Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.107 no.5 Madrid may. 2015
ORIGINAL PAPERS
Accuracy for optical diagnosis of colorectal polyps in clinical practice
Precisión del diagnóstico óptico de pólipos de colon en la práctica clínica
Javier Sola-Vera, Rubén Cuesta, Francisco Uceda, Elena Morillo, Estefanía Pérez, María Dolores Pico, Jesús Sáez, Eva Girona, Lidia Buendía and Marifé García-Sepulcre
Endoscopy Unit. Digestive Medicine Department. Hospital General Universitario de Elche. Elche, Alicante. Spain
ABSTRACT
Background: Optical diagnostic involves predicting polyp histopathology from its endoscopic characteristics. It is only recommended for diminutive polyps (≤ 5 mm) and for predictions made with high confidence.
Objectives: To evaluate the accuracy of optical imaging in clinical practice and to assess if optical diagnosis is useful for predicting future colonoscopy surveillance intervals without waiting for histopathological analysis.
Methods: consecutive > 18 years patients were enrolled in this prospective study. Colonoscopies were performed by five expert endoscopists who previously participated in an ex-vivo training. Colonoscopes CF-H180AL and CF-Q180AL were used together with Exera II (Olympus Medical System, Tokyo, Japan) processors. Each polyp was characterized in real time using white light and Narrow Band Imaging. Accuracy of optical diagnosis (S, E, NPV, PPV) and correlation between surveillance interval based on optical diagnosis and histopathological analysis were calculated.
Results: 311 colon polyps < 10 mm (216 diminutive) in 195 patients were analyzed. Accuracy of optical diagnostics for predictions made with high confidence: Diminutive polyps (sensitivity 0.59, specificity 0.92, NPV 0.48); polyps < 10 mm (sensitivity 0.73, specificity 0.88, NPV 0.50). An optical diagnosis based surveillance recommendation was given to 90 patients. Concordance with histopathology based recommendation was 92.2% according to the European guideline and 93.3% according to the ESGE guideline.
Conclusions: Optical diagnostics can be used to predict future surveillance intervals immediately after colonoscopy. However, in this study, based on clinical practice, the accuracy of optical imaging is below the recommended standards.
Key words: Sensitivity and specificity. Colonoscopy. Colorectal polyps. Optical diagnosis.
RESUMEN
Antecedentes: el diagnostico óptico consiste en predecir la histopatología de un pólipo a partir de sus características endoscópicas. Sólo es recomendable para pólipos diminutos (≤ 5 mm) y para predicciones realizadas con alta confianza.
Objetivos: evaluar la precisión del diagnóstico óptico en la práctica clínica habitual y valorar si es posible recomendar un intervalo de seguimiento basado en diagnóstico óptico sin esperar el análisis histopatológico.
Métodos: estudio prospectivo con pacientes consecutivos > 18 años. Las colonoscopias fueron realizadas por 5 endoscopistas expertos que realizaron previamente un entrenamiento ex-vivo. Se emplearon colonoscopios CF-H180AL y CF-Q180AL y procesadores Exera II (Olympus Medical System, Tokyo, Japan). Se evaluó cada pólipo en tiempo real con luz blanca y narrow band imaging. Se calculó la precisión del diagnóstico óptico (sensibilidad, especificidad, VPN, VPP), así como la concordancia entre la recomendación de seguimiento basada en diagnóstico óptico y en diagnóstico histopatológico.
Resultados: se analizaron 311 pólipos de colon < 10 mm (216 diminutos) en 195 pacientes. Precisión del diagnóstico óptico para las predicciones realizadas con alta confianza: pólipos diminutos (sensibilidad 0,59, especificidad 0,92, VPN 0,48); pólipos < 10 mm (sensibilidad 0,73, especificidad 0,88, VPN 0,50). Pudo darse una recomendación de seguimiento basada en diagnóstico óptico a 90 pacientes, coincidiendo con la recomendación tras histopatología según la guía europea en 92,2% y según la guía ESGE en 93,3%.
Conclusiones: el diagnóstico óptico permite dar una recomendación de seguimiento tras la colonoscopia. Sin embargo, en este estudio basado en práctica clínica, la precisión del diagnóstico óptico está por debajo de los estándares recomendados.
