Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Gaceta Sanitaria
versión impresa ISSN 0213-9111
Gac Sanit vol.26 no.1 Barcelona ene./feb. 2012
Evaluation of the national health surveillance program of workers previously exposed to asbestos in Spain (2008)
Evaluación del programa integral de vigilancia de la salud de los trabajadores que han estado expuestos a amianto en España (2008)
Montserrat García Gómeza, Rosario Castañedaa, Vega García Lópezb, Manuel Martínez Vidalc, Vicent Villanuevad, Mercedes Elvira Espinosae, Working Group on Occupational Health of the CISNS+ Commission on Public Health1
aÁrea de Salud Laboral, SGSAySL, Dirección General de Salud Pública y Sanidad Exterior, Ministerio de Sanidad, Política Social e Igualdad, Madrid, España
bSección de Epidemiología Laboral, Investigación y Evaluación Sanitaria, Instituto Navarro de Salud Laboral, Consejería de Salud, Gobierno de Navarra, Pamplona, España
cServicio de Salud Laboral, Dirección General de Ordenación e Inspección, Consejería de Sanidad, Comunidad de Madrid, España
dServicio de Salud Laboral, Dirección General de Salud Pública, Consejería de Sanidad, Generalidad Valenciana, Valencia, España
eDirección General de Salud Pública e Investigación, Desarrollo e Innovación, Consejería de Sanidad, Junta de Castilla y León, Valladolid, España
ABSTRACT
Objectives: Although asbestos was banned in Spain in 2001, monitoring the health of previously-exposed workers is required. In 2002 the Ministry of Health and the autonomous regions of Spain planned a health surveillance program for workers exposed to asbestos (Programa de Vigilancia de la Salud de los Trabajadores Expuestos al Amianto [PIVISTEA]) with employers' organizations, trade unions and scientific societies. The aim of this study was to evaluate the PIVISTEA to improve its effectiveness.
Methods: A questionnaire with indicators for the year 2008 was sent to Spain's 17 autonomous regions, as well as to the autonomous cities of Ceuta and Melilla. The results were analyzed by evaluating the compliance of each program with the activities established by the PIVISTEA.
Results: In December 2008, a total of 22,158 workers from 14 autonomous regions and 306 companies were included in the program. The program had been started in 88% of the regions but surveillance activities remained scarce in 24%. Fifty-seven percent of the autonomous regions (69% of the total number of workers) provided the information requested. Seven autonomous regions provided data on the relationship between the diseases found and asbestos exposure. Only 5% of these diseases entitled affected individuals to receive compensation for occupational diseases.
Conclusions: The health surveillance of workers previously exposed to asbestos in Spain, as well as medical-legal recognition of diseases caused by exposure at work, remain in adequate. Although the trend is positive, the effectiveness of many regional programs is limited, and inter-regional inequalities among affected workers have been detected.
Key words: Evaluation. Asbestos. Health surveillance. Programs.
RESUMEN
Objetivos: Después de la prohibición del amianto en España en 2001, resulta necesario vigilar la salud de los trabajadores expuestos en el pasado. En 2002, el Ministerio de Sanidad y las Comunidades Autónomas consensuaron un Programa de Vigilancia de la Salud de los Trabajadores Expuestos al Amianto (PIVISTEA) con las organizaciones empresariales y sindicales, y con las sociedades profesionales del sector. El objetivo de este estudio es evaluar el programa con el fin de tratar de mejorar su eficacia.
Métodos: Se enviaron cuestionarios con indicadores referentes al año 2008 a las 17 comunidades autónomas y a las ciudades autónomas de Ceuta y Melilla. Los resultados se analizaron evaluando el cumplimiento de cada programa en relación con las actividades establecidas en PIVISTEA.
Resultados: En diciembre de 2008, un total de 22.158 trabajadores, de 14 comunidades autónomas y 306 empresas, estaban incluidos en el programa. El 88% de las comunidades autónomas han iniciado el programa, aunque en el 24% las actividades siguen siendo escasas. El 57% (69% del total de los trabajadores) de las comunidades autónomas han proporcionado la información solicitada. Siete han comunicado datos sobre la relación entre la patología que encuentran y la exposición al amianto. Sólo el 5% de esas enfermedades son compensadas como profesionales.
Conclusiones: La situación en España respecto a la vigilancia de la salud de los trabajadores previamente expuestos al amianto, y el reconocimiento médico-legal de las enfermedades derivadas de esa exposición, aún no es adecuada. Aunque la tendencia es positiva, muchos de los programas autonómicos tienen todavía una eficacia limitada y se detectan desigualdades interterritoriales.
