Introduction
Cardiovascular diseases (CVD) are the leading cause of death in developing and developed nations,1 and the social, medical, and economic burden of CVD is likely to increase over the next decades worldwide.1 In Spain, there were 210,618 new cases of CVD in men and 220,957 in women in 2015.2
The prevention of CVD requires a combination of population and individual-level approaches,3 but very little research in CVD prevention in Spain has leveraged population approaches.4 An understanding of social factors that influence CVD is key to designing and implementing these approaches. Socioeconomic position, as measured by several indicators including race, education, income, and social class, has been associated with CVD in several studies.5-7 Importantly, inequities in CVD may be a reflection of similar inequities in CVD risk factors,8 which may be more tractable and amenable to interventions to prevent the development of CVD. In Spain, there is evidence of unequal exposure to CVD risk factors such as smoking,9 high blood pressure,10 high cholesterol,10 diabetes11 or obesity12 by socioeconomic status, along with higher mortality in people with established CVD and lower income.13 However, very few of these studies have been conducted in nationally representative samples.
The pathway between socioeconomic position and CVD risk factors might be different for each risk factor. For instance, inequities in diabetes, blood pressure and high cholesterol may be moderated by inequities in obesity14 or by inequities in treatment and control.15 Some of these social inequities in CVD are heterogeneous by gender, in a phenomenon called intersectionality. For instance, the educational social gradient in smoking prevalence in Spain varies greatly by gender, and this variation has evolved through time.9
Despite the mounting evidence regarding the role of socioeconomic position and cardiovascular health in different settings, there is scarce information on studies looking at the sub-national heterogeneity in these. This is specially important in countries like Spain, which has a territorial organization with markedly autonomous regional governments (autonomous communities) with legislative power over numerous social welfare aspects, including healthcare and education. This territorial organization warrants the possibility to explore heterogeneity in aspects related to social and health inequities. Understanding which regions have wider inequities can be a powerful advocacy tool for improved, more egalitarian health promotion and disease prevention policies in those regions.
The objective of this study was to describe social inequities in cardiovascular risk factors in women and men by autonomous regions in Spain.
Method
Study population
We used data from the 2017 Spanish National Health Survey (n = 23,089). We excluded participants from the autonomous cities of Ceuta and Melilla (N = 255 and 281, respectively) due to low sample sizes, those aged < 18 (N = 538), and those with missing values in social class (N = 579), high cholesterol (N = 36), diabetes (N = 12), hypertension (N = 28), obesity (N = 955) or smoking (N = 18), leaving a final analytic sample of 20,406 individuals (10,712 women and 9,694 men). Additional information about the sampling strategy and interview details of the Spanish National Health Survey can be found elsewhere.16
Exposures
We used occupational social class as our main measure of socioeconomic position. Survey participants were asked about their past or current occupation, which was then classified using the Spanish version of the International Standard Classification of Occupations.17 Each occupation was assigned to a social class category, as suggested by Domingo-Salvany et al.18: (I) higher grade professionals, administrators, and officials; managers in large industrial establishments; (II) lower grade professionals, administrators, and officials; higher grade technicians; managers in small industrial establishments; sportspeople and artists; (III) intermediate occupations and own-account workers; (IV) lower supervisory and technical occupations; (V) skilled workers in primary production and other semi-skilled workers; and (VI) non-skilled workers. In sensitivity analyses, we used education and household income as alternative proxies of socioeconomic position. Education was defined as the highest level of education achieved, and classified as university degree or equivalent, advanced professional school, mid-level professional school, complete high school, first stage of secondary education complete, complete primary education, incomplete primary education, and can't read or write. Income was measured as monthly net household income and classified as ≥6000, 4500-5999, 3600-4499, 2700-3599, 2200-2699, 1800-2199, 1550-1799, 1300-1549, 1050-1299, 800-1049, 570-799, and < 570 euros per month.
Outcomes
We used data on five modifiable cardiovascular risk factors: high cholesterol, diabetes, hypertension, obesity, and current smoking. High cholesterol, diabetes, and hypertension were defined as someone who answered “Yes” to at least one of the questions “Have you ever suffered from. . .?” and “Has your doctor ever tell you that you suffer from. . . diabetes/high blood pressure/high cholesterol?”, respectively. Obesity was defined as a body mass index ≥30 kg/m2; height and weight were self-reported. Individuals were classified as current smokers if they answered “Yes, daily” or “Yes, but not daily” to the question “Are you a current smoker?”.