Palabras clave: Sensibilidad y especificidad. Colonoscopia. Pólipos colon. Diagnóstico óptico.
Introduction
The detection and resection of colorectal adenomas during colonoscopy reduces the risk of colorectal cancer (1). Over 90% of polyps detected during colonoscopy are small (6-9 mm) or diminutive (≤ 5 mm). The ability to correctly classify a polyp as adenomatous or non-adenomatous from its endoscopic features is known as "optical diagnostics".
Optical diagnostics is associated with several benefits. On the one hand, it can lower the costs related to colonoscopy. Also, overload of the Pathology Services can be reduced through a reduction in the number of biopsies (2). Furthermore, as fewer polyps are removed patients are less exposed to potential complications. In addition, it may serve to give an immediate recommendation on the follow-up interval to a patient with polyps, without waiting for histopathological analysis (3). To achieve these benefits in clinical practice, the American Society for Gastrointestinal Endoscopy (ASGE), through a committee established to evaluate new technologies, proposes two different strategies (4): Leave "in situ" non-adenomatous diminutive rectosigmoid polyps or "resect and discard" (DISCARD), in which all diminutive colorectal polyps are resected and discarded without the need to sent them for formal histological evaluation (2). The minimum requirements to implement these strategies are as follows: For the "leave in situ" strategy, optical diagnostics must have a negative predictive value of 90% for adenomas, provided the predictions are made with high confidence. For DISCARD strategy, a 90% agreement in the surveillance interval between optical diagnostics and histopathological diagnosis. In both cases, currently, optical diagnosis is recommended only for diminutive colon polyps (≤ 5 mm) (4).
Methodology for optical diagnosis of colorectal polyps has not been standardized. The standard white light endoscopy is not very useful to distinguish whether a colon polyp is adenomatous or hyperplastic (5,6). Magnification chromoendoscopy with Kudo pit pattern recognition allows a high diagnostic accuracy (7). However, this technique is not widely used because it is time consuming and the learning curve is steep. The new high definition equipment incorporates narrow band imaging (NBI, Olympus, Japan). NBI technology improves visualization of the mucosa and, particularly, observation of the vascular pattern (8). The advantages of NBI are its wide availability and its short learning curve (9). Several studies have demonstrated that NBI is associated with a high precision in expert hands (11-16). In a recent meta-analysis in which 28 studies were included, the overall sensitivity and specificity of NBI for the diagnosis of adenomas was 91.0% and 82.6%, respectively (16).
When implementing optical diagnosis of colon polyps in clinical practice several considerations must take into account:
- A classification scheme for distinguishing neoplastic from non-neoplastic lesions is needed. In this regard, an internationally accepted classification has been recently validated (NICE classification) (17,18) to distinguish neoplastic (NICE 1) from non-neoplastic lesions (NICE 2). The main limitation of this classification is that sessile serrated and traditional adenomas are not included.
- In studies to date, optical diagnosis provides better results in referral hospitals than in smaller centers (19).
- In most endoscopy units, the level of experience and/or competence of endoscopists is not homogeneous.
- The equipment that is available in many endoscopy units is not the same in all examination rooms.
- Studies to date have not assessed the optical diagnostics on the set of an endoscopy unit in routine clinical practice.
Therefore, the main objective of our study was to evaluate, in an endoscopy unit in daily clinical practice, the accuracy of optical diagnosis of diminutive colon polyps. Secondary objectives were the accuracy of optical diagnostics in polyps smaller than 10 mm, as well as to assess if optical diagnosis is useful for predicting future colonoscopy surveillance intervals without waiting for histopathological analysis.
Methods
Patients
This prospective study was conducted in a medium size (450 beds) academic public hospital. All patients over 18 years referred for colonoscopy were considered for inclusion. Patients were excluded if the endoscopy was performed in a room with equipment not suitable for optical diagnostics, rectosigmoidoscopy was requested, those without polyps, and those in which an obvious colon cancer was detected without simultaneous polyps. For the purposes of predicting future colonoscopy surveillance intervals, exclusion criteria were: Preparation of the colon not adequate (poor or inadequate, Aronchick scale), incomplete colonoscopy, hereditary polyposis syndromes, personal history of inflammatory bowel disease, obvious colorectal cancer detected without polyps, some polyps not resected and/or not recovered.
