Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.102 no.6 Madrid jun. 2010
CARTAS AL DIRECTOR
Gastric lipoma - an unusual cause of upper gastrointestinal bleeding
Lipoma gástrico: una causa rara de hemorragia digestiva alta
Palabras clave: Hemorragia digestiva alta. Estómago. Lipoma.
Key words: Upper gastrointestinal bleeding. Stomach. Lipoma.
Dear Editor,
Gastrointestinal lipomas are benign, non-epithelial, slowly growing tumors. The majority are located in the colon (60-75%), followed by the small bowel (20-25%). Gastric lipomas (GLs) are rare and usually located in the antrum (1,2).
Case report
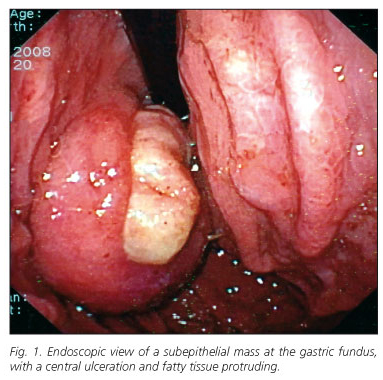
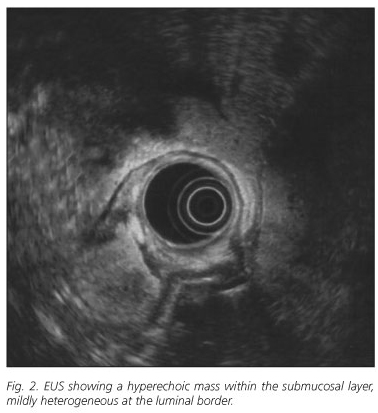
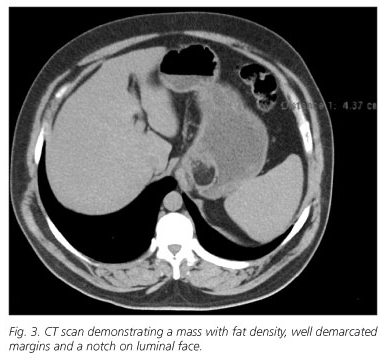
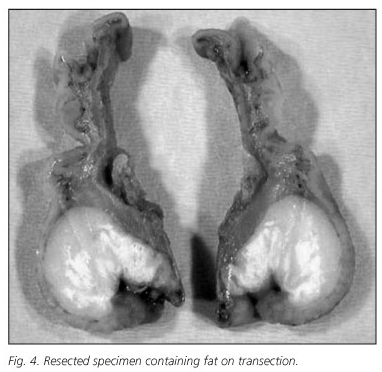
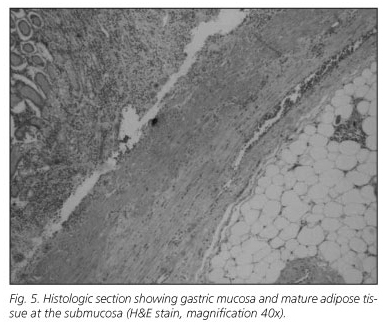
We report the case of a 44-year-old man that was admitted to the emergency department with a history of tiredness and intermittent melena for the previous month. He denied abdominal pain, dyspeptic symptoms, and anorexia or weight loss; there was no intake of non-steroidal anti-inflammatory drugs. Past medical history was significant for arterial hypertension, obesity and sleep apnea syndrome. An esophagogastroduodenoscopy (EGD) performed 5 years earlier was described as normal. Physical examination was unremarkable, except for pallor and obesity (body mass index 34 kg/m2). Laboratory tests showed a decreased hemoglobin (7,8 g/dL); the remaining blood cell count and chemistry profile were within normal limits. Emergency EGD revealed a subepithelial mass at the gastric fundus, approximately 4 cm in diameter, with a central ulceration where a yellowish tissue suggestive of fat was protruding (Fig. 1) -a lipoma or liposarcoma was suspected. An endoscopic ultrasonography (EUS) was performed, showing a hyperechoic mass within the submucosal layer, mildly heterogeneous at the luminal border (Fig. 2). A computerized tomography (CT) was also performed which revealed a homogeneous mass with fat density in the gastric fundus, with well demarcated margins, with a notch on the side facing the lumen (corresponding to the ulceration saw at EGD); no secondary lesions were present (Fig. 3). The patient was submitted to partial gastric resection (Fig. 4) and was discharged 10 days after the procedure; no incidents were reported. Histological examination confirmed the diagnosis of submucosal lipoma and ulceration of the overlying mucosa (Fig. 5).
