Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.103 no.3 Madrid mar. 2011
Laparoscopy versus open surgery for advanced and resectable gastric cancer: a meta-analysis
Laparoscopia versus cirugía abierta en el cáncer gástrico avanzado y resecable: una meta-análisis
David Martínez-Ramos1, Juan Manuel Miralles-Tena1, Miguel A. Cuesta2, Javier Escrig-Sos1, Donald van der Peet2, Jane S. Hoashi1 and José Luis Salvador-Sanchis1
1Department of General and Digestive Surgery. Hospital General de Castellón. Castellón, Spain.
2Department of Gastrointestinal Surgery. Vrije Universiteit Medisch Centrum. Amsterdam, Netherlands
ABSTRACT
Background: there are few studies in the literature comparing laparoscopic versus open Gastrectomy, predominantly for advanced gastric cancer (AGC). Most of the available studies and meta-analysis compare both approaches in the early gastric cancer. The meta-analysis, here presented, compares the clinical outcomes between these two procedures for AGC.
Objectives: to evaluate the current status of both partial and total laparoscopic gastrectomy (LG), with regard to its short and long-term outcomes by comparing it to conventional open gastrectomy (OG) for AGC.
Data sources and review methods: original articles published in English language from January 1991 to October 2009 were searched in the Medline, Embase, Current Contents, Science Citation Index databases and Cochrane Controlled Trials Register. All articles comparing LG and OG for AGC were included, and those comparing outcomes only for early gastric cancer (EGC) were excluded. Clinical appraisal and data extraction were conducted independently by 3 reviewers. Statistical analysis was carried out following the DerSimonian-Laird random effects model.
Results: out of 2,344 studies, 7 studies were selected. One prospective randomized controlled trial, one comparative prospective study and five comparative retrospective studies were analyzed. These studies include a total of 452 patients with gastric cancer, 174 patients in the LG and 278 in the OG. The analyzed result variables were operative time, operative blood loss, hospital postoperative stay, number of dissected lymph nodes and cancer-related mortality risk. Compared to OG, LG was a longer procedure: weighted mean difference (WMD) 44 minutes; 95% confidence interval (CI) 20 to 69; I-squared = 91.6%, but was associated with a lower blood loss (WMD -122 cc; 95% CI -208 to -37; I-squared = 90.8%); this was more significant for hospital operative stay (WMD -6.2 days; 95% CI -9.4 to -2.8; I-squared = 67.8%). Moreover there were no significant differences between the two groups concerning the number of dissected lymph nodes (WMD -1.57; 95% CI -3.41 to 0.26; I-squared = 8.3) and no significant differences for cancer-related mortality risk (adjusted for 60 months of follow-up) although there was a tendency toward a protective effect for LG (Odds Ratio 0.53; 95% CI 0.23 to 1.22; I-squared 41%).
Conclusion: laparoscopic total and partial gastrectomy for AGC is associated with a longer operative time but lower blood loss and shorter postoperative hospital stay. Moreover there were similar outcomes between both approaches in terms of number of dissected lymph nodes and long-term follow-up (survival).
Key words: Advanced gastric cancer surgery. Laparoscopic gastrectomy. Open gastrectomy. Meta-analysis.
Introduction
Laparoscopic surgery has been shown to provide important advantages on the short term when compared to open surgery for the treatment of several malignant diseases with at least the same long term survival (1-6).
However, while laparoscopic surgery has been accepted worldwide for selected GIST tumors, early gastric cancer (EGC) and morbid obesity surgery, its application in advanced gastric cancer (AGC) has not been generalised. In fact, there are only a few studies in English scientific literature comparing laparoscopic and open gastrectomies for non-early gastric cancer (7-13). While a number of meta-analysis and systematic reviews have been published for EGC (14-18), such studies have not been conducted for a majority number of cases with AGC. Treatment options and outcomes clearly differ for both stages of gastric cancer; as a consequence, the results of laparoscopic surgery for EGC cannot be directly applied to AGC.
