Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.108 no.10 Madrid oct. 2016
PICTURES IN DIGESTIVE PATHOLOGY
Acute abdomen from duodenal diverticulitis. A case report
Abdomen agudo por diverticulitis duodenal. Caso clínico
Antonio José Fernández-López, Miguel González-Valverde, Nuria Martínez-Sanz, María Encarnación Tamayo-Rodríguez and Antonio Albarracín-Marín-Blázquez
Department of General Surgery. Hospital General Universitario Reina Sofía de Murcia. Murcia, Spain
Duodenal diverticulitis is an uncommon though clinically significant complication that may be mistaken for other differently managed disorders.
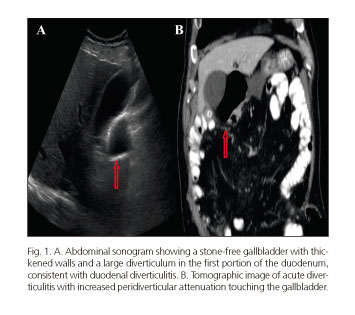
An 82-year-old male with a history of hypertension and left hemicolectomy for colonic adenocarcinoma presented with pain in the epigastrium and right hypochondrium of 12 hours duration. He had fever at 38.7 oC, and the physical examination revealed tenderness in the right hypochondrium with a positive Murphy's sign. His CBC showed 16.7 x 109 cells/L (88% neutrophils). An abdominal sonogram, supplemented with a CT scan, revealed duodenal diverticulitis around the ampulla and gallbladder inflammation by contiguity (Fig. 1).
The clinical picture remitted completely following antibiotic therapy (amoxicillin-clavulanic) for 7 days. Follow-up sonograms and CT scans showed improved diverticulitis in the absence of other intra-abdominal complications. The patient was discharged symptom-free but returned on two occasions with the same diagnosis, which led to diverticular resection and cholecystectomy. After 6 months the patient remains asymptomatic.
The duodenum is the second most common site of diverticula in the digestive tract (1-2%), after the colon (5-60%) (1-3). Most common complications include diverticulitis (20-25%), bleeding and perforation; bile obstruction and obstructive pancreatitis are more uncommon (4). Duodenal diverticulitis remains underdiagnosed because, in the absence of pathognomonic data, it is usually mistaken for other intra-abdominal conditions (4). The picture is usually associated with other gastrointestinal manifestations, hence the benefit of reduced differential diagnoses such as cholecystitis, retrocecal appendicitis, perforated duodenal ulcer, pancreatitis, pancreatic pseudocysts and neoplasms, infected enteric duplication cyst, and duodenitis from trauma or Crohn's disease (1,2). CT is the ideal diagnostic test for upper GI tract diverticula (4). Surgery is the definitive therapy with diverticulectomy or duodenal resection.
References
1. Kassir R, Boueil-Bourlier A, Baccot S, et al. Jejuno-ileal diverticulitis: Etiopathogenicity, diagnosis and management. Int J Case Reports 2015;10:151-3. DOI: 10.1016/j.ijscr.2015.03.044. [ Links ]
2. Minicis S, Antonini F, Belfori V, et al. Small bowel diverticulitis with severe anemia and abdominal pain. World J Clin Cases 2015;3:462-5. DOI: 10.12998/wjcc.v3.i5.462. [ Links ]
3. Rodríguez M, Artigas V, Trías M, et al. Enfermedad diverticular: revisión histórica y estado actual. Cir Esp 2001;70:253-60. DOI: 10.1016/S0009-739X(01)71893-3. [ Links ]
4. Schroeder TC, Hartman M, Heller M, et al. Duodenal diverticula: potential complications and common imaging pitfalls. Clin Radiol 2014:69:1072-6. DOI: 10.1016/j.crad.2014.05.103. [ Links ]











 texto en
texto en