Introduction
Smoke-free laws are an important instrument in tobacco control to protect people from the hazards of secondhand smoke (SHS)1,2 and to reduce smoking consumption rates, especially among young adults.3 Since the approval of the World Health Organization Framework Convection for Tobacco Control (WHO-FCTC) in 2003, many countries have introduced policies to restrict smoking in indoor public places and workplaces, including health care and educational locations.2 However, research has demonstrated that despite the existence of indoor regulation, non-smokers continue to be exposed to SHS in outdoor areas where smoking is still allowed,4,5 mainly because smokers have moved outdoors due to indoor smoking bans.6 SHS exposure in outdoor locations will decrease when a more restrictive regulation comes into force7 and smoking prevalence will drop, especially among the youth.8
High concentrations of outdoor SHS are determined by the density of smokers, the creation of semi-open places, a lack of wind and the presence of stable atmospheric conditions.9 The presence of nitrosamines and particulate matter ≤2.5μm in diameter (PM2.5) has been found in both open and semi-open places,9,10 with the associated risks for health. Besides health concerns, there are other reasons to support the prohibition of outdoor smoking such as reducing the litter, decreasing fire risks, and, most importantly, establishing a positive smoke-free model for youth in order to reduce imitative behavior.11
In Spain, 28.6% of young adults aged 18 to 24 years old are enrolled in university-level degree programs.12 Universities, especially those that offer degree programs in health-related disciplines, can contribute to the health of the wider community by setting an example of good practice and banning smoking from their premises.13 Similarly, university health professional students (HPS) should act as role models for their patients, and acquire knowledge and skills to assist their patients stop smoking.14
Previous studies have demonstrated that university smoke-free policies are associated with a drop in student smoking rates15 and with fewer students reporting exposure to SHS or seeing someone smoke on campus.16 These studies have been conducted in the United States (US), where tobacco-free campus policies are a growing trend as of October 2015, 1,620 US universities were 100% smoke-free campuses.17
In many European countries outdoor smoke-free regulation are less prevalent, and limited mainly to primary and secondary schools.2 Since the year 2011, Spain has had one of the most comprehensive smoke-free regulations indoors; in addition, the current legislation also restricts smoking in some outdoor public areas- including hospital premises, primary and secondary school grounds and playgrounds.18 Nevertheless, the existing ban does not prohibit smoking on university campuses. As a result, entrances areas and outdoor areas in near proximity to these entrances often concentrate numerous smokers, which could represent a health risk for non-smokers due to ongoing exposure to SHS over times.7 A study conducted in Barcelona found that 90% of university students reported being exposed to SHS in outdoor areas of their university campuses.6
In the last 20 years, smoking rates have decreased substantially among Spanish adults (aged 16 to 24 years old) -from 32.1% in 199319 to 24.7% in 201320-; however, these rates are still high when compared to other developed countries such as the US (18.7%)21 or Australia (18.5%).22 According to studies published in the same period (1997 to 2016), smoking prevalence among HPS in Spain ranged from 38.7%23 to 18.2%24 among nursing students, and from 27.0%25 to 15.7%26 among medical students.
Given that the process of adopting smoke-free legislation requires strong political will and population support, it is essential to determine student support before implementing outdoor smoke-free policies at university campuses. The current legislation means that HPS have become one of the university student groups most affected by smoke-free regulations in Spain. Mainly because medical and nursing faculties are often located near acute care hospitals and, of course, these students spend much of their practical training in such facilities. As a result, they are affected by both indoor and outdoor smoking bans. This is the case at the Universitat Internacional de Catalunya (UIC) Health Professions Campus, which is located adjacent to an acute care hospital, although both institutions have separate main entrances.
In this context, we sought to investigate whether HPS are influenced by outdoor smoking bans in hospitals and also whether they agree with extending smoking regulations to outdoor campus areas. Our main aims were to identify the factors that influence these students in having a more favorable attitude towards outdoor smoking bans and to ascertain support for such policies.
Methods
Design and participants
This is a cross-sectional study conducted at the Faculty of Medicine and Health Sciences at the Univesitat Internacional de Catalunya (UIC), located in Barcelona (Spain).