We present the first meta-analysis comparing laparoscopy to open surgery predominantly in advanced gastric cancer. Surgically-related and long-term follow-up results are discussed according to the best scientific literature available.
Methods
Literature search
The literature search began with original articles written in English for laparoscopy treatment for gastric cancer from January 1991 to October 2009 in the following databases: Medline, Currents Contents, and Science Citation Index, Embase, and Cochrane registry. A total of 2,344 articles were selected.
Literature review. Inclusion and exclusion criteria
The first step consisted of including all articles comparing laparoscopic and open surgery for gastric cancer. Only those articles referring to either of the techniques were included. Those referring to combined procedures or non-surgical procedures were excluded.
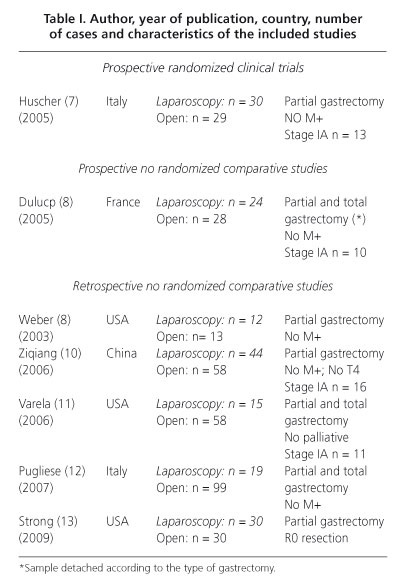
The second step consisted of excluding articles referring only or predominantly to EGC. After the exclusion process, only one randomized controlled clinical trial fulfilled these requirements (7). We therefore included prospective and retrospective studies of higher quality in our meta-analysis. It was essential for the prospective and retrospective non-randomized studies to provide information on certain variables including operating time, blood loss, hospital stay, number of harvested lymph nodes and deaths due to gastric cancer during the follow-up (8-13). Quality evaluation was done by 3 reviewers, who agreed to finally include 7 articles (Fig. 1). Characteristics of the 7 chosen articles are shown in table I. In one of them (9), it was possible to individualize data for partial and total gastrectomy and some of the variables could be analyzed.
Statistical analysis
Quantitative variables
From each included study, quantitative variables (operating time, blood loss, postoperative hospital stay, number of harvested lymph nodes and survival) were obtained. The number of cases, mean and standard deviation were collected from both laparoscopic and open surgery groups. When a study reported a range and not a standard deviation, the standard deviation was estimated by dividing the range amplitude by 4. When the mean was not reported, for small samples (< 25 observations), it was estimated according to the formula proposed by Hozo et al. (19):
Mean = (low end of the range + (2 x median) + high end of the range) / 4
According to these authors, for samples with ≥ 25 observations, the best estimator of the mean is just the median. Articles not reporting mean, range or median were excluded from the study.
Due to the rather heterogeneous selection of studies, the model for random effects based on the DerSimonian-Laird method was chosen for calculating the Weighted Mean Differences (WMD) and their confidence intervals.
Heterogeneity was measured with I2 index and p-value.
Qualitative variables
For qualitative variables (risk of death related to gastric cancer in the follow-up) the Odds Ratio (OR) was calculated for each study, by the mean number of deaths over the total number of patients, for both open and laparosocopic surgeries. The total number of cases for each group was modified according to Vale (20) and Tierney (21) in order to uniformly adjust the follow-up time to 60 months. The weighted summary OR was calculated following DerSimonian-Laird's model, with the number of events in each group, and the total number of cases after the 60-month follow-up adjustment. Heterogeneity was also calculated by using I2 index and p-value.
Forest graphs, including data from all selected articles, were done for each variable. Publication bias was evalua-ted following the method proposed by Egger (22). All statistical calculations were performed using STATS DIRECT version 2.7.