Covariates
Data on age (in years), gender (women or men), and region (autonomous community) were self-reported.
Statistical analyses
First, we performed a descriptive analysis of sociodemographic characteristics and cardiovascular risk factors calculating survey weighted means and proportions of continuous and categorical variables, respectively, overall and for women/men. We performed t-test (for continuous variables) and chi squared tests (for categorical variables) for women/men taking into account survey weights and stratification. We also described the distribution of occupational social class and each of the outcomes by autonomous community.
We calculated the relative index of inequality (RII)19 by estimating prevalence ratios of each of the five cardiovascular risk factors for occupational class; we used Poisson regression models with robust standard errors, acknowledging the complex sur vey structure by including weights and stratification using R survey package. Social class was treated as an ordinal variable after exploratory analysis revealing a log-linear dose-response between risk factors and social class. RII above one indicate higher inequity, while RII below one indicate inverse social gradient. All models were adjusted for age and squared age and were stratified for women/men by introducing an interaction term between social class and women/men. To assess regional differences in these associations, we then ran the same model for each of the 17 autonomous communities. We displayed RII for each risk factor-region-women/men combination. In sensitivity analyses, we estimated absolute prevalence differences by social class with the slope index of inequality,19 and repeated the analyses by autonomous community using education and household income as exposure variables. We conducted all analyses and plots with R V3.5.1.
Results
Table 1 describes the sociodemographic characteristics and prevalence of cardiovascular risk factors in the sample. Mean age was 49.55 years, slightly higher in women (50.09) than in men (48.99). Approximately 11%, 8%, 19%, 15%, 34%, and 14% of participants belonged to social classes I through VI, respectively. These distributions were similar in men and women, with a higher proportion of women belonging to social class IV (lower supervisory and technical occupations) and a higher proportion of men belonging to social class VI (non-skilled workers). The prevalence of cardiovascular risk factors was: 24% for high cholesterol, 10% for diabetes, 27% for hypertension, 18% for obesity, and 24% for smoking. Men had a higher prevalence of smoking and obesity as compared to women (28% vs. 21%, and 19% vs. 17%). Supplementary tables I and II in online Appendix show the distribution of occupational social class and cardiovascular risk factors by autonomous community, respectively. Figure 1 shows the prevalence of cardiovascular risk factors by social class categories, where there was a linear dose-response relationship between occupational class and each of the risk factors. Supplementary fig. I shows the prevalence also stratified by age.

Figure 1. Prevalence of cardiovascular risk factors by social class categories, overall, in women and men. Social class classification: (I) higher grade professionals, administrators, and officials; managers in large industrial establishments; (II) lower grade professionals, administrators and officials, higher grade technicians, managers in small industrial establishments, sportspeople and artists; (III) intermediate occupations and own-account workers; (IV) lower supervisory and technical occupations; (V) skilled workers in primary production and other semi-skilled workers; and (VI) non-skilled workers.
Table 1. Characteristics of the participants (aged ≥18) from the Spanish National Health Survey (N = 20,406)
| Individual characteristicsa | Total (N = 20,406) | Women (N = 10,712) | Men (N = 9,694) | pb |
|---|---|---|---|---|
| Age (years), mean (SD) | 49.55 (17.6) | 50.09 (18.0) | 48.99 (17.2) | < 0.001 |
| Social class | ||||
| I. Higher grade professionals, administrators and officials; managers in large industrial establishments | 2164 (10.6%) | 1109 (10.4%) | 1055 (10.9%) | 0.708 |
| II. Lower grade professionals, administrators and officials; higher grade technicians; managers in small industrial establishments; sportpeople and artists | 1577 (7.7%) | 839 (7.8%) | 738 (7.6%) | 0.625 |
| III. Intermediate occupations and own account workers | 3879 (19.0%) | 2104 (19.6%) | 1775 (18.3%) | 0.256 |
| IV. Lower supervisory and technical occupations | 3012 (14.8%) | 1393 (13.0%) | 1619 (16.7%) | < 0.001 |
| V. Skilled workers in primary production and other semi-skilled workers | 6898 (33.8%) | 3574 (33.4%) | 3324 (34.3%) | 0.811 |
| VI. Non-skilled workers | 2876 (14.1%) | 1693 (15.8%) | 1183 (12.2%) | < 0.001 |
| High cholesterol | 4937 (24.2%) | 2548 (23.8%) | 2389 (24.6%) | 0.006 |
| Diabetes | 1986 (9.7%) | 921 (8.6%) | 1065 (11.0%) | < 0.001 |
| Hypertension | 5601 (27.4%) | 2873 (26.8%) | 2728 (28.1%) | 0.054 |
| Obesity | 3693 (18.1%) | 1861 (17.4%) | 1832 (18.9%) | 0.027 |
| Current smoker | 4972 (24.4%) | 2280 (21.3%) | 2692 (27.8%) | < 0.001 |
SD: standard deviation. a. Reported as n (%) unless specified. b. p correspond to t-test (for continuous variables) and chi squared tests (for categorical variables) by women/men. All statistical tests accounted for complex survey structure by including weights and stratification.