Written consent was requested to all patients. The study was approved by the local IRB of the Hospital General Universitario de Elche (Alicante, Spain).
Procedures
Colonoscopies were performed by five expert endoscopists. All of them had previously done more than 5,000 colonoscopies. One of them had experience in the characterization of colon polyps with NBI while the other four had not. Endoscopists were divided into two categories according to their dedication to endoscopy: Two full-time and three part-time (less than 30% of their annual working time).
Before the study, all endoscopists conducted a training period on characterization of colon polyps with NBI using the NICE classification. The training module consisted of a pre-test with 10 still images of adenomatous and hyperplastic polyps, a learning phase, in which the characteristics of 25 still images were explained by an expert and a post-test with 20 still images. All participants achieved in the post-test an accuracy of over 90% for optical diagnosis on still images.
During the study period there were 4 examination rooms in the endoscopy unit: Three of them equipped with Exera II (Olympus Medical System, Tokyo, Japan) processors and high definition monitors, and one equipped with a processor not suitable for optical diagnosis (no high definition processor). CF-H180 AL and CF-Q180 AL Olympus colonoscopes were used.
Polyp characteristics were evaluated in real time. For each polyp, endoscopists collected location, estimated size (compared to open biopsy forceps or snare sheath) and the morphology according Paris classification. One photo with NBI and another with white light were taken of all the polyps. These pictures were stored in a computerized database. The endoscopist scored the type of polyp according to the NICE classification (type 1: Hyperplastic polyp; type 2: Adenomatous polyp; type 3: Cancer with deep submucosal invasion). The confidence level for each polyp (high if polyps had one or more characteristics of a type and none of the other; lower if the features were not clear or could belong to both types) was registered. It was recommended that that the endoscopist dictate to a nurse all these parameters in real time. If possible, a recommendation for surveillance interval was recorded at the end of the procedure using the European (20) as well as the ESGE guidelines (21).
Each polyp was resected by biopsy forceps or polipectomy snare, depending on size. The polyps were then sent in a separate pot for histopathological analysis. When the pathology report was available, an independent researcher recorded this information in the data collection form, as well as follow-up interval according to the pathology report.
Two independent investigators entered the data into the computer system. Endoscopists who participated in the study were encouraged to compare the pathological diagnosis with their optical diagnosis prediction, in a continuous process of self-learning.
Histopathology
All biopsies were processed as usual. The pathologist did not know the endoscopist prediction for each polyp. The histopathological diagnosis was standardized in all cases, following the WHO classification for digestive tumors (22). For purposes of analysis, all sessile serrated and traditional adenomas were considered as non-adenomatous in this study, since the NICE classification includes them in the same category as hyperplastic polyps (type 1).
Outcome variables
The main outcomes were the sensitivity, specificity, negative predictive value, positive predictive value, likelihood ratios and diagnostic odds ratio for diminutive and small adenomatous polyps, for all predictions and for those made with high confidence. Secondary outcomes were accuracy of optical diagnosis as a function of size and location of polyps, dedication of endoscopists and type of endoscope. The correlation between optical diagnosis and pathological diagnosis when recommending a follow-up interval after colonoscopy was also calculated.
Statistical analysis
Sample size: A total of 239 polyps smaller than 10 mm needed to be prospectively assessed, assuming a sensitivity for optical diagnosis of 91% (α error 0.05; β error 0.20). Assuming that 80% of the predictions would be made with high confidence, the total number of polyps smaller than 10 mm needed was 299. This figure was increase by 5% to compensate for possible losses.
χ2 test was used to compare categorical variables, using the Fisher exact test when the value of cells was less than 5. Subgroup studies were performed to analyze the effect of the size of polyps (6-9 mm vs. ≤ 5 mm), dedication of the endoscopist (full or partial) and type of endoscope (180Q vs. 180H). The optical diagnosis based surveillance interval was compared with the histopathology based interval. A value of p < 0.05 was considered significant.
