Introduction
In Spain, the prevalence of problematic alcohol consumption, assessed with the AUDIT questionnaire,1 is approximately 4.9%.2 Moreover, 15.5% of Spaniards between 15 and 64 years has participated in episodes of binge drinking in the past month, a percentage that increases in young adults (20-24 years), reaching almost 35% in the male population.2
However, only 5 to 10% of problem drinkers are identified or receive any type of treatment or brief counseling by professionals of the primary care services.3,4 The fact that the assessment of alcohol consumption is sometimes limited to those patients whose reason for consultation is directly related to their consumption or to their symptomatology reveals the need to identify and treat them.5 This situation is striking when taking into account that both identification and brief intervention in these services have proven to be an efficacious, effective, and efficient element to reduce risky alcohol consumption.6,7
In view of this, many studies have assessed the possible barriers in the health professionals for the identification and treatment of problem drinkers. In this sense, and despite the fact that general practitioners support early intervention in alcohol-related problems,8,9 the lack of time to address them, together with the lack of training and the lack of support from government policies or of funding or incentives, are emerging as the main barriers that hinder its implementation.9-14 The perception that alcohol consumption is more difficult to address with the patients or the fear of offending them or of harming the relationship with the patient by asking questions about alcohol are also barriers frequently referred to by health professionals.5,15-17 Another barrier is professionals’ low motivation and low expectations about the effectiveness of a brief intervention.5,8,18
With regard to patient factors, the professionals’ belief that patients will not be motivated to change, they will not be interested or they will make up excuses to avoid intervention are also barriers commonly referred to by health professionals.11,13,19,20 Professionals are also convinced that patients will not answer questions about alcohol consumption honestly.19,21
Despite that all these barriers have been widely evaluated, few studies have been carried out in Spanish population. Therefore, the goals of this study are to analyze the barriers perceived by health professionals in different Spanish health centers when identifying and treating problem drinkers, and to determine the importance granted to such identification and intervention, as a function of the health team to which the professionals belong. We also analyze the psychometric properties of the questionnaire used to assess these barriers.
Method
Participants
Participants were 107 health professionals belonging to nine primary care centers in the province of Alicante (Spain), of whom 62.7% (n = 67) belonged to the medical team and 32.4% (n = 40) to the nursing team.
Variables and instruments
By means of an ad hoc questionnaire, we first assessed perceived barriers to the identification and treatment of problem drinkers. A two-stage process was used to develop the questionnaire. First of all, we performed a review of previous studies5,8-11,13-21, in order to compile the barriers mentioned in them. Second, after a frequency analysis, we selected the most commonly referred barriers and developed a 9 items-questionnaire for their assessment in Spanish health professionals.
Respondents were asked to indicate their level of agreement on a scale of 1 to 5 (strongly disagree to strongly agree) of the following barriers: (a) lack of time, (b) fear of offending patients, (c) lack of adequate training or experience, (d) considering it pointless to speak with patients about their alcohol consumption, (e) not perceiving risky alcohol consumption as an important health problem, (f) believing that patients would lie about their alcohol consumption, (g) believing that patients will not identify the negative consequences of their consumption, (h) believing that patients will not accept an intervention for their alcohol consumption, and (i) considering that the intervention would not help patients to change their alcohol consumption.
We also assessed the degree of importance granted to the identification and treatment of problem drinkers with a single item on Likert-type scale ranging from 1 (not at all important) to 5 (very important).
Procedure
We contacted with the primary care directors of all Alicante and Elche public care centers. Nine of them agreed to participate. After arranging a meeting with the medical directors of those centers, we went to the centers during working hours and explained the goals of the study. Both medical and nursing staffs were invited to participate in the study. All those who wished to participate, after given the permission to use their data, completed the questionnaire anonymously and confidentially, following the instructions provided. The current study was reviewed and approved by the ethics committee of the Miguel Hernández University.
Analysis of results
The obtained data were coded and analyzed with the IBM SPSS 20.0 statistics for Windows computer program. We analyzed the reliability of the instrument through its internal consistency (Cronbach's alpha coefficient). Alpha values should be equal to or higher than .70 to be acceptable.22 We also performed descriptive analysis (means and standard deviations) of all the items, as well as we calculated the discrimination index for each item. Item discrimination was classified as poor (<0.20), acceptable (0.20-0.29), good (0.30-0.39) and excellent (≥0.40).23
To analyze the factor structure of the questionnaire, we performed a factor analysis with the principal components extraction method and Varimax rotation. We also tested the intercorrelation between the scores of each factor with Pearson's correlation coefficient. Once the initial factor structure was obtained, we also performed a second-order factor analysis, in order to test the possible unidimensionality of the questionnaire. The raw scores on the factors obtained in the first factorial analysis were used for this second analysis. Finally, we also analyzed the differences in the assessed variables (all continuous variables) with Student's t-test for independent samples with a 95% confidence level.