Participants were students from the Nursing and Medicine degree courses at the UIC who were enrolled in classes during the first quarter of the 2014-2015 academic year. For inclusion, subjects were required to meet the following criteria: 1) enrolled in the nursing or medicine degree program, 2) age ≥18 years during the 2014 academic year, and 3) registered in the class in which the study data were collected. Students in practical training during the study period were excluded due to difficulties in reaching them. Consequently, we included nursing students from the 1st to 3rd year of school, and medical students from the 1st to 4th year.
Instrumentation
An anonymous, self-administered questionnaire based on the Global Health Professions Student Survey (GHPSS) was designed to be administered during regular class hours. This questionnaire included questions covering tobacco use, SHS exposure, enforcement of smoking bans, attitudes and beliefs towards tobacco control activities, and agreement with the health professionals (HP)’ and HPS’ role.27
To collect information about “compliance with the smoke-free campus ban”, “agreement with the smoking ban” and “exposure to SHS”, we differentiated between indoor and outdoor areas. Each of the questions had five response options (ranging from “totally agree” to “totally disagree”). For purposes of this study, responses were recalculated into two dichotomous answers (agreement = totally agree and agree, and non-agreement = not agree, not disagree, disagree, totally disagree). We also collected data on participants’ demographic characteristics, including sex (male or female), age group (≤18 years old, age 19-21, ≥22 years old), degree (medicine or nursing) and degree program year (1, 2, 3, 4). For this paper, the main independent variables were smoking status28 [classified as smokers (including daily and occasional smokers) and non-smokers (including both former smokers not smoking for 6 months or longer, and never smokers)], degree, sex, and age group. We ruled out degree program as independent variable for performing the analysis because it was highly correlated with age group.
Procedure
Prior to questionnaire distribution, all students were informed about the main objectives of the study and all provided informed consent for their voluntary participation.
The final study sample was composed of 384 students, a response rate of 74.3% (384/517) of the students enrolled. All students that were in class on the day of the survey, voluntary participated in the study. Participation among medical students was slightly higher than among nursing students [81.1% (253/312) vs 64.0% (131/205)]. Medical students accounted for 65.9% (253/384) of participants, with nursing students accounting for 34.1% (131/384) of the final sample. Females were more represented than males in both degree programs, although the proportion of females in the nursing degree was significantly higher (79.5% vs. 66.0%; p <0.001). In the final sample, 70.6% (n=272) were females and 29.4% (n=112) were males, and females had a higher participation rate than males (83.6% vs 58.3%).
Data analysis
We computed prevalence rates (%) and corresponding 95% confidence intervals (95%CI). For the bivariate analysis we use Chi square test or the Fisher exact statistic when one or more of cells had an expected frequency of 5 or less, with p <0.05 as statistical significant threshold. Students were categorized into three age groups and the Chi square test was used to assess for the linear trend. Logistic regression analyses for attitudes concerning students’ support to smoke-outdoor campuses and their agreement with the exemplarity role were performed, after controlling for smoking status, sex, degree and age group. Odds ratios (OR) and 95%CI were calculated. We selected these attitudes because we focus the study in the evaluation of attitudes towards smoke-free outdoors and exemplarity role which were conceptually considered the most relevant for answering our research question. The statistical analysis was performed with the statistical package SPSS 21.0 for Windows.
Results
Smoking status
Overall, 23.4% of responders were smokers. By degree, 17.5% of medicine students smoked vs 35.1% of nursing students (p ≤0.001). By sex, 25.2% of men and 22.9% of women were smokers. By age, 34.7% of those ≥22 years old were smokers, whereas 20.0% of ≤18 years, and 21.2% of 19-21 years were (p for trend = 0.034).
Agreement with health professionals’ role in tobacco control by independent variables
Table 1 summarizes students’ agreement with several tobacco control statements including HP’ and HPS’ role. Nearly three-quarters (74.9%) of the students agreed that HP should set an example by not smoking. Only 58.6% of smokers agreed with this statement vs 79.7% of non-smokers (p <0.001). Similarly, a smaller percentage of students in the youngest age group (≤18 years old) agreed with this statement compared to those in older age groups (p for trend = 0.004). When students were asked about their own role in setting an example 64.1% agreed. Smokers and the youngest students expressed lower support (statistically significant in both cases: p <0.005) about the importance of setting an example. Finally, 54.4% of the students believed that tobacco cessation treatments should be included in the National Health System (NHS), with nursing students demonstrating significantly greater support for this policy than medical students (69.7% vs 46.9%, p <0.001).