Results
The 7 selected studies included a total of 452 patients with advanced gastric cancer, resected with curative intention; 174 patients were in the laparoscopic surgery group, and 278 patients were in the open surgery group. Demographic information, ASA classification and tumour characteristics (stage, histological type, etc.), were similar and not statistically different for type of surgery, in all studies.
Operating time
The result was favourable for open surgery because the operating time is lower than in the laparoscopic approach, with a WMD of 44 minutes less (p < 0.001). However, this result was influenced by the level of heterogeneity (I2 = 91.6%), especially by the particular results of Weber (8), Ziqiang (10), and Strong (13), whose average differences are around 1 or more hours (Fig. 2). In spite of this, the general tendency of the differences seems to show laparoscopy to consume more surgery time than open surgery.
Operating blood loss
The result was favourable for laparoscopic surgery with a WMD of blood loss of less than 122 millilitres compared to open surgery (p = 0.005). The general tendency of each study was favourable for laparoscopic surgery (Fig. 3) but with high differences between them, resulting in a high heterogeneity (I2 = 90%).
Number of dissected lymph nodes
The WMD of harvested lymph nodes seems to be in favour of open surgery in 1.57 lymph nodes, although this finding is not statistically significant (p = 0.093). We cannot talk about a common tendency in the studies, although none of them showed statistically significant differences, and each particular difference was similar to the others (Fig. 4). The heterogeneity was not high (I2 = 8.3%), meaning that the result seems to be reliable and represents rather well the differences due to the technique.
Postoperative stay
Postoperative stay was shorter for the laparoscopic approach with a WMD of 6 days (p < 0.001). This result is derived from a similar tendency in all articles, which showed a statistically significant advantage for laparoscopy (Fig. 5). Nevertheless, a noteworthy heterogeneity was seen (I2 = 67.8%), especially due to Strong et al.'s article (13).
Survival
Tumour-related mortality, adjusted at 5-year follow-up, showed a favourable tendency for laparoscopic surgery (OR = 0.53), although not statistically significant (p = 0.191). This could be explained by the low number of included articles, and the result being negatively affected by a moderate level of heterogeneity (I2 = 41%), mainly due to Dulucq et al.'s (9) study of a surprising OR = 0.09 in favour of laparoscopy (Fig. 6).
No publication bias was statistically detected. Nevertheless, due to the low number of included articles, and the particular characteristics of each, this must be carefully taken into consideration.
Discussion
Laparoscopic approach has been shown to be an effective alternative to open surgery for treatment of several benign pathologies of the stomach, such as resection of GIST tumors and early gastric cancer. In Europe, the first series of laparoscopic gastric resections for gastric cancer was published by Azagra et al. 10 years ago (23). Since then, the laparoscopic approach has gained acceptance for treating gastric cancer, though not as quickly as other malignancies like colon cancer (24-26). It is possible that anatomical and surgical difficulties such as the type of lymphadenectomy and difficult anastomosis, as well as a lower number of cases involved, justify this delay in its diffusion.
For gastric cancer, the adequacy of surgical margins and the extension of lymphadenectomies using the laparoscopic approach have been repeatly reported. However, some important aspects, especially those referring to advanced gastric cancer, remain uncertain. In fact, as this meta-analysis reflects, there are only a few studies with an acceptable level of evidence. In addition, most of the recent publications refer to EGC, and their results should not be directly extrapolated to AGC.
In regions with high incidences of gastric cancer (Japan, China), there are population-based screening programs, in which 50-80% of gastric cancers are diagnosed at an early stage (27). Moreover, there are substantial differences between the Eastern and Western cultures with regard to the characteristics of the populations; Western patients are on average 10 years older, and have higher rates of cardiovascular disease, overweight, and are at a higher risk for postoperative thromboembolic events (28). Besides, in Japan, reports on survival rates are systematically higher than in Western countries (29). We can therefore assume that our meta-analysis reflects a synthesis of both worlds regarding AGC, since it combines Western and Eastern results.
