Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.107 no.12 Madrid dic. 2015
PICTURES IN DIGESTIVE PATHOLOGY
Duodenal gastrointestinal stromal tumor and endoscopic ultrasound
Fernando M. Castro-Poças1,2, Tarcísio P. Araújo3, Jorge D. Silva2,4, Carlos A. Lopes2,5 and Miguel M. Saraiva1,2
1 Department of Gastroenterology. Institute of CUF-ManoPH. Porto, Portugal.
2 Institute of Biomedical Sciences Abel Salazar. University of Porto. Portugal.
3 Department of Gastroenterology. Santo António Hospital. Porto Hospital Center. Porto, Portugal.
4 Department of Surgery. Santa Maria Hospital. Porto, Portugal.
5 Department of Pathology. Institute of CUF-ManoPH. Porto, Portugal
Case reports
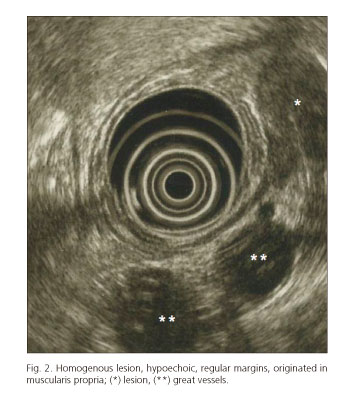
Case report 1. 73-year-old patient performed an upper endoscopy (UE) (Fig. 1), revealing a subepithelial lesion (20 mm) in the second part of the duodenum. Endoscopic ultrasound (EUS) showed a homogeneous lesion, 25x13.3 mm, hypoechoic, regular margins, originated in muscularis propria, two centimeters distal to papilla of Vater (PV) (Fig. 2). We suspected of a gastrointestinal stromal tumor (GIST). Surgery was advised. Laparoscopic excision confirmed the diagnosis.
Case report 2. 51-year-old patient underwent UE, revealing a bulge in the second part of the duodenum. EUS showed a heterogeneous lesion, 27.5x18.5 mm, hypoechoic, irregular margins, originated in muscularis propria, three centimeters distal to PV (Fig. 3). Diagnostic hypothesis was GIST, surgery being advised. The patient demanded clinical test with higher diagnostic accuracy. EUS guided fine-needle-aspiration (FNA) was performed (Fig. 4). Cytology (Fig. 5) showed spindle cells aggregates; malignant signs were not seen. This pattern suggested a mesenchymal tumor without malignancy. Low risk GIST was probable, although leiomyoma could be considered. For final diagnosis, an immunocytochemical study for CD117 and CD34 was done in a cell-block specimen that showed positivity in some cells for both. The final diagnosis was low risk GIST. Surgery was performed. Histology confirmed the diagnosis.
Discussion
GISTs in the duodenum are very rare (1). The treatment of choice is surgical resection of the tumor (2,3). Optimal surgical procedure has not yet been established (1,3,4). Surgery implies morbidity, so a definitive pre-operative diagnosis, when there is doubt in resection, is essential (4,5).
The proximity to PV seems to be an important factor affecting surgical approach (3). The precise location is imperative. We used EUS to characterize the lesions and their anatomical relations to PV, allowing a more guided surgery. In one of the cases, there was the need to perform FNA supporting the diagnostic hypothesis.
References
1. Buchs NC, Bucher P, Gervaz P, et al. Segmental duodenectomy for gastrointestinal stromal tumor of the duodenum. World J Gastroenterol 2010;16:2788-92. DOI: 10.3748/wjg.v16.i22.2788. [ Links ]
2. Bodega-Quiroga I, Tejedor-Togores P, Sáez-García MA, et al. Gastrointestinal stromal tumors (GIST): New treatment options expectations. Rev Esp Enferm Dig 2013;105:506-7. DOI: 10.4321/S1130-01082013000800016. [ Links ]
3. Kamath AS, Sarr MG, Nagorney DM, et al. Gastrointestinal stromal tumour of the duodenum: Single institution experience. World J Gastroenterol 2013;19:6000-10. [ Links ]
4. Beham A, Schaefer IM, Cameron S, et al. Duodenal GIST: A single center experience. Int J Colorectal Dis 2013;28:581-90. DOI: 10.1007/s00384-012-1432-8. [ Links ]
5. Goh BK, Chow PK, Kesavan S, et al. Outcome after surgical treatment of suspected gastrointestinal stromal tumors involving the duodenum: Is limited resection appropriate? J Surg Oncol 2008;97:388-91. [ Links ]