Palabras clave: Evaluación. Amianto. Vigilancia de la salud. Programas.
Introduction
Asbestos, from the Greek word asbestos, fireproof, and amiantos, incorruptible, comprises a group of metamorphic mineral fibers (silicates) well known for their indestructibility and high melting point.
There are two main categories of asbestos: serpentines, represented by chrysotile, and amphiboles1. Serpentine fibers, the best example of which is is chrysotile, or white asbestos, are wavy, flexible and easily breakable and soluble in tissues. Amphiboles, such as crocidolite (or blue asbestos) and amosite, are rigid, sharp and highly resistant to chemical or biological solution, and have a longer biological persistence2. In Spain these materials were banned by law in the Royal Decree 1406/1989 and the Act of December 7th, 20013,4.
Asbestos is extracted from open cast mines, a task that is always less dangerous than its purification and industrial uses. The epidemiological importance of this substance lies in the wide range of sources of exposure resulting from its numerous applications. Because of its resistance to mechanical force, electricity, chemical substances and fire, as well as its high insulating power, asbestos is used in around 1,500 industrial applications, such as construction, shipbuilding, the railway and automobile industries, plastics, chemicals and food, metallurgy, and every type of fire-insulating fabric5,6.
There are two kinds of exposure: occupational and environmental. The former can be strictly occupational, when the mineral is manipulated directly by the worker, or para-occupational, through proximity with other people in the same workplace. The latter can be domestic, through inhalation of asbestos fiber in the household after being transported by workers in their work clothes, or through aging of construction materials; environmental exposure can also be geographic, urban or industrial, and can occur through intake of liquid or solid products that may contain the mineral. Because of these epidemiological characteristics, asbestos is considered a potential and unlimited pathogenic substance7.
The asbestos fiber penetrates easily and deeply into the respiratory system, due to its physical, chemical and aerodynamics properties, and has been proven to cause asbestosis, pleural fibrosis, pleural and peritoneal mesothelioma, lung and larynx cancer and other gastrointestinal cancers8.
The environmental danger of asbestos is currently the subject of public debate. In July 2010, a Court in Madrid sentenced Uralita to pay more than 3.9 million euros to 45 inhabitants of Cerdanyola and Ripollet (Barcelona) for the damage resulting from asbestos dust exposure caused by a factory located between these two cities9. This was pioneer event in Spain, as it was the first time that claimants were not employees but people living in the proximity of the factory and who, according to the Court's resolution, suffered from diseases caused by daily contact with the asbestos used by the factory to manufacture its products.
There is a need for epidemiologic surveillance systems to monitor the incidence of asbestos-related diseases and their course over time, to study the fraction attributable to occupational asbestos exposure and to improve pathologic diagnosis. Several European countries, such as France10, Italy11, Germany12, and Scandinavian and Baltic countries13-16 have mesothelioma surveillance programs. However, the methods used are not homogeneous.
In Spain, after asbestos was banned, the problem focused on monitoring the health of workers with prior exposure to this substance and those currently involved in the demolition of asbestos-containing buildings and facilities and in asbestos removal tasks.
In 2002 the Ministry of Health and the autonomous regions of Spain planned a health surveillance program for workers previously exposed to asbestos (Programa de Vigilancia de la Salud de los Trabajadores Expuestos al Amianto [PIVISTEA])17 with the most important employers' organizations and trade unions, to guarantee an adequate and homogeneous national intervention. The first results showed that in 2005 the situation was not ideal, as the program's implementation rate among the autonomous regions was uneven18.
The aim of this study was to evaluate the performance of the PIVISTEA in December 2008 in order to try to improve its effectiveness.
Methods
A questionnaire was designed with all the basic indicators in a post-occupational health surveillance program. The checklists were sent to all PIVISTEA focal points in each of the 17 autonomous communities, as well as the autonomous cities of Ceuta and Melilla, at the beginning of 2009, with backup telephone calls to ensure that all the questionnaires were completed. Data were requested for the year 2008, so that the programs could monitor the whole year. The data analysis was carried out in the second half of 2009.
The questionnaire contained the following indicators:
• Structure assessment:
- The starting date for identifying the first cohort suitable for surveillance; the concluding date for identifying the first surveillance cohort; date of creation of the Register of Workers Exposed to Asbestos.
- Information on the companies that used asbestos: economic activity, according to the National Classification of Economic Activities.