With regard to operative time, although the learning curve is already in a plateau phase for some groups, laparoscopic gastric resection is a time-consuming procedure (30). In fact, according to some authors, this learning curve will involve about 60-90 cases (31). Nevertheless, recent and continuous technological improvements have reduced this time and it is reasonable to think that it will decrease in the future (32). In our study, differences between the open and laparoscopic approach showed a high heterogeneity. We therefore cannot affirm that these differences (40 minutes on average) are exact and universal. Hence, the heterogeneity should indicate that the observed differences could be due to differences among surgeons or other unknown factors and not to differences between surgical techniques per se.
A similar explanation can be made for intraoperative blood loss, where differences can be not only a consequence of surgical approach but also of surgical general management. Again, differences between series are present. Moreover, it is also possible that surgical difficulties influence the results. During the selection process in non-randomized studies, it is possible that favourable patients were included in one group and not in the other, something that would directly affect the results of meta-analysis. As a consequence, the real magnitude of this variable remains unclear. In any case, the clinical importance of the observed differences (< 300 mL) would not be relevant.
The extension of lymphadenectomies was similar for both approaches. The moderate heterogeneity and the non-significant final result in comparing the approaches seem to support this affirmation. Moreover, we believe that the observed difference (1.57 lymph nodes, in absolute values) is not clinically significant for staging or for the prognosis of a more extended lymphadenectomy.
Postoperative stay was notably favourable for laparoscopic surgery but, once again, heterogeneity was high, therefore questioning in some extent the result. Although postoperative stay is affected by a number of postoperative factors (paralytic ileum, oral intake, pain, blood-loss, complications, etc.) it is possible that heterogeneity was a reflection of any of these non-individually analyzed variables.
The 5-year survival analysis did not provide a clear conclusion. Although concrete estimation benefits the laparoscopic approach, only a few articles are available regarding this, showing a rather significant heterogeneity with no statistically significant differences among them. As a result, there is no evidence that differences exist regarding 5-year survival for open vs. laparoscopic surgery for AGC. More clinical trials with this specific objective in mind, with larger sample size and higher scientific quality are necessary to definitively answer this question.
Some limitations of our article must be addressed. The final number of articles included is low because of the lack of high quality articles available in the literature. Therefore, we decided to add comparative but non-randomized studies, including a retrospective study, which can bias the final outcome. If a bias was present, it was not detected in our study. Nevertheless, our results must be interpreted with caution, taking into consideration the potential influence of bias, especially when concerning high levels of heterogeneity. On the other hand, although heterogeneity is a negative factor in a meta-analysis, it can be helpful in showing us aspects that must be developed and investigated (33). Future research, focusing on high quality randomised clinical trials will most likely resolve these issues. We can expect these studies to appear, as in other malignant tumours (5), as these procedures become more popular among surgeons (34).
In summary, from this meta-analysis only two reliable conclusions can be made in spite of different levels of heterogeneity: a) there were similar outcomes between both approaches in terms of number of dissected lymph nodes and long-term follow-up (survival); and b) laparoscopic gastrectomy for AGC is associated with a longer operative time but lower blood loss and shorter postoperative hospital stay. Moreover and due to several reasons that affect heterogeneity, these results should be observed with caution and not definitive. It is important to focus on future randomized prospective studies for analysing short and long-term results, especially 5-year survival, of laparoscopic surgery for AGC.
Final note and acknowledgments
This article is dedicated in memoriam of its predecessor, Dr. Juan Manuel Miralles-Tena, who passed away when the first version of the manuscript was close to being written.
The authors would like to thank the Valencian Society of Surgery (Sociedad Valenciana de Cirugía) and Hospital Provincial Foundation (Fundación Hospital Provincial) for their financial support.
Our acknowledgments go out to the Department of Statistics of Jaume I University of Castellón (Universitat Jaume I) and the Department of Epidemiology and Statistics of Vrije University Medical Center of Amsterdam (Netherlands), especially to Dr. Elly de Lange.
