Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.104 no.1 Madrid ene. 2012
https://dx.doi.org/10.4321/S1130-01082012000100014
LETTERS TO THE EDITOR
Idiopathic portal hypertension complicated by ischemic hepatitis: the diagnostic importance of hemodynamics and liver biopsy
Hipertensión portal idiopática complicada con hepatitis isquémica: importancia diagnóstica de la biopsia y la hemodinámica hepáticas
Key words: Idiopathic portal hypertension. Hepatosclerosis. Noncirrhotic liver fibrosis. Incomplete septal cirrhosis. Nodular transformation of Delhi. Presinusoidal. Esophageal varices. Splenomegaly.
Palabras clave: Hipertensión portal idiomática. Hepatoesclerosis. Fibrosis hepática no cirrótica. Cirrosis septal incompleta. Transformación nodular Delhi. Presinusoidal. Varices esofágicas. Esplenomegalia.
Dear Editor,
The etiology of idiopathic portal hypertension (IPH) is unknown. IPH is characterized by periportal fibrosis, portal hypertension, the formation of esophageal varices, and the development of portosystemic collateral vessels, splenomegaly, and secondary hypersplenism, all of which appear in the absence of hepatic cirrhosis (1). However, there are clinical situations that can coexist with IPH that render its diagnosis difficult, as we experienced in a patient in whom the presentation was complicated by ischemic hepatitis and abnormal liver enzymes. In most cases, liver biopsy and portal pressure measurements are sufficient to make the correct diagnosis.
Case report
Our patient was a 32-year-old man who was diagnosed with Fanconi anemia 20 years earlier progressing into acute myeloid leukemia M-5. Therefore, he was treated with allogeneic bone marrow transplantation from an HLA-identical sibling at age 26. He presented with Staphiloccocus haemolyticus bacteremia and antigenemia for cytomegalovirus on day 40 after transplantation, as well as iron overload that required regular phlebotomy, after which he experienced complete remission. He did not smoke or consume alcohol.
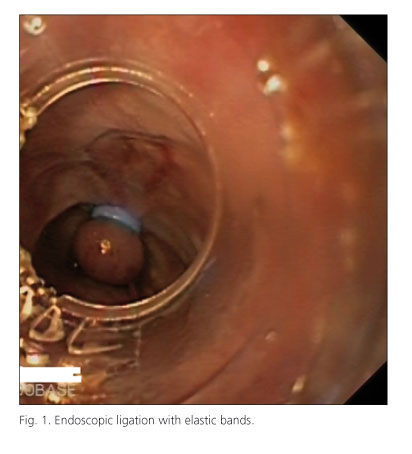
The current disease presented with an episode of gastrointestinal bleeding, secondary to large esophageal varices and a subcardial varix, which was controlled by endoscopic ligation with elastic bands (Fig. 1). After the patient was stabilized, abdominal ultrasonography was performed, revealing signs of chronic liver disease and portal hypertension (increased size of the portal vein, splenomegaly, and splenic hilum shunt; decreased flow in the main portal vein; and mild ascites). The hepatic veins were normal, and there were no hepatic or splenic focal lesions.
The physical examination revealed hepatomegaly of 3 cm, and the blood tests showed AST 615 U/L, ALT 896 U/L, ALP 392 U/L, GGT 284 U/L, and bilirubin 1.3 mg/dL, which coincided with an episode of hypotension secondary to variceal bleeding. These abnormalities in the liver tests normalized once the episode of hypotension subsided. These findings suggested an ischemic hepatitis.
By viral serology, the patient was negative for HAV, HBV, HCV, HIV, CMV, and EBV. Iron, transferrin saturation, ferritin, copper, ceruloplasmin, porphyrin, and alpha-1-antitrypsin levels were also in the normal range. The immunology, proteinograms, and autoimmunity tests were also normal, as was the echocardiogram. Marrow aspiration was consistent with Fanconi anemia and acute myeloid leukemia in remission, for which the erythroid hyperplasia was likely secondary to the previous pathology. No pathological populations were detected by cytometry.