Analyses were performed with SPSS 17.0 (SPSS, Chicago, Ill) and Epidat 4.0 (Dirección Xeral de Innovación e Xestión da Saúde Pública [Xunta de Galicia]). The results of the study were reported following the recommendations for publication of studies of diagnostic accuracy (STARD).
Results
Between November 2013 and January 2014, eight hundred twenty two colonoscopies were performed in the Endoscopy Unit. Six hundred twenty seven were excluded for the following reasons: No polyps at colonoscopy 482; equipment not suitable for optical diagnostic 85; rectosigmoidoscopy requested 48; obvious cancer without concomitant polyps 12. Finally 195 patients (401 colon polyps) were included in the study (Fig. 1). Of the patients included, 55.9% were male, with a mean age of 64.0 ± 12.4 years.
Table I lists the reasons for colonoscopy. Table II shows the characteristics of polyps found during colonoscopy. Three hundred fifteen polyps were < 10 mm, but four of them could not be recovered, leaving a total of 311 polyps less than 10 mm (216 diminutive) where it was possible to compare the prediction based on optical imaging and histopathology. The pathological result of these polyps was: Adenomas 239, hyperplastic 48, serrated adenomas 8, lymphoid follicle 1, mucosa with inflammatory changes 7 and mucosa without significant changes 8. For serrated adenomas, the optical diagnostics prediction was hyperplastic in 4 cases and adenoma in the other four. All polyps with mucosal lymphoid follicle, mucosal inflammatory changes and no significant changes were predicted as hyperplastic. There were 37 polyps with advanced features (villous component and/or high-grade dysplasia), but most were lesions greater than 10 mm. Within polyps < 10 mm there were only 5 with high-grade dysplasia and 6 with villous component. In all of them the optical diagnosis prediction was adenoma.
Table III shows several parameters of the accuracy of optical imaging. For polyps smaller than 10 mm optical diagnosis properly predicted histopathology in 201/311 (71.1%), and did so in 159/239 adenomas and 60/72 hyperplastic (sensitivity 0.66, specificity 0.83). For the diminutive polyps, optical diagnostics properly predicted histopathology in 138/216 (63.9%), and did so in 85/155 adenomas and 53/61 hyperplastic (sensitivity 0.55, specificity 0.87). Predictions were made with high confidence in 238/311 (76.5%) of polyps smaller than 10 mm and 166/216 (76.9%) of diminutive polyps. Considering only the predictions made with high confidence, optical diagnostic adequately predicted 181/238 polyps smaller than 10 mm (76.1%), 131/181 adenomas and 50/57 hyperplastic (sensitivity 0.73, specificity 0.88), with a negative predictive value for adenoma 0.50 (Table III). For the diminutive polyps and high confidence prediction, optical diagnostic adequately predicted 67/114 adenomas and 44/48 hyperplastic (sensitivity 0.59, specificity 0.92) with negative predictive value for adenoma 0.48 (Table III).
Analysis by size, location, endoscopist and type of endoscope (Table IV)
The sensitivity of optical diagnosis was higher for polyps 6-9 mm polyps than for polyps ≤ 5 mm (0.88 vs. 0.55, p < 0.001). No significant differences in sensitivity were observed between rectosigmoid polyps and polyps located in the rest of the colon (0.70 vs. 0.65, p = 0.4). For the predictions made with high confidence in polyps smaller than 10 mm located in rectosigmoid, sensitivity was 0.71, specificity 0.91 and negative predictive value 0.72. Optical diagnosis showed greater sensitivity for full time endoscopists (0.68 vs. 0.57), without reaching statistical significance (p = 0.1). No significant differences in sensitivity were observed when the two types of endoscope used in the study were compared (180H vs. 180Q, 0.63 vs. 0.68, p = 0.4).
Colonoscopy surveillance intervals
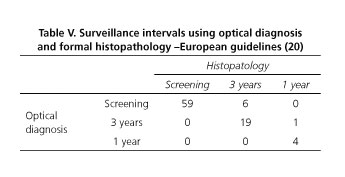
A recommendation for follow-up colonoscopy could be made on the basis of optical diagnosis in 90 of the 195 patients included in the study. A surveillance interval could not be given for the remaining patients for the reasons listed in figure 1. Surveillance intervals based on histopathology and optical diagnosis were the same for 83/90 (92.2%) patients using the European guidelines (Table V) and for 84/90 (93.3%) patients using the ESGE guidelines (Table VI).