Results
Reliability analysis
Cronbach's alpha coefficient of the test was initially .62, indicating an acceptable level of internal consistency (Table 1). Given that the items concerning the belief that alcohol consumption is not an important health problem, the lack of time, and the lack of training or experience all presented poor discrimination indexes (less than 0.20), they were removed as recommended by Ebel and Frisbie's.23 The internal consistency coefficient of the total scale, rose from an alpha of 0.62 to 0.70 after the removal of these items.
Table 1 Reliability coefficients and mean scores in the perceived barriers questionnaire.
| Items of the perceived barriers questionnaire (n=107) | Mean (SD) | Discrimination index | α without the item |
|---|---|---|---|
| 1. Lack of time during the consultation | 3.13 (1.03) | 0.14 | 0.63 |
| 2. The patient may be offended | 2.48 (1.16) | 0.36 | 0.58 |
| 3. Lack of adequate training/experience | 2.93 (0.99) | 0.18 | 0.62 |
| 4. No point in talking about alcohol consumption | 1.46 (0.88) | 0.25 | 0.61 |
| 5. Risky alcohol consumption is not a major problem | 1.56 (1.17) | 0.15 | 0.64 |
| 6. The patient will lie about his/her consumption | 3.29 (1.18) | 0.47 | 0.55 |
| 7. The patient will not identify the negative consequences of consumption | 3.24 (1.09) | 0.42 | 0.56 |
| 8. The patient will refuse treatment | 3.09 (0.88) | 0.49 | 0.56 |
| 9. The intervention will not help to change consumption | 2.15 (1.10) | 0.32 | 0.59 |
SD: standard deviation.
Internal consistency total scale: α=0.62.
Internal consistency eliminating items 1, 3 and 5: α = 0.70.
Out of all the items, those related to the belief that patients would not accept intervention, as well as the beliefs that they would lie about their consumption and would not identify the negative consequences of drinking showed high discriminative power, with discrimination indexes ranging between 0.42 and 0.49. They were followed by the items assessing the belief that patients may be offended if the professional addressed their alcohol consumption and that the intervention would not help them to change their consumption, with good discrimination indexes (between 0.32 and 0.36). Finally, the item assessing the belief that there is no point in talking about alcohol consumption showed acceptable discrimination index (.25).
Factor analysis
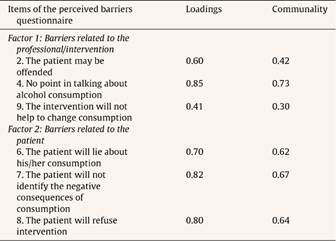
After reliability analysis, we conducted factor analysis on the 6 items that made up the final questionnaire. The KMO test was 0.73, and Bartlett's statistic was statistically significant (p < 0.01).
The principal component analysis with varimax rotation confirmed the existence of two factors (Table 2). The first factor was called “Barriers related to the professional and to intervention”, which groups the items that assess the belief of that patients may be offended if their alcohol consumption is addressed, the belief that it is pointless to talk about such consumption, and the professionals’ expectations about the help the treatment can provide to change alcohol consumption. The second factor was called “Barriers related to the patient”, made up of items that assess the belief that patients will lie about their true consumption, that they will not identify the negative consequences of their consumption, and that they will not accept participating in a treatment for their alcohol consumption. The percentage of variance explained by the two-factor structure was 56.40%.
Correlation between factors was high (r = 0.43, p <0.01) and the second-order factor analysis showed a one-factor structure which was statistically significant (χ2 = 20.32, p = 0.001) and explained 71.29% of variance. Thus, the questionnaire showed to be a unidimensional measurement instrument, supporting thereby the use of a single total score.
Differences between health professionals of the medical and nursing teams
As shown in Table 3, the results obtained yielded no significant differences (p >0.05) between the two teams of health workers in any of the barriers evaluated, resulting in a very similar mean level of agreement in each team.
Table 3 Differences between medical team (n = 67) and the nursing team (n = 40) on the of perceived barriers questionnaire.

SD: standard deviation.
aRange of factor score: 0 to 15.
These professionals pointed out that the three main barriers for identification and intervention are, firstly, the belief patients will lie about how much they really drink and will not identify the negative consequences of their consumption, followed by the belief that patients will not agree to participate in a treatment for their alcohol consumption (Table 3).