Discussion
Gastric lipomas (GLs) are rare, representing 3% of all benign tumours of the stomach and 5% of all the gastrointestinal lipomas; 75% are located in the antrum and the vast majority (95%) are submucosal (1). Although they are usually asymptomatic and detected incidentally, severe symptoms can occur with larger lesions (> 2 cm), such as hemorrhage, obstruction or abdominal pain. Gastrointestinal hemorrhage is the most common symptom (in over 50% of patients), occurring due to pressure necrosis and ulceration of the mucosa (3).
At EGD, GLs appear as smooth, soft masses with a normal overlying mucosa; a yellowish colour, the "tenting" sign (easy retraction of the overlying mucosa with a biopsy forceps) and the "cushion" sign (impression after compressing the mass with the biopsy forceps) help to identify these lesions (1). Biopsy is usually not diagnostic due to the submucosal nature of the lesion.
CT is highly specific for lipomas (4), showing well circumscribed submucosal masses with uniform fat density (-70 to -120 Hounsfield Units), although thin fibrous septations inside the mass are not uncommon (5). EUS has been reported for the excellent diagnosis accuracy of GLs, the typical findings being homogeneous hyperechoic tumours within the submucosal layer (6). If ulceration is present, the lipomatous characteristics may be masked on both exams, due to inflammation and scar into the tumor (4), as occurred in our case.
The treatment of GLs is still controversial. For small, submucosal lesions, endoscopic resection is a safe procedure, although mere observation is a valid option, because malignant degeneration has not been reported (7). For the majority of authors, surgical resection remains the treatment of choice for larger, symptomatic GLs (1), but the endoscopic resection has gained importance even in this field. Reports of successful endoscopic removal, without major complications (hemorrhage or perforation) have been published (8).
A. Sadio1, P. Peixoto1, A. Castanheira1, E. Cancela1, P. Ministro1, C. Casimiro2 and A. Silva1
Departments of 1Gastrenterology and 2Surgery. São Teotónio Hospital. Viseu, Portugal
References
1. Maderal F, Hunter F, Fuselier G, et al. Gastric lipomas -an update of clinical presentation, diagnosis and treatment. Am J Gastroenterol 1984; 79: 964-7. [ Links ]
2. Agha FP, Dent TL, Fiddian-Green RG, et al. Bleeding lipomas of the upper gastrointestinal tract. A diagnostic challenge. Am Surg 1985; 51: 279-85. [ Links ]
3. Johnson DC, DeGennaro VA, Pizzi WF, et al. Gastric lipomas: a rare cause of massive upper gastrointestinal bleeding. Am J Gastroenterol 1981; 75: 299-301. [ Links ]
4. Park SH, Han JK, Kim TK, et al. Unusual gastric tumours: radiologic-pathologic correlation. Radiographics 1999; 19: 1435-46. [ Links ]
5. Thomson WM, Kende AI, Levy AD. Imaging characteristics of gastric lipomas in 16 adult and pediatric patients. Am J Roentgenol 2003; 181: 981-5. [ Links ]
6. Yasuda K, Cho E, Nakajiama M, et al. Diagnosis of submucosal lesions of the upper gastrointestinal tract by endoscopic ultrasonography. Gastrointest Endosc 1990; 36: 517-20. [ Links ]
7. Alberti D, Grazioli L, Orizio P, et al. Asymptomatic giant gastric lipoma: what to do? Am J Gastroenterol 1999; 94: 3634-7. [ Links ]
8. Yu HG, Ding YM, Tan S, et al. A safe and efficient strategy for endoscopic resection of large, gatrointestinal lipoma. Surg Endosc 2007; 21: 265-69. [ Links ]