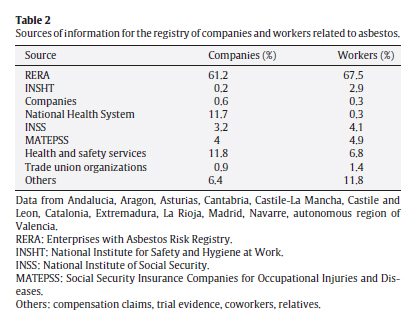
- Information sources of the companies that used asbestos: Enterprises with Asbestos Risk Registry, Public Health Services, National Institute of Social Security, Social Security Insurance Companies for Occupational Injuries and Diseases, Occupational Health and Safety Services, Trade Unions, and others.
- The number of workers registered by categories: exposed (removal), post-exposed (active, inactive -retired or unemployed-); losses to follow-up (non-traceable, uncollaborative, exitus).
- Health resources assigned to the program: from health departments (central and peripheral services); from public health services (primary and specialized care); from the occupational health and safety system.
• Evaluation of the process:
- Coverage: the number of workers (by categories) tested for the first time per year, multiplied by 100, divided by the total number of workers.
- Delay: the time interval between incorporation in the registry and the medical examination.
- The number of workers not attending the medical examination.
- The number of workers under surveillance per year (periodic medical examinations).
• Evaluation of the results:
- The number of workers (by categories) with asbestos-related diseases.
- The type and number of asbestos-related diseases.
- The number of asbestos-related diseases classified as occupational (entitling affected individuals to receive compensation).
A chart was made with the activities set out in the PIVISTEA, and each program's compliance with these activities was evaluated. The information collected in the records was transcribed into a database, and a descriptive analysis was performed using the statistical package SPSS-PC19. The results of the program's implementation and the number of asbestos-exposed workers are shown by autonomous regions. The information sources for the register are shown in percentages, and asbestos-related diseases overall by disease and exposure situation.
Results
Of the 17 autonomous regions receiving the questionnaire, in addition to Ceuta and Melilla (19 in total), 95% responded, with a delay of between 11 days and 8 months. Melilla, and the Canary and Balearic Islands had not yet started the program; no data from 2008 were available from Extremadura or Galicia, and therefore data from 2007 were used. There was no information from Murcia.
Table 1 summarizes the actions developed in each autonomous region, showing wide variability. Ceuta and 15 (88%) of the autonomous regions had started the program. Melilla and the remaining two (12%) autonomous regions did not have a program, and four (24%) autonomous regions had implemented only a few activities. Figure 1 shows the current state of development of the programs and the number of workers in the autonomous regions with a history of occupational asbestos exposure. In December 2008, a total of 22,158 workers from 14 autonomous regions and 306 companies were included in the program. Half of these workers were inactive (retired and unemployed) and 45.7% were active. The remaining workers recruited to the program were lost to follow-up.

Figure 1. Status of the health surveillance program and number of asbestos-exposed
workers included per autonomous region in Spain 2008.
To evaluate the appropriateness and adequacy of the program, information on the size and characteristics of the cohort of asbestos-exposed workers, the total amount of resources, and the qualifications and suitability of the professionals performing the activities, must be available. Nine (64.3%) out of the 14 autonomous regions that started the program were aware of the economic activity of the companies and workers that used asbestos in the past and 12 (85.7%) provided their sources of information (Table 2). Five (35.7%) autonomous regions did not show information about the available workforce; in the remaining 64.3%, 64 health professionals from the health departments (central and peripheral services), 53 from the public health services (34 pneumologists and 19 radiologists); and 34 from the system of prevention of occupational risks, were involved.
Eight (57%) autonomous regions provided the information requested for evaluation of the process. Coverage varied from 5.65% in Catalonia to 96% in Valencia, the average being 58.6%. Delay was not reported regularly, only La Rioja and Valencia provided this information (150 and 120 days, respectively).
Seven (50%) of the autonomous regions that started the program provided data on the possible relationship between the diseases found and asbestos exposure. Eight (57%) autonomous regions provided information on the asbestos-related diseases in these workers (Table 3 and Table 4).
Finally, other data requested, constituting a basic objective of PIVISTEA, consisted of the number of diseases classified as occupational and entitling affected individuals to compensation. Strikingly, only Asturias and Navarre provided this information: 3.7% and 6%, respectively.