References
1. Iwanaka T, Arkovitz MS, Arya G, Ziegler MM. Evaluation of operative stress and peritoneal macrophage function in minimally invasive operations. J Am Coll Surg 1997;184:357-63. [ Links ]
2. Gupta A, Watson DI. Effect of laparoscopy on immune function. Br J Surg 2001;88:1296-306. [ Links ]
3. Schwenk W, Bohm B, Muller JM. Postoperative pain and fatigue after laparoscopic or conventional colorectal resections: a prospective randomized trial. Surg Endosc 1998;12:1131-6. [ Links ]
4. Glavic Z, Begic L, Simlesa D, Rukavina A. Treatment of accute cholecystitis. A comparison of open vs laparoscopic cholecystectomy. Surg Endosc 2001;15:398-401. [ Links ]
5. Reza MM, Blasco JA, Andradas E, Cantero R, Mayol J. Systematic review of laparoscopic versus open surgery for colorrectal cancer. Br J Surg 2006;93:921-8. [ Links ]
6. Petrakis IE, Kogerakis NE, Drositis IE, Lasithotakis KG, Bouros D, Chalkiadakis GE. Video-assisted thoracoscopic surgery for thoracic empyema: primarily, or after fibrinolytic therapy failure? Am J Surg 2004;187:471-4. [ Links ]
7. Huscher CGS, Mingoli A, Sgarzini G, Sansonetti A, Di Paola M, Recher A, et al. Laparoscopic versus open subtotal gastrectomy for distal gastric cancer: five-year results of a randomized prospective trial. Ann Surg 2005;241:232-7. [ Links ]
8. Weber KJ, Reyes CD, Gagner M, Divino CM. Comparison of laparoscopic and open gastrectomy for malignant disease. Surg Endosc 2003;17:968-71. [ Links ]
9. Dulucq JL, Wintringer P, Stabilini C, Solinas L, Perissat J, Mahajna A. Laparoscopic and open gastric resections for malignant lesions: a prospective, comparative study. Surg Endosc 2005;19: 933-8. [ Links ]
10. Ziqiang W, Feng Q, Zhimin C, Miao W, Lian Q, Huaxing L, et al. Comparison of laparoscopically assisted and open radical distal gastrectomy with extended lymphadenectomy for gastric cancer management. Surg Endosc 2006;20:1738-43. [ Links ]
11. Varela JE, Hiyashi M, Nguyen T, Sabio A, Wilson SE, Nguyen NT. Comparison of laparoscopic and open gastrectomy for gastric cancer. Am J Surg 2006;192:837-42. [ Links ]
12. Pugliese R, Maggioni D, Sansonna F, Scandroglio I, Ferrari GC, Di Lernia S, et al. Total and subtotal laparoscopic gastrectomy for adenocarcinoma. Surg Endosc 2007;21:21-7. [ Links ]
13. Strong VE, Devaud N, Allen PJ, Gonen M, Brennan MF, Coit D. Laparoscopic versus open subtotal gastrectomy for adenocarcinoma: A case-control study. Ann Surg Oncol 2009;16:1507-13. [ Links ]
14. Kitano S, Shiraishi N, Fujii K, Yasuda K, Inomata M, Adachi Y. A randomized controlled trial comparing open vs laparoscopy-assisted distal gastrectomy for the treatment of early gastric cancer: an interim report. Surgery 2002;131:S306-S311. [ Links ]
15. Lee JH, Han HS, Lee JH. A prospective randomized study comparing open vs laparoscopy-assisted distal gastrectomy in early gastric cancer: early results. Surg Endosc 2005;19:168-73. [ Links ]
16. Hayashi H, Ochiai T, Shimada H, Gunji Y. Prospective randomized study of open versus laparoscopy-assisted distal gastrectomy with extraperigastric lymph node dissection for early gastric cancer. Surg Endosc 2005;19:1172-6. [ Links ]