According the recommendations of the European guidelines, seven patients had a longer interval recommended after optical diagnosis. According to the ESGE this situation occurred in 6 patients. Table VII shows a list of cases in which there was no agreement on follow-up intervals between optical diagnosis and histopatology. If we only consider patients in which all the polyps were diminutive, a recommendation for follow-up was possible in 47 cases. In this situation, surveillance intervals based on histopathology and optical diagnosis were the same for 46/47 (97.8%) for both the European and the ESGE guidelines.
Discussion
Optical diagnosis can predict histology of colon polyps without the need for histopathological analysis. This can be associated with several potential benefits: Possibility of leaving non-neoplastic polyps "in situ", resect and discard diminutive colorectalpolyps without sending them for histopathological analysis, thus saving costs (2) and the possibility of immediate feedback to the patient to recommend a follow-up interval, which is recommended by the ESGE guidelines (21). Both the ASGE guidelines, through the committee for the preservation and incorporation of endoscopic innovations of interest (PIVI) (4), as well as the ESGE (21) recommend that optical diagnosis be done by experts and only for diminutive polyps.
The results obtained in this study showed that the optical diagnosis in daily clinical practice does not meet the minimum requirements recommended by the PIVI (4). To leave "in situ" diminutive rectosigmoid hyperplastic polyps the negative predictive value, when predictions are made with high confidence, should be above 90%. In the present study it was below 90%. We also assessed the diagnostic accuracy of optical diagnosis for polyps up to 10 mm, but the results showed that for these polyps the minimum requirements are not met.
Previous studies showed that optical imaging in real time was excellent in large tertiary hospitals by expert endoscopists. Sensitivity figures were well above 90%-96% in the study by Rex et al. (14), 99% in the study by Rastogi et al. (15). However, not all studies conducted in large centers reported these figures. Thus, in the study by Rogart et al. (23) the sensitivity was 80% and specificity 81%. In the DISCARD study (2), experts endoscopists achieved a sensitivity of 96% compared with 88% of those without experience in optical diagnosis. The differences are even greater in non-academic centers (19,21). Kuiper et al. (19) reported a sensitivity of 69% for optical diagnosis based on NBI (75% for high confidence predictions). Therefore, the results of our study, conducted in a teaching hospital, are close to those reported previously in non-academic centers. Note that our study was based on the application of optical diagnostics in an endoscopy unit, including all consecutive colonoscopies and taking into account the heterogeneity in endoscopists and equipment, which represents the reality of clinical practice, unlike many previous studies in which endoscopist and equipment have been selected.
Undoubtedly, in our study, most endoscopists had made a large number of colonoscopies previously but they had no experience in characterization of colon polyps by using NBI. Although they all completed an "ex-vivo" training, it seems that this training is not enough. Previous studies reported that the characterization of colon polyps "ex-vivo" NBI showed a short learning curve, so that it could be learned in just a few minutes (9). However, the learning curve in real time does not seem so short. In a study with 4 expert endoscopists, an accuracy of 74% in the first 133 polyps was reached, increasing to 87% during the second half of the study (23). In another recent study in which 12 endoscopists with no previous experience in NBI were enrolled, considerable variation was found without a clear pattern of early learning and subsequent stabilization (24). In our study no single endoscopist characterized more than 100 polyps so it is possible that with more polyps analyzed results would be better.
Subgroup analysis showed that sensitivity was significantly higher for small polyps (5-9 mm) than for diminutive polyps (≤ 5 mm). Also, sensitivity was greater for fully dedicated endoscopists versus partially dedicated endoscopists, although without statistical significance. Surprisingly, no significant differences were observed between high definition endoscopes (180H) versus high resolution endoscopes (180Q). This finding is consistent with a recently published study in which no difference was observed in the negative predictive value for the optical diagnosis of adenomas between 180 Series with Exera II processors and 190 series with Exera III processors (25).