Discussion
One limitation of this study lies in the validity of the data, which was provided by the autonomous regions themselves; obtaining some of the information was difficult, due to the lack of staff specifically dedicated to the program. Although the questionnaires were not always fully completed, and gathering them took 8 months, the collaboration of the autonomous regions was generally satisfactory, allowing important data to be obtained for this study.
As seen in the results of our analysis, although health surveillance of asbestos-exposed workers who had ceased to work in the risk activity -whether because of retirement, change of company or any other reason- has been regulated in Spain since 1993, not only in occupational areas but also in health areas18, and the PIVISTEA was approved by the National Commission of Public Health (plenary assembly of December 12, 2002), the National Commission of Occupational Safety and Health (plenary assembly of January 29, 2003) and the Interterritorial Council of the National Health System (plenary assembly of its Executive Committee of February 26, 2003), some autonomous regions had not yet introduced this program. In addition, those that had done so were performing only a few of the basic activities recommended. Many of the questionnaire sections were left blank, showing the precariousness of post-occupational surveillance of the health of these workers in Spain.
Unfortunately, no similar articles have been found in the literature to compare these results with those in other countries. As previously stated, there are mesothelioma surveillance programs in several European countries, but there are no health surveillance programs for workers previously exposed to asbestos similar to the Spanish program.
A high percentage of the questionnaires (35.7%) provided no data about the staff available. The remaining autonomous regions that did provide this information clearly showed that the number of available staff was insufficient to perform the activities that should be included in any post-occupational health surveillance program. The development of a post-occupational health surveillance program requires strenuous efforts to coordinate the distinct administrative areas. These programs also involve both primary care and specialized health professionals from the public health system, as well as staff from the occupational risk prevention services from both companies and the public structures of the autonomous communities, all of which poses difficulties for putting such programs into practice. Assigning more personnel to the program would allow professionals working in the national health system to increase identification of occupational exposures that could be the cause of some of the diseases seen in their practice.
There were wide variations in the coverage achieved among the autonomous regions initiating the program, and only two regions were close to 100% coverage. An important question is whether most of the asbestos-exposed workers have been identified, or whether current cohorts will be enlarged in the future, which would imply changes in the global population under surveillance and in the coverage indicator. The total population that would benefit from the program would also increase. For example, in Madrid a search of different sources for the identification, location and inclusion of workers in the cohort allowed the initial list of 918 exposed individuals to be increased to the current 4,84320, and in Navarre, an active search identified 1,694 out of the 3,713 persons comprising the cohort21.
One of the main aims of the national program is to encourage the medical-legal recognition of asbestos-related diseases. However, as described above, only two autonomous regions were aware of this information. This finding draws attention, first of all, to the need to urgently improve collaboration and coordination between the national health and social security systems to facilitate information exchange, recognition and compensation for these diseases to workers. Secondly, the low number of diseases classified as occupational (6% in Navarre and 3.7% in Asturias) might be caused by various factors. Firstly, the diseases might currently affect retired workers, without coverage for professional compensation, as these individuals are no longer working and would therefore not be included in the Registry of Occupational Diseases. If these persons are receiving any social security benefits (retirement, disability, widowhood, orphanhood) resulting from occupational disease, the statistics on the type of disease that led to these benefits are unknown22. Secondly, these diseases may be considered as common, leading to their under-recognition as occupational. This consideration is crucial as, according to some authors, 83% of occupational diseases are not included in the official registry23. Two facts illustrate underreporting in the case of asbestos: in 2001, 29 cases of asbestosis were reported in Spain as occupational diseases, while during the same year 210 people diagnosed with asbestosis were treated at Spanish hospitals11. A study performed in the Basque Country, which studied mortality and the incidence of occupational sentinel events in 1987 in the population aged over 24 years and examined several sources found that only two out of the eight pleural mesothelioma that appeared in the cancer registry had been studied in the disability assessment medical units, and none declared as occupational disease24. Importantly, pleural mesothelioma, as well as asbestosis, are both occupational sentinel events inherent to the workplace and are highly unlikely to appear without occupational exposure.
To sum up, the situation in Spain regarding the health surveillance of workers previously exposed to asbestos and medical-legal recognition of diseases caused by exposure at work are not yet adequate. Despite being a right and a duty established by law, some autonomous regions do not monitor programs and most of those that have been started are poorly developed. To improve this situation, the national coordination structure should be reinforced, and each autonomous region should mobilize resources to initiate and/or develop regional programs.
