report an economic deficit, and 2.99 times more likely to report having a stable income.
Substance use disorders, other Axis 1 mental disorders, and personality disorders according to the type of intervention
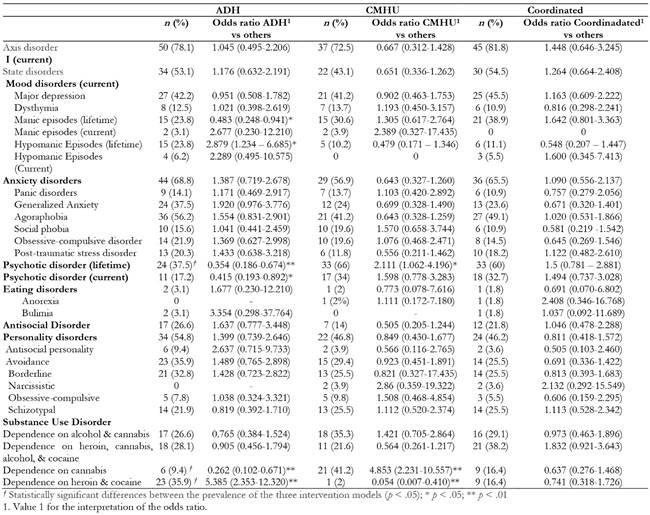
The distribution of the various mental disorders and the odds ratio corresponding to each group are shown in Table 2. In relation to Axis 1 disorders, it is observed that the probability of finding patients with manic episodes is 2.07 (1 / 0.483 = 2.07) times lower in the ADH compared with the other intervention modalities. In contrast, the probability of finding patients with hypomanic episodes is 2.879 times higher compared with the other care modalities. ADH patients are 2.82 times less likely to report lifetime psychotic disorders than those in the other care modalities, whilst the probability of having a current diagnosis of psychotic disorder is 2.41 lower than the other modalities. In contrast, patients in the CMHU are 2.11 times more likely to have had psychotic disorders at some time in their lives. The analysis of personality disorders did not reveal any differences in terms of prevalence or odds ratios among the three intervention modalities analyzed.
In relation to the consumption profiles, Table 2 shows that ADH patients are 3.82 (1 / 0.262 = 3.82) less likely to report problems derived from the exclusive use of cannabis. In contrast, there is a 5.39 times greater probability of finding patients with a profile of combined heroin and cocaine use. The opposite pattern of results was found in CMHU patients, where they are 4.85 times more likely to report having problems derived from cannabis use alone, and 18.51 times less likely to report problems of combined heroin and cocaine use.
Table 2: Comparison of Axis 1 disorders, personality disorders, and substance use disorders according to the service in which they receive care.
The multivariate analysis reveals that, among the dual pathology patients, attendance to the ADH is primarily explained by having a profile of heroin and cocaine dependence (odds ratio = 3.307), as well as having presented hypomanic episodes (odds ratio = 3.248). However, presenting a psychotic disorder is a factor that appears to be linked with non-attendance to this type of service (3.59 times less likely). Similarly, it is observed that in this resource there is a higher probability of patients reporting an economic deficit (odds ratio = 2.32), whilst attendance to the CMHU is explained mainly by presenting a cannabis dependence profile (odds ratio = 3.454), and is clearly not dependent on heroin and cocaine use (odds ratio = 7.75). It was also found that patients with an economic deficit are less likely to use this resource (odds ratio = 2.35) in comparison with the other therapeutic modalities (Table 3).
Discussion
The objective of this study was to compare the profile of dual pathology patients who receive coordinated care in two centers (CMHU and ADH) with patients who attend only one of the centers, as well as to identify which variables determine whether patients use a particular care resource. The initial hypotheses were based on the fact that, since all dual pathology patients should receive coordinated care from the ADH and CMHU network, there should be no differences in the patient profile according to the modality of care received by the patients. The results of this study partially support this hypothesis; no differences were observed between the three therapeutic modalities in terms of the majority of the analyzed disorders, although differences were observed in lifetime manic and hypomanic episodes, psychotic disorder, and dependence on cannabis and heroin and cocaine. Although quantitatively there are relatively few disorders in which differences were observed, in qualitative terms these disorders determine the profile of patients who come to each center and their healthcare needs.
As noted, among the ADH patients there is a higher prevalence of hypomanic episodes, but fewer manic episodes. This may be due to the fact that hypomanic episodes are more strongly linked with substance use, and are therefore primarily treated in the ADH. On the other hand, when patients are in a manic phase, their psychiatric stabilization is necessary, and it is therefore unsurprising to observe a lower prevalence of manic episodes in the ADH, with a higher odds ratio for these episodes in the coordinated service between the CMHU and the ADH.