In our study, follow-up intervals based on optical diagnosis met the criteria proposed by the PIVI, since the correlation with pathological diagnosis was above 90%, both for diminutive polyps as if we extend the approach to polyps smaller than 10 mm. This figure is similar to that observed in previously published studies. It can be argued that optical diagnostics does not take into account histologic features, such as villous component or the degree of dysplasia, which in turn affect the follow-up interval according to the current guidelines. However, only a small percentage of small polyps have advanced features (26). In our study this percentage was 3.5%, which may explain the lack of influence of this parameter on the final prediction. One thing to note is that the percentage of patients in which a surveillance recommendation could be given after colonoscopy was less than 50%. This is because many patients had concomitant polyps exceeding the recommended size for optical diagnosis to be applied. This percentage could be improved trying to recover all polyps and ensuring that the predictions with low confidence are the least possible. In this sense, the experience of the endoscopist is essential, but also an optimum equipment (25).
In conclusion, our study based on clinical practice shows that the accuracy of optical diagnosis of colon polyps does not meet recommended standards, being lower than that obtained in controlled conditions. While the optical diagnosis can be used to give an immediate recommendation for surveillance in a percentage of patients, to implement it in all endoscopy units, several issues should be answered, such as clarifying the learning curve and why differences are observed between tertiary and other centers. Meanwhile, the optical real-time diagnosis should only be done under controlled conditions by expert endoscopists who have reached the recommended standards.
Conflict of interest
The authors declare that Javier Sola-Vera is currently collaborating with Olympus Iberia in training courses on optical diagnosis. This study has no support in the form of grants, equipment, drugs, or all of the above. The authors state that this study did not receive any funding.
References
1. Zauber AG, Winawer SJ, O'Brien MJ, et al. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N Engl J Med 2012;366:687-96. [ Links ]
2. Ignjatovic A, East JE, Suzuki N, et al. Optical diagnosis of small colorectal polyps at routine colonoscopy (Detect InSpect ChAracterise Resect and Discard; DISCARD trial): A prospective cohort study. Lancet Oncol 2009;10:1171-8. [ Links ]
3. Gupta N, Bansal A, Rao D, et al. Accuracy of in vivo optical diagnosis of colon polyp histology by narrow-band imaging in predicting colonoscopy surveillance intervals. Gastrointest Endosc 2012;75:494-502. [ Links ]
4. Rex DK, Kahi C, O'Brien M, et al. The American Society for Gastrointestinal endoscopy PIVI (Preservation and Incorporation of Valuable Endoscopic Innovations) on real-time endoscopic assessment of the histology of diminutive colorectal polyps Gastrointest Endosc 2011:73:419-22. [ Links ]
5. De Palma GD, Rega M, Masone S, et al. Conventional colonoscopy and magnified chromoendoscopy for the endoscopic histological prediction of diminutive colorectal polyps: A single operator study. World J Gastroenterol 2006;12:2402-05. [ Links ]
6. Su MY, Hsu CM, Ho YP, et al. Comparative study of conventional colonoscopy, chromoendoscopy, and narrow-band imaging systems in differential diagnosis of neoplastic and nonneoplastic colonic polyps. Am J Gastroenterol 2006;101:2711-6. [ Links ]
7. Fu KI, Sano Y, Kato S, et al. Chromoendoscopy using indigo carmine dye spraying with magnifying observation is the most reliable method for differential diagnosis between non-neoplastic and neoplastic colorectal lesions: A prospective study. Endoscopy 2004;36:1089-93. [ Links ]
8. Machida H, Sano Y, Hamamoto Y, et al. Narrow-band imaging in the diagnosis of colorectal mucosal lesions: A pilot study. Endoscopy 2004;36:1094-8. [ Links ]