Table 2 shows the RII of cardiovascular risk factors for the entire Spanish territory. Overall, the RII was statistically significant for all risk factors; it was lowest for high cholesterol (RII = 1.02; 95% confidence interval [95%CI]: 1.00-1.04), and highest for obesity (RII = 1.16; 95%CI: 1.12-1.19) and diabetes (RII = 1.13; 95%CI: 1.10-1.17). RIIs of diabetes, hypertension, and obesity were higher for women (interaction p = 0.01, p < 0.001 and p < 0.001, respectively), while inequities in current smoking were stronger for men (interaction p < 0.001).
Table 2. Associations between social class (1-category decrease in social class) and cardiovascular risk factors prevalence. Model acknowledged the complex survey structure by including weights and stratification.
| Total | Women | Men | Interaction p | ||||
|---|---|---|---|---|---|---|---|
| RII | 95%CI | RII | 95%CI | RII | 95%CI | ||
| High cholesterol | 1.02 | 1.00-1.04 | 1.03 | 1.01-1.06 | 1.01 | 0.99-1.04 | 0.391 |
| Diabetes | 1.13 | 1.10-1.17 | 1.20 | 1.14-1.26 | 1.08 | 1.03-1.13 | 0.010 |
| Hypertension | 1.06 | 1.04-1.08 | 1.11 | 1.08-1.13 | 1.02 | 0.99-1.04 | < 0.001 |
| Obesity | 1.16 | 1.14-1.19 | 1.25 | 1.20-1.29 | 1.10 | 1.06-1.13 | < 0.001 |
| Current smoking | 1.09 | 1.07-1.11 | 1.05 | 1.02-1.08 | 1.13 | 1.10-1.16 | < 0.001 |
95%CI: 95% confidence interval; RII: relative index of inequality.
Figures 2 and 3 display the RII for each Spanish region. Regions with a RII further above from one are regions with wider health inequities. We observed heterogeneity by region and by women/men in the RIIs of cardiovascular risk factors by occupational social class. In general, some regions (e.g. Asturias and Balearic Islands) presented higher RII than others (e.g. Galicia, Navarra or Murcia). For high cholesterol, Canarias had the highest RII overall and for women, and the second highest in men. In men, Catalunya had the lowest RII (RII = 0.90), meaning that, for each 1-unit decrease in social class, the prevalence of high cholesterol decreases by 10%. For diabetes, RII tend to be higher in women; the regions with the highest RII were Comunitat Valenciana and Asturias. For hypertension, the RII ranged from 1.23 to 0.91, the highest being Castilla-La Mancha (women) and La Rioja (men). Obesity had the highest RII of all risk factors, specially in women; for instance, women in Asturias had a RII of 1.41 (95%CI: 1.13-1.76). For smoking, there was greater regional variability in RII for women (from 1.32 in Asturias to 0.94 in Castilla-La Mancha) than men.