17. Hosono S, Arimoto Y, Ohtani H, Kenamiya Y. Meta-analysis of short-term outcomes after laparoscopy-assisted distal gastrectomy. World J Gastroenterol 2006;12:7676-83. [ Links ]
18. Memon MA, Khan S, Yunus RM, Barr R, Memon B. Meta-analysis of laparoscopic and open distal gastrectomy for gastric carcinoma. Surg Endosc 2008;22:1781-9. [ Links ]
19. Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of sample. BMC Medical Research Methodology 2009;5:13. [ Links ]
20. Vale CL, Tierney JF, Stewart LA. Effects of adjusting for censoring on meta-analyses of time-to-event outcomes. Int J Epidemiol 2002; 31:107-11. [ Links ]
21. Tierney JF, Stewart LA, Ghersi D, Burdett S, Sydes MR. Practical methods for incorporating summary time-to-event data into meta-analysis. Trials 2007;8:16. [ Links ]
22. Egger M, Smith GD, Altman DG. Systematic reviews in health care. Meta-analysis in context. London: BMJ Books; 2001. [ Links ]
23. Azagra JS, Goergen M, DeSimone P, Ibañez J. Minimally invasive surgery for gastric cancer. Surg Endosc 1999;13:351-7. [ Links ]
24. Campillo-Soto A, Torralba-Martínez JA, Martín-Lorenzo JM, Lirón-Ruiz R, Bento-Gerard M, Pérez-Cuadrado E, et al. Gastrojejunal anastomosis stricture after laparoscopic gastric bypass. Our experience with 62 patients. Rev Esp Enferm Dig 2010;102:187-92. [ Links ]
25. Ibáñez Aguirre FJ, Azagra JS, Erro Azcárate ML, Goergen M, Rico Selas P, Moreno Elola-Olaso A, et al. Laparoscopic gastrectomy for gastric adenocarcinoma. Long-term results. Rev Esp Enferm Dig 2006;98:491-500. [ Links ]
26. E. M. Targarona, X. Feliu1 and C. Balagué. Laparoscopic management of gastric cancer Rev Esp Enferm Dig (Madrid) 2006; 98: 485-490. [ Links ]
27. Dicken BJ, Bigam DL, Cass C, Mackey JR, Joy AA, Hamilton SM. Gastric adenocarcinoma: review and considerations for future directions. Ann Surg 2005;241:27-39. [ Links ]
28. Griffin SM. Gastric cancer in East: same disease, different patient. Br J Surg 2005;92:1055-6. [ Links ]
29. Bonenkamp JJ, Hermans J, Sasako M, van de Velde CJ, Welvaart K, Sogun I, et al. Extended lymph-node dissection for gastric cancer. N Engl J Med 1999;340:908-14. [ Links ]
30. Fujiwara M, Kodera Y, Kasai Y, Kanyama Y, Hibi K, Ito K et al. Laparoscopy-assisted distal gastrectomy with systemic lymph node dissection: a phase II study following the learning curve. J Surg Oncol 2005;91:26-32. [ Links ]
31. Zhang X, Tanigawa N. Learning curve of laparoscopic surgery for gastric cancer, a laparoscopic distal gastrectomy-based analysis. Surg Endosc 2008; Sep 24 (Springer Online). [ Links ]
32. Adachi Y, Shiraishi N, Shiromizu A, Bandoh T, Aramaki M, Kitano S. Laparoscopy-assisted Billroth I gastrectomy compared with conventinal open gastrectomy. Arch Surg 2000;135:806-10. [ Links ]
33. Naylor CD. Meta-analysis and the meta-epidemiology of clinical research. BMJ 1997;315:617-9. [ Links ]
34. Strong VE, Devaud N, Karpeh M. The role of laparoscopy for gastric surgery in the West. Gastric Cancer 2009;12:127-31. [ Links ]
![]() Correspondence:
Correspondence:
David Martínez Ramos.
Servicio de Cirugía General y Digestiva.
Hospital General Universitario de Castellón.
Avenida Benicasim, s/n
12004. Castellón. Spain.
e-mail: davidmartinez@comcas.es
Received: 16-09-10.
Accepted: 14-10-10.