A higher prevalence of patients with heroin and cocaine dependence has also been observed in the ADH, with a residual of this patient profile in the CMHU. In this regard, it should be noted that in the ADH, patients admitted to treatment for heroin and cocaine dependence represented approximately 20% of the patients who started treatment, which clearly determines the profile of patients that are shown to use these resources. However, there was an observed high prevalence of these patients in the ADH as opposed to the CMHU, despite these being patients with other (highly complex) mental disorders. This could be taken to suggest that the problems of these patients have been erroneously attributed to substance addiction, without adequately assessing the impact of other comorbid mental disorders on their daily lives.
Further, the higher probability of observing patients with psychotic disorders in the CMHU was also found in the study by Havassy et al. (2004). This result can be explained by the higher complexity of psychiatric care required for treating such disorders, and hence the higher rates of attendance to this service. In addition, the association between psychotic disorders and cannabis use has been widely documented (Radhakrishnan, Wilkinson & D'Souza, 2014). Therefore, it is logical to suppose that in the CMHU there has been a higher prevalence of patients diagnosed with cannabis abuse / dependence. It should be noted that in this study, these patients correspond mostly with a young patient profile (the average age of these patients in this study is 33 years (SD = 9.7) compared with the average age of 42.8 (SD = 10.9) in the remaining patients), who, possibly due to the severity of psychotic symptomatology, are more likely to attend the CMHU - rather than the ADH- as a matter of priority.
Another noteworthy aspect of our results is that economic status emerged as an explanatory variable for the patients' use of a particular service. In particular, more patients with no income were observed in the ADH centers than in the CMHU. There could be a number of reasons for this observation. For instance, chronic mental health users with severe mental disorders often retire early, which affords them a certain level of economic stability, whilst in the ADH centers - strongly linked with low or marginal economic status- the patients are heavily stigmatized. Thus, a user with a normalized socioeconomic status prefers to receive treatment at the CMHU (or go to private addiction centers) rather than attend ADH centers. Thus, a variable related to the socioeconomic status could be having an impact on their decision to select the most appropriate intervention for their mental health status.
From a therapeutic perspective, the results show that almost eight out of ten patients have an Axis 1 disorder whilst half have personality disorders, with this set of disorders being presented in a comorbid manner with substance dependence, regardless of the service that is used to treat them. In addition to this, it has been observed that there are differences in patient profiles between the two networks in spite of the fact that all if the patients have been diagnosed with dual pathology. Therefore, taken together, we consider that this set of findings constitutes sufficient evidence to suggest that whilst there is good coordination between the services, these patients require integrated care by teams of professionals that are specialized in dual pathology, a view that appears to be shared by the majority of professionals working in addictions and mental health (Szerman et al., 2014; Vega et al., 2015). As long as this is not the case, it is necessary to develop clinical protocols that not only include those aspects of the patient profile that indicate coordinated care, but that also consider the main evidence on therapeutic modalities and their effectiveness for specific patient profiles.
Although we believe that the results of this study should be considered in the care planning of mental health units and addiction centers, we consider it necessary to point out some limitations. In particular, it was not possible to contact 35.4% of the patients with indications for attending mental health services and addiction centers in a coordinated manner. The inclusion of such patients could have modified the profile of the patients observed in each of the therapeutic modalities analyzed. However, we consider it noteworthy that they stopped attending treatment; that is, it is precisely this 35.4% of patients that failed to attend their therapeutic appointments. This lack of therapeutic adherence could be the result of inadequate adjustment to the needs of these patients, which negatively affects their prognosis (Roncero et al., 2013). In this regard, although it has been widely shown that the presence of dual pathology negatively affects therapeutic adherence, future studies should analyze whether the failure to adapt resources to the needs of dual pathology patients could be a key factor in the lack of adherence to treatment (Araos et al., 2014). It should also be noted that all patients in this study were diagnosed with dual pathology by healthcare professionals (ADH and CMHU) following the diagnostic criteria of the DSM-IV-TR, as stipulated in the joint action protocol (DGAS, 2012). The disorders analyzed in this study were assessed through the MINI and the PID, the scores of which are in accord with the diagnostic criteria DSM-IV and DSM-5 respectively. Both interviews were fundamentally of a screening nature, and used diagnostic criteria that were different from those used in the inclusion and exclusion criteria; thus homogenization of the different versions would be desirable. But to the extent that these interviews were applied to all patients regardless of the modality of care and administered by the same qualified professional, we believe that the sources of error for the comparative analysis are fewer than those that would otherwise have been observed if the analysis had been conducted on the basis of diagnoses (made by different professionals) found in the clinical histories of each patient.
In spite of these limitations, we believe that this study provides novel findings that could help to inform the development of care resources that are adapted to the therapeutic needs of dual pathology patients. Future studies should analyze how different patient profiles evolve in these therapeutic modalities in terms of adherence, quality of life, and patient functionality.

