One of the objectives of the PIVISTEA program, which was based on broad consensus, is to guarantee uniform specific medical health surveillance for workers. This goal is not being achieved, leading to inter-regional inequalities among the workers involved. Major differences were found among the autonomous regions and consequently a qualitative study is urgently required to identify the obstacles to the implementation and development of the programs, as well as possible improvement strategies.
Because of the lack of information and dispersion of people exposed to asbestos at work in the past, evaluation requires configuration of an active surveillance system for mesothelioma and asbestosis. Such a system would allow cases to be located and the cohort of exposed workers to be reconstructed. Active identification of asbestos-related diseases requires other procedures (memory and/or records of other colleagues), examination of health records (hospital discharge records, cancer registries, work disability system, mortality statistics) and especially the involvement and coordination of health professionals and the resources described in this article.
Programs such as the PIVISTEA provide an opportunity for collaboration between the occupational risk prevention system and the national health system and can also be used as an example and guideline for similar programs in the future focusing on other occupational carcinogens, with long latency periods, that require surveillance to preserve the health rights of exposed workers.

Author's contributions
M. García Gómez conceived the study and supervised all aspects of its performance. All the authors collected data, contributed ideas and reviewed the drafts of the manuscript. All the authors approved the final version of the manuscript. M. García is responsible for the article.
Funding
None.
Conflicts of interests
The authors warrant they have no financial or other relationships that could have influenced the performance of the study or the preparation of the manuscript for publication.
*Appendix A. Remaining members of the Working Group on Occupational Health of the CISNS+ Commission on Public Health
Valentín Esteban Buedo (Servicio de Salud Laboral, Dirección General de Salud Pública, Consejería de Sanidad, Generalidad Valenciana, Valencia, España), Carlos Rodríguez (Instituto Asturiano de Prevención de Riesgos Laborales, Gobierno del Principado de Asturias, Oviedo, España), Alberto Montilla (Sección de Salud Laboral, Dirección General de Salud Pública, Consejería de Salud y Bienestar Social, Junta de Comunidades de Castilla-La Mancha, Toledo, España), Juan Carlos Coto (Unidad de Salud Laboral, Instituto Vasco de Seguridad y Salud Laborales-Osalan, Consejería de Empleo y Asuntos Sociales, Gobierno Vasco, Vitoria, Álava, España), José Luis Millares (Servicio de Epidemiología y Salud Laboral, Secretaría General de Salud Pública y Participación, Consejería de Salud, Junta de Andalucía, Sevilla, España), Nieves Martínez Arguisuelas (Sección de Salud Laboral, Dirección General de Salud Pública, Consejería de Salud y Consumo, Gobierno de Aragón, Zaragoza, España), María Luisa Mena (Sección de Salud Laboral, Dirección General de Salud Pública, Consejería de Salud y Consumo, Gobierno de Aragón, Zaragoza, España), Lourdes Miralles (Dirección General de Salud Pública y Consumo, Consejería de Salud, Gobierno de La Rioja, Logroño, España), Rosa Fernández Bardón (Dirección General de Salud Pública, Consejería de Salud, Generalitat de Catalunya, Barcelona, España), Íñigo Fernández Fernández (Sección de Salud Laboral, Servicio de Salud Pública, Dirección General de Salud Pública, Consejería de Sanidad, Gobierno de Cantabria, Santander, España), Yolanda Anes del Amo (Dirección General de Gestión del Conocimiento y Calidad, Consejería de Sanidad y Dependencia, Junta de Extremadura, Cáceres, España), Ana Rivas (Servicio de Epidemiología, Consejería de Sanidad y Consumo, Ciudad Autónoma de Ceuta, Ceuta, España), Patricia López Menduina (Área de Salud Laboral, SGSAySL, Dirección General de Salud Pública y Sanidad Exterior, Ministerio de Sanidad, Política Social e Igualdad, Madrid, España).