Table 1 Student agreement with the role of health professionals and health professional students in tobacco control by independent variables.
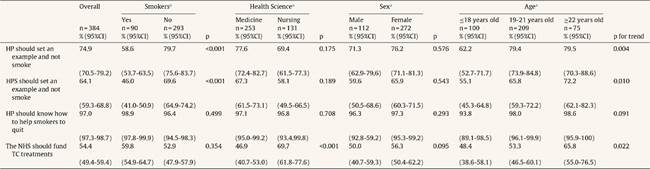
95%CI: confidence interval of 95%; HP: health professionals; HPS: health professional students; NHS: National Health System; TC: tobacco control.
aMissing data.
Compliance with smoke-free policies and exposure to secondhand smoke in indoor and outdoor areas
Nearly all students (97.9%) agreed that indoor campuses should be smoke-free. By contrast, only 39.3% supported banning smoking in outdoor areas of university campuses with non-smokers significantly more supportive of such a ban compared to smokers (48.8% vs 8.1%; p <0.001) (Table 2).
Table 2 Agreement with the compliance of the smoke-free campus ban and support for indoor and outdoor smoke-free policies.

95%CI: confidence interval of 95%; UC=University Campus.
aMissing data.
bFisher exact statistic.
A high percentage of students (87.0%) reported believing that the university complies with the indoor smoking ban, but only 12.2% agreed about the compliance with the outdoor ban. Compared to nursing students, a significantly higher percentage of medical students believed that the outdoor ban is respected (8.5% vs 18.9%; p = 0.006).
In addition, 8.1% of the students reported that they had not been exposed to SHS on campus during the prior week. The majority (89.3%) were exposed in outdoor areas, without differences among students’ degree and sex. Smokers reported higher exposure to SHS than non-smokers (98.9% vs 87.0%; p <0.001) (Table 3).
Factors associated with exemplary role and smoke-free outdoor campuses
Table 4 summarizes HPS’ factors associated with having positive attitudes towards tobacco control (including exemplarity role and agreement with smoke-free outdoor campuses) after running a logistic regression model (that controls by sex, age, degree, and smoking status). Compared to smokers, non-smokers were more likely to believe that HP (OR = 2.854; 95%CI: 1.651-4.936) and HPS should set an example by not smoking (OR = 2.755; 95%CI: 1.642-4.624). In addition, compared to younger students, a higher percentage of older students believed in the importance of HPS and HP setting an example.
Table 4 Factors associated with some tobacco control attitudes and beliefs among tobacco control.

HP: health professionals; HPS: health professional students; UC: university campus.
Method used for the logistic regression: ENTER.
Non-smoking students were 12 times more likely than non-smokers to believe that smoking should be prohibited in outdoor areas of the campus (OR = 12.315; 95%CI: 5.377-28.204). Older students were more likely to support outdoor smoking bans: students in the 19-20 years old age group were twice as likely support outdoor smoking bans than younger students (OR = 2.085; 95%CI: 1.199-3.624); students in the oldest age group (≥22 years) were three times more likely than younger students to support the ban (OR = 3.001; 95%CI: 1.439-6.257).
Discussion
This is the first study to explore HPS attitudes about compliance with indoor and outdoor smoke-free policies on university campuses in Spain among HPS. Our results show that four years after a comprehensive smoke-free law was passed in Spain, support among HPS for extending smoke-free policies to outdoor areas of university campuses is low. Non-smokers and older age groups were more likely to positive attitudes about tobacco control in terms of agreeing with the need to: 1) set a good example and by not smoking and 2) pass outdoor smoking bans.