9. Raghavendra M, Hewett DG, Rex DK. Differentiating adenomas from hyperplastic colorectal polyps: Narrow-band imaging can be learned in 20 minutes. Gastrointest Endosc 2010;72:572-6. [ Links ]
10. Hirata M, Tanaka S, Oka S, et al. Magnifying endoscopy with narrow band imaging for diagnosis of colorectal tumors. Gastrointest Endosc 2007;65:988-95. [ Links ]
11. Tischendorf JJ, Wasmuth HE, Koch A, et al. Value of magnifying chromoendoscopy and narrow band imaging (NBI) in classifying colorectal polyps: A prospective controlled study. Endoscopy 2007;39:1092-6. [ Links ]
12. Sano Y, Ikematsu H, Fu KI, et al. Meshed capillary vessels by use of narrow-band imaging for differential diagnosis of small colorectal polyps. Gastrointest Endosc 2009;69:278-83. [ Links ]
13. Henry ZH, Yeaton P, Shami VM, et al. Meshed capillary vessels found on narrow-band imaging without optical magnification effectively identifies colorectal neoplasia: A North American validation of the Japanese experience. Gastrointest Endosc 2010;72:118-26. [ Links ]
14. Rex DK. Narrow-band imaging without optical magnification for histologic analysis of colorectal polyps. Gastroenterology 2009;136:1174-81. [ Links ]
15. Rastogi A, Early DS, Gupta N, et al. Randomized, controlled trial of standard-definition white-light, high-definition white-light, and narrow-band imaging colonoscopy for the detection of colon polyps and prediction of polyp histology. Gastrointest Endosc 2011;74:593-602. [ Links ]
16. McGill SK, Evangelou E, Ioannidis JP, et al. Narrow band imaging to differentiate neoplastic and non-neoplastic colorectal polyps in real time: A meta-analysis of diagnostic operating characteristics. Gut 2013;62:1704-13. [ Links ]
17. Hewett DG, Kaltenbach T, Sano Y, et al. Validation of a simple classification system for endoscopic diagnosis of small colorectal polyps using narrow-band imaging. Gastroenterology 2012;143:599-607. [ Links ]
18. Hayashi N, Tanaka S, Hewett DG, et al. Endoscopic prediction of deep submucosal invasive carcinoma: Validation of the narrow-band imaging international colorectal endoscopic (NICE) classification. Gastrointest Endosc 2013;78:625-32. [ Links ]
19. Kuiper T, Marsman WA, Jansen JM, et al. Accuracy for optical diagnosis of small colorectal polyps in nonacademic settings. Clin Gastroenterol Hepatol 2012;10:1016-2017. [ Links ]
20. Atkin WS, Valori R, Kuipers EJ, et al. International Agency for Research on Cancer. European guidelines for quality assurance in colorectal cancer screening and diagnosis. 1st ed. Colonoscopic surveillance following adenoma removal. Endoscopy 2012;44(Supl. 3):SE151-63. [ Links ]
21. Hassan C, Quintero E, Dumonceau JM, et al; European Society of Gastrointestinal Endoscopy. Post-polypectomy colonoscopy surveillance: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 2013;45:842-51. [ Links ]
22. Bosman F. WHO Classification of tumours of the digestive system. Lyon France: IARC Press; 2010. [ Links ]
23. Rogart JN, Jain D, Siddiqui UD, et al. Narrow-band imaging without high magnification to differentiate polyps during real-time colonoscopy: Improvement with experience. Gastrointest Endosc 2008;68:1136-45. [ Links ]
24. Ladabaum U, Fioritto A, Mitani A, et al. Real-time optical biopsy of colon polyps with narrow band imaging in community practice does not yet meet key thresholds for clinical decisions. Gastroenterology 2013;144:81-91. [ Links ]
25. Wallace MB, Crook JE, Coe S, et al. Accuracy of in vivo colorectal polyp discrimination by using dual-focus high-definition narrow-band imaging colonoscopy. Gastrointest Endosc 2014;80:1072-87. [ Links ]
26. Gupta N, Bansal A, Rao D, et al. Prevalence of advanced histological features in diminutive and small colon polyps. Gastrointest Endosc 2012;75:1022-30. [ Links ]
![]() Correspondence:
Correspondence:
Javier Sola-Vera-Sánchez.
Endoscopy Unit.
Digestive Medicine Department.
Hospital General Universitario de Elche.
Cami de l'Almazara, 11. 03203
Elche, Alicante. Spain
e-mail:
solavera_jav@gva.es
Received: 24-11-2015
Accepted: 12-02-2015











 texto en
texto en