Bibliografía
1. Greiller L, Astoul P. Mesothelioma and asbestos-related pleural diseases. Respiration. 2008; 76:1-15. [ Links ]
2. McDonald JC, McDonald AD. The epidemiology of mesothelioma in historical context. Eur Respir J. 1996; 9:1932-42. [ Links ]
3. Real Decreto 1406/1989, sobre limitaciones a la comercialización y al uso de ciertas sustancias y preparados peligrosos. Boletín Oficial del Estado no 278, 20/11/1989. [ Links ]
4. Orden de 7 de diciembre de 2001, que modifica el anexo I del Real Decreto 1406/1989, sobre limitaciones a la comercialización y al uso de ciertas sustancias y preparados peligrosos. Boletín Oficial del Estado no 299, 14/12/2001. [ Links ]
5. Sartorelli E. Trattato di medicina del lavoro. Padova: Piccin Editore. 1981. p. 703-8 and 1039-41. [ Links ]
6. Gilson JC, Asbestosis. In: Parmeggiani L., editor. Enciclopedia de salud y seguridad en el trabajo. Madrid: Ministry of Work and Social Security; 1989. 289-94. [ Links ]
7. Desoille H, Martí Mercadal JA, Scherrer J, et al. Medicina del trabajo. Barcelona: Masson; 1986. [ Links ]
8. Villanueva V, Ballester R, Celma C, et al. Protocolos de vigilancia sanitaria específica: amianto. Madrid: Ministry of Health and Consummers Affairs. 1999; 9-24. [ Links ]
9. EFEverde. [Accessed 30/08/2010.] Available at: http://www.efeverde.com/esl/contenidos/noticias/14-julio-2010-08-40-00-sentencia-pionera-en-espana-obliga-a-indemnizar-a-vecinos-victimas-del-amianto. [ Links ]
10. Gilg Soit Ilg A, Goldberg M, Rolland P, et al. The French national program for mesothelioma surveillance - principal results 1998-2006. Saint-Mauri French Institute for Public HSurveillance; 2009. 24 p. Available at: http://www.invs.sante.fr. [ Links ]
11. Marinaccio A, Nesti M. Regional operational centers, Analysis of survival of mesothelioma cases in the Italian registry (ReNaM). Eur J Cancer. 2003; 39:1290-5. [ Links ]
12. Neumann V, Günter S, Müller KM, et al. Malignant mesothelioma - German mesothelioma register 1987-1999. Int Arch Occup Environ Health. 2001; 74:383-95. [ Links ]
13. Kjaergaard J, Anderson M. Incidence rates of malignant mesothelioma in Denmark and predicted future number of cases among men. Scand J Work Environ Health. 2000; 26:112-7. [ Links ]
14. Ulvestad B, Kjaerheim K, Moller B, et al. Incidence trends of mesothelioma in Norway, 1965-1999. Int J Cancer. 2003; 107:94-8. [ Links ]
15. Järvholm B, Englund A, Albin M. Pleural mesothelioma in Sweden: an analysis of the incidence according to the use of asbestos. Occup Environ Med. 1999; 56:110-3. [ Links ]
16. Karjalainen A, Pukkala E, Mattson K, et al. Trends in mesothelioma incidence and occupational mesotheliomas in Finland in 1960-1995. Scand J Work Environ Health. 1997; 23:266-70. [ Links ]
17. García-Gómez M, Artieda L, Camino F, et al. Programa nacional de vigilancia de la salud de trabajadores expuestos a amianto. Madrid: Ministry of Health and Consummers Affairs. 2004; 8-16. [ Links ]
18. García-Gómez M, Artieda L, Esteban V, et al. Health surveillance of workers exposed to asbestos: an example of co-operation between the occupational prevention system and the national health system. Rev Esp Salud Pública. 2006; 80:27-39. [ Links ]
19. SPSS/PC+ for the IBM PC/XT/AT. Chicago: SPSS Inc.; 1986. [ Links ]
20. Zimmermann M, Martínez M, González MF. Reconstrucción de la cohorte de trabajadores expuestos a amianto en un ámbito autonómico: estudio de salud basal. Gac Sanit. 2004; 18(Supl 3):120. [ Links ]
21. Artieda L, Beloqui A, Lezaun M. Cohorte poblacional de trabajadores expuestos a amianto, Navarra 1999-2004. An Sist Sanit Navar. 2005; 28:335-44. [ Links ]
22. Ministerio de Trabajo e Inmigración. Seguridad Social. [Accessed 6/09/2010.] Available at: http://www.seg-social.es/Internet_1/Estadistica/Est/Pensiones_y_pensionistas/index.htm. [ Links ]
23. García AM, Gadea R. Estimation of morbidity and mortality through occupational diseases in Spain. Arch Prev Riesgos Labor. 2004; 7:3-8. [ Links ]
24. Fernández A, Esnaola S, García Gómez M, et al. Los sucesos centinela ocupacionales. Vitoria: Gobierno Vasco, Departamento de Sanidad y Consumo; 1990. [ Links ]
![]() Correspondence:
Correspondence:
mgarciag@mspsi.es
(M. García Gómez).
Received 5 January 2011
Accepted 27 June 2011