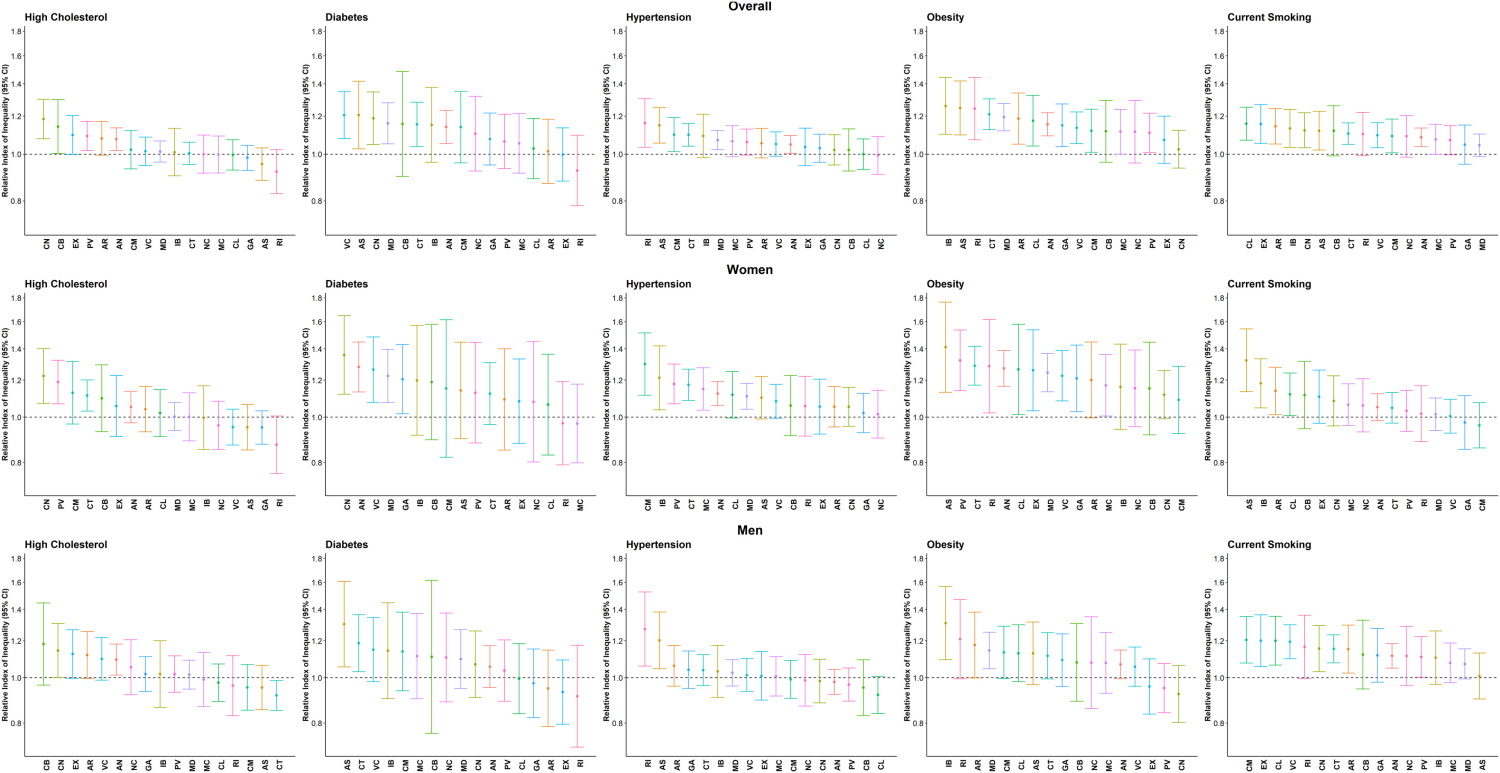
Figure 2. Regional heterogeneity in the the relative index of inequality (RII) for high cholesterol, diabetes, hypertension, obesity and current smoking, sorted by RII. AN: Andalucia; AR: Aragón; AS: Asturias; IB: Balearic Islands; CN: Cannary Islands; CB: Cantabria; CL: Castilla and Leon; CM: Castilla-La Mancha; CT: Catalonia; VC: Comunidad Valenciana; EX: Extremadura; GA: Galicia; MD: Madrid; MC: Murcia; NC: Navarra; PV: Basque Country; RI: La Rioja.
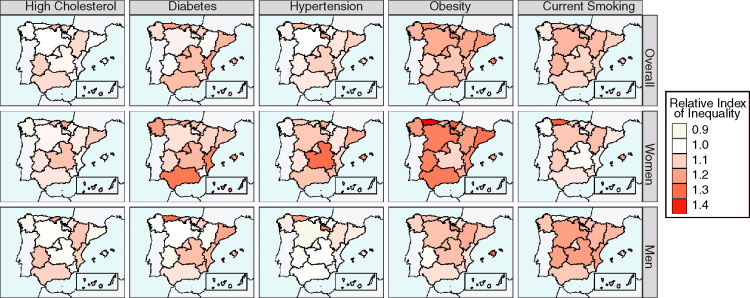
Figure 3. Map showing the spatial heterogeneity in the relative index of inequality (RII) for high cholesterol, diabetes, hypertension, obesity and current smoking.