In our study, only 40% of student participants agreed with the notion of extending smoke-free policies to outdoor areas of the campus. A previous study conducted in the Washington state -where a smoke-free campus policy was in place- showed that 72.0% of students supported the policy.29 Although there were several notable differences between our study and the Washington one in terms of the results, in both studies non-smokers showed greater support than smokers for outdoor smoke-free regulation. A previous study conducted at Tennessee State University suggests that, before implementing outdoor smoking bans, it would be beneficial to identify sub-groups that are more receptive towards such measures in order to leverage this support to promote positive attitudes towards change in current smoking policies.30
In our study, we included several independent variables including smoking status, age, sex, and degree to check for differences between sub-groups. We found that a higher percentage of nursing students smoked compared to medical students (35.1% vs 17.5%; p <0.001). For this reason, our adjusted model included area of study apart from other sociodemographic variables. Our results suggest that smoking and being in the young age (≤18 years) were associated with lower support for tobacco control measures. As previously reported, both Spanish nursing students31 and medical students25 are unaware about their own role when they are smokers. In this sense, it was interesting to observe that in our model HPS’ support of tobacco control was associated mainly with smoking status and age, rather than the health science degree studied. This imply that if measures were implemented to reduce smoking consumption among all students enrolled in Health Science degrees, then agreement in favor of tobacco control policies would probably increase.
Our findings regarding exposure to SHS are consistent with a previous study6 and also help to explain low compliance with outdoor smoke free policies. In the US compliance with SHS and acceptance of outdoor smoking bans has increased over time.16,28 In Spain, the lack of specific regulations for university Health Professions Campuses means that HPS are largely unaware of the benefits of outdoor smoking ban in place at hospitals. However, research has shown that the more frequently such policies are adopted, the higher the compliance and support.32
WHO-FCTC suggests that national bodies and organizations should protect the population from the hazards of SHS ‘wherever the evidence shows that hazard exists’, including quasi-outdoor and outdoor places.33 However, the adoption of smoke-free legislation in any setting requires strong population support to achieve a high degree of compliance. Meanwhile, several measures can be undertaken to facilitate implementation and improve compliance. For instance, the Tobacco-Free College Campus Initiative proposes actions that could improve motion, such as improving the communication channels, improving signage, reinforcing compliance surveillance, maintaining grounds litter-free, and so on.34
Our results seem to point out future directions that university administrators and undergraduate health science’ educators could take to advance the implementation of tobacco-free universities in Spain. Firstly, Spanish University Associations should adopt comprehensive smoke-free policies that included a similar to the one approved by the American College Health Association in 200917 that included a package of measures to facilitate implementation. Secondly, university educators should provide specific training techniques for preventing and controlling tobacco use. Lastly, specific actions should be undertaken by universities to promote protection from SHS and encourage smoking cessation. In our context, a previous study has proven that multicomponent intervention tailored to university students obtains high abstinence rates at 6 months.35 Although, such initiatives are still uncommon, Spanish universities should provide tobacco cessation services to reduce high smoking prevalence rates.24-26
This study has limitations, mostly due to the use of a self-administered questionnaire, which can lead to social desirability bias. We attempted to minimize these limitations by basing our questionnaire on a previous questionnaire used in similar populations.27 In addition, data on SHS exposure was self-reported and we did not use biomarkers to detect exposure; as a result, participants may have underestimated their exposure. However, since we only sought to explore whether the HPS were exposed or not to SHS during their time on campus precise levels of exposure were not required. Another limitation is the cross-sectional study design; moreover, our study is the difficulty in extrapolating results to other Spanish Universities given that UIC is a private university, and it is quite probably that students at UIC have a higher socioeconomic status. We did not assess socioeconomic status, which would have been useful to adjust the analysis for this variable. Finally, we cannot rule out selection bias given that 25% of registered students did not attend class on the day the survey was conducted. It is plausible that absent students had different attitudes and opinions about tobacco control. Nevertheless, we expect that our results may be similar to those obtained at other Health Science Universities due similarities in curriculum.
In conclusion, support to extend such bans to outdoor ages of university campuses is limited. Non-smokers and older students expressed moderate levels of support. Our findings indicate that, before smoke-free regulations are extended to outdoor areas, it is necessary to educate students on the importance of tobacco control and to persuade them to set an example for other students and patients. These aims can be achieved by promoting smoking cessation among smokers and convincing HPS to act as role models by not smoking. Future research should include the implementation of initiatives that include a range of actions- including outdoor bans- similar to those proposed by the Tobacco-Free College Campus Initiative. Pilot programs should be undertaken to evaluate the impact and success of such measures, with the ultimate aim of extending smoke-free policies to all university campus.