A computed tomography was performed that again showed signs of chronic liver disease, including abnormal homogeneous liver, perivesicular varices and in the splenic hilum and cholelithiasis (Fig. 2). Vascular disease was ruled out (portal vein thrombosis, Budd-Chiari syndrome, etc.).
Based on the negative results of the liver study, ultrasonography-guided liver biopsy was performed, showing cholestasic liver tissue, light ductopenia, reactive ductal neoplasm, marked dilation of venous vascular structures, and focal endothelitis (Fig. 3). Given these findings, we ruled out veno-occlusive disease, chronic graft-versus-host disease (2), and liver cirrhosis and performed a hepatic hemodynamic study. This study showed values of presinusoidal portal hypertension, with multiple veno-venous connections. Based on the clinical, histological, and hepatic hemodynamic examination, we made a diagnosis of IPH.
Discussion
In the presence of portal hypertension, the first diagnosis to rule out is liver cirrhosis, because it is the most common cause of portal hypertension. In this patient, who had a history of Fanconi anemia and bone marrow transplantation, with an increased risk of thrombosis, we ruled out extrahepatic causes of portal hypertension by imaging methods (echocardiography without evidence of tamponade/pericardial effusion, absence of portal, splenic, or hepatic veins thrombosis).
The absence of regenerative nodules in an adequately sized biopsy ruled out liver cirrhosis-essential data for considering other causes of portal hypertension. IPH in the biopsy can show aberrant vascularization, periportal fibrosis, sinusoidal dilatation, microthrombosis, obliteration of small portal vessels, and the absence of hepatocellular damage, but none of these findings is pathognomonic (3).
Therefore, we examined postsinusoidal and presinusoidal intrahepatic causes. Among the former, it must be considered sinusoidal obstruction syndrome, which has been described in patients who have received bone marrow transplants and is linked to chemotherapy. However, this syndrome usually appears 10-20 days after trasplantation (2), which, in addition to portal pressure measurements, consistent with presinusoidal HTP, ruled out this diagnosis. In IPH, pressure in the portal vein is typically increased, with resistance to flow predominantly at presinusoidal levels. The hepatic venous pressure gradient is normal or modestly elevated, whereas portal venous pressure is much greater than intrahepatic pressure (4).
After determining portal pressure, we focused on presinusoidal causes, including schistosomiasis, sarcoidosis, primary biliary cirrhosis, and IPH. Considering the available data, our patient was diagnosed with IPH. We based our diagnosis primarily on the liver biopsy and hepatic hemodynamics, despite the patient experiencing concomitant episodes of ischemic hepatitis with analytical alterations that made us suspect hepatocellular damage.
Pablo Miranda-García1, M.a Carmen López-Martín1, Tomás Álvarez-Malé1, Ma José Casanova-González1,
Cecilio Santander1, Rafael Bañares2, Ricardo Moreno-Otero1,3, and María Trapero-Marugan1
1Hospital Universitario La Princesa. Instituto de Investigación Sanitaria Princesa (IP) and CiberEHD. Madrid, Spain.
2Hospital General Universitario Gregorio Marañón.
3Universidad Autónoma de Madrid. Spain
References
1. Okudaira M, Ohbu M, Okuda K. Idiopathic portal hypertension and its pathology. Semin Liver Dis 2002;22:59-72. [ Links ]
2. DeLeve LD, Valla DC, Garcia-Tsao G. Vascular disorders of the liver. AASLD pactice guidelines. Hepatology 2009;49:1729-64. [ Links ]
3. Seijo-Rios S, García-Pagan JC. Hipertensión portal idiopática. Gastroenterol Hepatol 2010;33:179-90. [ Links ]
4. Sarin SK, Kumar A. Noncirrhotic portal hipertensión. Clin Liver Dis 2006;10:627-51. [ Links ]











 texto en
texto en