Supplementary figures II and III show the sensitivity analysis using the slope index of inequality, with similar results between the relative and the absolute measures in women and men. We also repeated the analysis by autonomous community changing the exposure to education (supplementary fig. V) and household income (supplementary fig. VI), showing similar inferences as the main analysis.
Discussion
We found strong inequities in cardiovascular risk factor prevalence by occupational social class in Spain: individuals of disadvantaged social class presented a higher prevalence of high cholesterol, diabetes, hypertension, obesity, and smoking, independent of age. Moreover, we found that social inequities in diabetes, hypertension, and obesity were stronger in women as compared to men, while the inequities in smoking were stronger in men as compared to women. Lastly, we found heterogeneity by region (autonomous communities), with some regions (e.g. Asturias and Balearic Islands) presenting wider social inequities in cardiovascular risk factors than others (e.g. Galicia, Navarra and Murcia).
Social inequities in cardiovascular risk factors by occupational social class and other measures of socioeconomic position have been reported previously in Spain.10,12 Previous studies have reported inequities in cholesterol in Spain10; however, our results were modest and modified by age; as seen in supplementary figure* I, in those < 40, there was an inverse social gradient in high cholesterol that might reflect less frequent visits to healthcare providers. Social inequities in diabetes prevalence have been reported in Spain before,20 and they might be moderated partially by inequities in obesity.14 Regarding hypertension, Regidor et al.21 found that the highest prevalence of hypertension was seen in subjects of disadvantaged occupational social class. Obesity inequities have been also found previously in Spain22; probably due to differences in the intermediate determinants of health (food availability and affordability, walkability), as well as the impact of marketing of unhealthy products, such as cars or fast food. Also, inequities by social class in smoking have been described before,23 with a strong cohort effect and gender intersectionality. Our results were mostly consistent in the sensitivity analyses by education and household income, as another previous study showed.12
The RII for diabetes, hypertension, and obesity was stronger in women compared to men. The excess risk of CVD associated with disadvantaged socioeconomic position is greater for women compared to men,24 potentially mediated by differences in risk factors.7 Specifically, in Spain education inequities in CVD mortality are higher in women than in men.25 Nonetheless, we also found that inequities in smoking were higher in men compared to women, consistent with previous studies showing cohort effects in the association between socioeconomic status and smoking by gender, as the social inequity in smoking for women has only emerged in the last few decades.9 Previous studies have found that absolute measures of inequity in diabetes mortality might be higher in men, and that relative measures are higher for women26; however, in our study, both absolute and relative measures were consistent. All of these observations lend support to the idea of considering the intersectionality of class and gender when studying and designing prevention strategies aiming to reduce health inequities.27 Also, it should be noted that social inequities vary by age, with wider gaps in older ages (as seen in supplementary figure I), as consistent with other studies,10 and a complex relationship with gender in the case of smoking, also consistent with previous studies.9
We observed variation across Spanish autonomous communities in the magnitude of social inequities in cardiovascular risk factors. Previous studies have shown variability in social inequities in health between countries.28 However, the information on subnational heterogeneity of social inequities in health is scarce.29 There might be many reasons, both in context and composition of autonomous communities, that could explain the regional variability in social inequities in CVD risk factors observed in our study. Regarding differences in context, Mackenbach et al.28 suggested in a study of social inequities in 22 European countries that such regional differences might be a reflection of regional differences in educational opportunities, income distribution, or access to health care. This is a key policy issue in Spain, where education or health care competencies are decentralized at the regional (autonomous communities) level. In fact, Costa-Font and Gil29 analyzed determinants of health inequities between 19802001 in Spain and found that regional self-reported health status inequities appeared to be driven by income regional inequities, but not by differences in funding or health expenditure between autonomous communities. Nonetheless, health care competencies to the autonomous communities were not completely transferred until 2002, which was after the study period of the Costa-Font and Gil29 study. Access to healthcare might explain inequities in specific groups, such as undocumented migrants, as there are differences between Autonomous Communities in how their right to access healthcare is guaranteed30; however, it is not likely that this population is well-represented in the Spanish National Health Survey. Also, differences in health care might explain better the heterogeneity in inequities in blood pressure and cholesterol, which