In contrast, the barriers related to believing that there is no point in addressing alcohol consumption or that the intervention will not help to change patients’ consumption obtained a low mean agreement, even approaching levels of strong disagreement in the former item. And, lastly, at a medium level of agreement, was the item about the belief that patients may be offended if the professionals address their alcohol consumption (Table 3).
With regard to the scores of the factors, no differences between the means of the scores of the two health teams were found in either of them (p >0.05), with a mean total score in the factor Barriers related to the professional and the intervention of 6.09 ± 2.09 and of 9.65 ± 2.50 in the factor Barriers related to the patient. No differences were also found between medical (M = 15.86, SD = 4.06) and nursing team (M = 15.45, SD = 3.68) in the total score of the questionnaire (t = 0.52, p >0.05).
Despite the perceived barriers, identification and treatment of problem drinkers is considered very important by the health professionals, who assigned a mean total score of 4.74 ± 0.54. No significant differences (t = -0.74, p >0.05) were found in the level of importance between the professionals of the medical team (M = 4.71 ± 0.61) and the nursing team (M = 4.79 ± 0.41).
Discussion
In view of the lack of studies in Spanish population, the goals in this work were to analyze the barriers perceived by health professionals to identify and treat problem drinkers and the level of importance granted to such identification and intervention, as a function of the professionals’ health team. We also analyzed the psychometric properties of the questionnaire used to assess these barriers.
The results obtained show a high awareness by health professionals, both from the medical and the nursing teams, of problematic alcohol consumption, granting a high level of importance to the identification and treatment of problem drinkers in the primary care setting. Likewise, these professionals recognize the usefulness of addressing alcohol consumption in the consultation. These results contrast with those reported in studies with samples of other countries, where, despite recognizing the importance of promoting moderate alcohol consumption, health professionals are more pessimistic about the effectiveness of an intervention and this emerges as one of the main barriers for the implementation of identification and intervention.5,8,9
The evidence obtained in this study indicates that the main factors that act as barriers are related to the beliefs that patients will not be honest when talking about their alcohol consumption, will not be capable of identifying the negative consequences of their consumption, and will not want to receive intervention. These findings are consistent with previous studies in which the main reasons for the reluctance to identify and treat problem drinkers are the assumptions about patients’ response and their motivation for change, as well as the belief that patients will not be interested in receiving intervention.11,13,19,20 In this sense, as reflected in the mean score of the factor Barriers related to the patient, which is higher than that of the factor Barriers related to the professional and the intervention, it seems that beliefs about the problem drinker's characteristics and attitudes have more weight in preventing the assessment and treatment of risky alcohol consumption than aspects like appropriate training and experience or the perception of the effectiveness or utility of the intervention.
The stereotyped image of the problem drinker has been shown in previous studies to be a noteworthy barrier in dealing with alcohol consumption in the consultation.15 Nevertheless, these results are to be expected when we consider that unawareness of the associated problems, resistance to change, and the rejection of being labeled as an “alcoholic” are some problem drinkers’ main characteristics and reasons for not seeking or delaying access to treatment.24-26 In the same vein, previous investigations point out that sometimes this type of patients do not seek treatment until they observe negative consequences associated with their alcohol consumption or they receive some kind of social pressure.27-29 It therefore seems important not only to train health professionals so they become more familiar with the characteristics of problem drinkers, but also to encourage them to apply brief interventions, precisely as a solution to these main above-mentioned barriers. As shown by the evidence in this regard, this type of intervention uses tools and strategies to mobilize motivation to change, and this is one of the essential goals of its application.30-32 Lastly, although differences were found in some prior studies,33,34 the fact that the scores in the items show no significant differences in the barriers perceived by the professionals of the medical and nursing teams also indicates that this instrument can be used interchangeably for the assessment both of doctors and nurses, guaranteeing the reliability of the results obtained for the two types of healthcare professionals.
This study has a series of limitations to be taken into account for future research. Firstly, the sample size should be increased to enable the generalization of the results obtained. Likewise, future studies with a second sample could be useful to perform a confirmatory factor analysis of the one-factor structure obtained in the present study. On another hand, the inclusion of other variables, such as sociodemographic variables, health care professionals’ training, and variables related to the detection and intervention -for instance, the number of screenings and brief interventions made during the latest months- would also be desirable. It could also have qualitative interest to let the respondents to add items to assess perceived barriers that were not included in the initial instrument. This way, we could determine more complete profile of the health professional who is reluctant to incorporate such interventions in the consultation. This would help to improve the design of programs to facilitate and encourage the assessment and treatment of problem drinkers in primary care.