may be driven partially by screening inequities by socioeconomic position.31 Moreover, public health policies and interventions aiming to improve health equity also might vary between Spanish regions; in fact, Borrell et al.32 reviewed in 2005 all autonomous community-level health plans in Spain and found that the Basque Country was the autonomous community that had the most recognition for health equity in their plans. However, there is no comprehensive information and evaluation of the impact of public health programs on health equity. An additional contextual explanation might be the presence of non-health interventions that impact health equity, such as neighborhood and urban interventions. For instance, in Catalonia, the urban renewal intervention known as the Neighborhood Law (Llei de Barris), seemed to prevent poor mental health increases in both sexes and especially among the lowest social classes.33 Regarding differences in composition, there is the possibility that there are differences in who gets to be in advantaged vs disadvantaged occupation social classes in the different regions. For instance, migrants tend to be of more disadvantaged social class34 and these populations have different cardiovascular risk profiles than local populations35; therefore, regions with a greater proportion of migrant residents might present different health inequities by social class. Catalunya, Murcia, Balearic Islands and Madrid are the regions with more non-EU migrant residents (11.26%, 11.20%, 9.57% and 8.85%, respectively36); however, these regions don't have clearly higher or lower inequities in our study. Also, the length of stay should be taken into account as health status of migrants may vary by length of stay in the host country.37 Future studies should test how regional characteristics (both contextual and compositional) could explain the heterogeneity of health inequities between regions.
We acknowledge that this study presents several limitations. First, this a descriptive cross-sectional study, so we cannot infer causality; however, the results of the study are consistent with previous findings, both in Spain and other countries. Second, cardiovascular risk factors measures were based on self-reported measures on previous diagnoses, which could introduce information bias; nevertheless, data on self-reported cardiovascular risk factors are a widely used cost-effective method for population health studies. Moreover, validity of health surveys might not vary by socioeconomic position.38 Third, there might different use by social class in health care use which can bias knowledge about cardiovascular risk factors; however, the direction of the potential bias is difficult to estimate; on the one hand, people of disadvantaged social class in Spain visit general practitioners more frequently; on the other hand, men and women of advantaged social position use private health care services more frequently where they can have screening of cardiovascular risk factors.39 Additionally, previous studies have shown that under-diagnosis of some cardiovascular risk factors, such as diabetes, might not follow a social gradient.40
Last, we did not test for the mechanisms by which the regional differences are present, although we have attempted to discuss some of the key potential mechanisms involved. Future studies should look at these mechanisms.
This study may have important implications. Social class reflects experiences and exposures during the life course, representing access to material resources relevant for health, as well as aspects relevant to job characteristics, such as environmental exposures or physical risks. In this study, we found that social inequities in cardiovascular risk factors varied between regions. Autonomous communities in Spain have political control over relevant aspects such as education or health; thus, encouraging social policies and strong cardiovascular preventive actions at the regional level may be effective equitable population prevention strategy.3
In conclusion, we found social inequities in the prevalence of cardiovascular risk factors among the adult population in Spain. Individuals of disadvantaged social class showed a higher prevalence of high cholesterol, diabetes, hypertension, obesity, and smoking, as compared to individuals of higher social class. These social inequities were generally larger for women than for men calling for an intersectional approach between gender and social class. Also, we found heterogeneity by autonomous community with some presenting wider social inequities than others. Education, social, economic, and health policies at the regional level could reduce health inequities in cardiovascular risk factors and, thus, prevent CVD.
What is known about the topic?
Previous studies have shown that there are social inequities in cardiovascular disease risk factors; however, there is scarce information on studies looking at the sub-national heterogeneity in these inequities.
What does this study add to the literature?
Social class inequities in the prevalence of diabetes, hypertension, and obesity were stronger for women compared to men. There was heterogeneity by autonomous communities, with some regions (e.g. Asturias and Balearic Islands) presenting wider social inequities in cardiovascular risk factors than others (e.g. Galicia, Navarra or Murcia). This is a key issue in countries like Spain, which has a territorial organization with markedly autonomous regional governments with legislative power over social welfare aspects, including health care and education














